5 professionals
BIODERMA Congress Reports EADV 2022
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Dr. Marcela Cirigliano (Dermatologist, Argentina), Dr. Marija Buljan (Dermatologist, Croatia), Dr. Nicolas Kluger (Dermatologist, Finland), Prof. Anna Zalewska (Dermatologist, Poland) and Dr. Marta Cantarero (Dermatologist, Spain)
Related topics
Speakers: Dr. Mina Kang and Dr. Martin Kassir
Report written by Dr. Marcela Cirigliano
Dr Mina Kang (Rhodes, Australia)
Dr Kang refers to the necrosis following sclerotherapy as a potentially debilitating complication with an incidence rate of 0,2 to 1,2%. The clinical presentation can range from small cutaneous ulcer to muscle necrosis and large ulcers. It may appear following intraarterial injection, which is the most feared and is uncommon with good technique, following extravasation, cited as most common in literature but rather unlikely with detergent sclerosants, and with well executed intra-venous injection. According to ulcer morphology, round or stellate, Dr Kang proposes a classification of the pathogenic mechanism.
Dr Martin Kassir (Waldorf, United States)
Cellulite is a common dermatological condition with female preponderance, affecting up to 90 % of post-puberal females. It occurs mostly in areas with greater fat storage like thighs, buttocks, and abdomen. Dr Kassir explains that it is now considered a pathological entity with systemic associations (insulin resistance, obesity, increased cardiovascular risk) and a negative psychological impact on patients.
Treatment options mentioned are several different topical treatments, noninvasive device-based and intralesional treatments and surgical modalities, but, as Dr Kassir points out, treatment remains a challenge. Regarding pathophysiology, the hypotheses Dr Kassir mention are sex specific dimorphic skin structure, alteration in the fibrous septae, vascular factors and inflammation. Histopathology shows hypertrophy and dystrophy of the adipocyte, increased fibrosis of the septae, enlargement and thickening of vascular endothelium and septal inflammation. Later stages show atrophy and dystrophy of the skin and extensive vascular damage.
Dr Kassir presents a procedure for the treatment of cellulite that consists in the creation of acoustic waves energy with laser. Q-Switch energy creates acoustic waves when it hits a target (e.g., melanin, tattoo ink) and this energy allows treatment of deeper skin structures. The carbon wave patch is a multilayered hydrogel patch embedded with carbon black, reactive with laser energy (single use).
Hydrogel is a silicone-based gel used to create solid structures (FDA class I device). Carbon black is an inert substance, that has other uses in dermatology. Dr Kassir explains that the laser energy is absorbed by the carbon patch creating the acoustic wave of energy that is contained in the multilayered aspect of the hydrogel. The acoustic waves of appropriate intensity have proved to “subcise” the fibrous septae (cellulite) He also shares a video that shows the different steps of the procedure: first places the patch onto the area to treat and then pulse laser over the patch (1064 laser system, actively Q-switched, nanosecond pulses).
Speakers: Dr. Emma Guttman-Yassky, Dr. Valeria Aoki, Dr. April W. Armstrong
Report written by Dr. Marcela Cirigliano
Dr Emma Guttman-Yassky (New York, United States)
Dr Guttman-Yassky explains that pediatric atopic dermatitis (AD) is the most common inflammatory skin disease in children (15-25% of children) that often persists into adolescence. Approximately 20% of the patients presents moderate to severe disease and still there is a large unmet need for long term disease control. AD has a complex multifactorial pathogenesis that implicates immune abnormalities (Th2 and Th2 adaptive immunity) and epidermal barrier defects leading to general inflammation.
Infants present the greatest downregulations in lipid barrier genes. AD lesions are associated with type 2 and 22 cytokine activation. Type 2 cytokines downregulate epidermal differentiation proteins in vitro and inhibit antimicrobial peptides. There is an interplay between microbioma and type 2 and 22 inflammation, with overgrowth of S.aureus that enhances skin inflammation and barrier alterations.
Type 2 inflammatory cytokines also mediate chronic itch in AD. Type 2/22 inflammatory cytokines link the skin barrier dysfunction, immune system activation and itch at all disease stages and affect a range of target organs that share pathogenic mechanisms (e.g., prurigo nodularis, chronic spontaneous urticaria, bullous pemphigoid, chronic rhinosinusitis, allergic rhinitis, asthma, eosinophilic COPD, eosinophilic esophagitis, etc).
It is comparable the Th2 activation in pediatric and adult AD. Skin homing Th2 cells were similarly up regulated in AD at all ages. The systemic Th2 upregulation in AD already starts in children. Type 2 inflammation is the predominant inflammatory pathway in blood from infancy trough adulthood. No Th1, Th22, Th17 or Th9 subset expansion was seen in blood of children with AD. Th2 axis is upregulated in lesional and non lesional skin across ages. Minimally invasive tape strips and tape- stripping analysis can be used for skin sampling and study of the cutaneous immune and barrier abnormalities in AD. Tape-strips can identify AD related biomarkers in both lesional and non lesional skin of children with early onset of the disease and may be useful for tracking therapeutic response and predicting future course and comorbidities.
Dr Valeria Aoki (São Paulo, Brazil)
Dr Aoki opens her conference mentioning the population of skin of color (SoC): African/Black, Hispanic/Latinx, Asian/Pacific Islander, American Indian/Native Alaskan, Indigenous Australian, Middle Eastern/Arabia/Northern Africa, Bi-racial/multiracial or non-White. AD is more prevalent in SoC patients (US/UK). AD incidence and persistence are higher among certain non-White racial/ethnic groups compared with non-Hispanic whites. She also presents evidence about the variations of AD immunophenotypes between European American, Asian, and African American. Regarding Filaggrin (FLG) mutations: Loss of function FLG mutation: increased risk or persistent AD in Asians, less frequent in Blacks with AD and higher in severe cases of AD in Hispanic/Latinx from Chile. Regarding skin barrier defects in SoC patients: there is evidence of a weaker barrier strength and slower recovery from barrier damage in Asians and higher dryness scores were observed in Blacks and Whites. Blacks had increased spontaneous desquamation compared to those with White and Asian skin. With respect to the forms of clinical presentation of the AD in SoC, we can observe: Nummular eczema, prurigo nodularis, erythroderma, lichenoid dermatitis, follicular dermatitis and pompholyx.
Dr Aoki presents and discusses the evidence of erythema scores that may mask severe AD in Black patients. The difficulties in the assessment due to skin pigmentation in severe cases may mean that these cases are not detected and appropriated treated. She also presents evidence published that refers that EASI has demonstrated excellent inter rater and intra-rater reliability for SoC patients and erythema perception did not contribute to inter rater variability in these populations, but patients with SoC may perceive their AD symptoms as less severe than light skin patients. Erythema in SoC patients is more violaceous or hyperpigmented so severity scores should be carefully performed considering diverse ethnicities. She also refers in the conclusions that SoC patients are still underrepresented in global clinical trials.
Dr April W. Armstrong (Los Angeles, CA, United States)
Regarding geriatric patients, Dr Armstrong presents evidence from different trials with JAK inhibitors to discuss the dose response. Geriatric Patients (≥65 y) had similar EASI 75 response to Upadacitinib 15mg or 30 mg and had similar IGA 0/1 response to Upadacitinib 15mg or 30 mg.
In the case of Abrocitinib IGA 0/1 at 12 weeks in monotherapy studies (JADE MONO-1, JADE MONO- 2) for ≥51 years was comparable to younger cohorts and regarding safety events by age groups, geriatric showed higher likelihood of low platelet count, lymphocyte count and herpes zoster with 200 mg dose.
With respect to immunocompromised patients Dr Armstrong refers that multiple case reports show Dupilumab suggest safety in patients with HIV. In two patients with HIV and AD, one had unchanged viral load and one patient had decrease by half in viral load. Dupilumab was used in a case of chronic hepatitis B on entecavir without reactivation.
Regarding adolescent patients evidence in monotherapy Upadicitinib studies, at week 16 EASI 75 rates with 15mg and 30 mg were similar between adolescents <18 years old vs adults ≥18 years old. With respect to Tralokinumab in adolescents (ECZTRA 6 trial): evidence show greater proportions of adolescents receiving tralokinumab achieved EASI 75 at 16 weeks compared to patients receiving placebo.
Speakers: Dr. Charlotte G. Mortz, Dr. Peter Schmid-Grendelmeier, Dr. Antti Ilmari Lauerma and Dr. Bernhard Homey
Report written by Dr. Marcela Cirigliano
The aspects discussed in this session were related to

 Food allergy and impact on skin disease
Food allergy and impact on skin disease
Dr Charlotte G. Mortz (Odense, Denmark)
Food allergy (IgE mediated) is a co-morbidity in AD
Dual-allergen-exposure hypothesis for the pathogenesis of food allergy: oral and skin sensitization
When we should test:
 If there is history of immediate type I reactions to food (all ages)
If there is history of immediate type I reactions to food (all ages) Infants/Children (<6years old) with persistent moderate-severe AD responding poorly on treatment: These patients have an increased risk for concomitant food allergy and should be tested to prevent a reaction during first feed of the allergenic food.
Infants/Children (<6years old) with persistent moderate-severe AD responding poorly on treatment: These patients have an increased risk for concomitant food allergy and should be tested to prevent a reaction during first feed of the allergenic food. Risk factors in childhood AD for food allergy:
Risk factors in childhood AD for food allergy:
 Increased severity of AD Persistent AD
Increased severity of AD Persistent ADRegarding sensitization in AD and controls in cohort studies: Strong and association between AD, food sensitization, and food allergy. AD of increased severity and chronicity is particularly associated with food allergy. (Tsakok T, Marrs T, Mohsin M, Baron S, du Toit G, Till S, Flohr C. Does atopic dermatitis cause food allergy? A systematic review. J Allergy Clin Immunol. 2016 Apr;137(4):1071- 1078)
Case history is crucial:
 Common food allergens that the patient has already eaten and tolerated Common potent allergen not yet consumed (geographical variations)
Common food allergens that the patient has already eaten and tolerated Common potent allergen not yet consumed (geographical variations)Testing will aim to confirm suspected allergens as being clinically relevant and allow for safe dietary expansion if other common and potent allergens not yet consumed
Dr Peter Schmid-Grendelmeier (Zurich, Switzerland)
Food allergy is very rare especially in adults.
Data supporting allergen avoidance to improve or prevent AD is sparse Most food allergies resolve during childhood
Little evidence supporting dietary interventions for the prevention of AD
Sensitization is not equal to relevant food allergy and relevance of food allergy as AD trigger Food allergy has not important effect on severity of AD in adults
Diet has no important effect on the severity of AD
(Elsawi R, Dainty K, Smith Begolka W, et al. The Multidimensional Burden of Atopic Dermatitis Among Adults: Results From a Large National Survey. JAMA Dermatol. 2022;158(8):887–892)
Avoidance of food may enhance risk of AD Food diversity reduces risk of AD
Food possibly reduces risk of food allergy Testing makes sense in children <5 years
No scenario/biomarker when to stop or restart food
Skin gut microbiome effect most probably much higher that food allergy
Dr Antti Ilmari Lauerma (Helsinki, Finland)
Evidence of therapeutic effects of probiotic Lactobaciullus rhamnosus GG in children with AD is presented ( ProPAD trial): Beneficial effects on disease severity and quality of life paralleled with a beneficial modulation of gut and skin microbiome.
(Carucci L et al. Pediatr Allergy Immunol . 2022 Aug;33(8): e13836)
Evidence of oral Administration of a Mixture of Probiotic Strains in AD patients that was effective in reducing SCORAD index and reducing the use of topical steroids in patients with moderate AD. (Navarro-Lopez V et al. JAMA Dermatol. 2018 Jan 1;154(1):37-43)
Evidence of topical Niclosamide reducing S.aureus and restoring skin microbiome diversity in AD patients,
(Weiss A et al. Clin Transl Med. 2022 May;12(5):e790) Current therapies that leverage skin microbiota are still limited
Although the efficacies of certain treatments are still controversial, the oral administration of probiotics may aid prevention of allergic diseases, including AD
More evidence is needed to standardize gut microbiota interventions. Microbial metabolites need to be tested in future trials
Dr Bernhard Homey (Düsseldorf, Germany)
Antibacterials and antibiotics control microbial colonization and infection but do not treat or clear AD lesions nor do we all develop skin inflammation due to antibiotic induced dysbiosis
Effect size of a given treatment matters
Clinical efficacy of available anti-inflammatory treatments and dynamics of microbiota during anti- inflammatory treatments:
There is evidence that Dupilumab therapy improves Stratum corneum hydration and skin dysbiosis in patients with AD: increases microbial diversity and decreases S.aureus and increases Lactobacillus spp.
(Lee SJ, et al. Allergy Asthma Immunol Res. 2021 Sep;13(5):762-775- Callewaert C et al. Journal of Investigative Dermatology (2020) 140, 191e202)
There is evidence Tralokinumab increases microbial diversity and reduces S aureus abundance in lesional skin.
(Bieber et al. E-poster Abstract#28170. Presented at the AAD VMX 2021 23-25 April 2021) Evidence that probiotics make little or no difference in improving eczema symptoms, in QoL, nor severity scores.
(Boyle RJ, Bath‐Hextall FJ, Leonardi‐Bee J, Murrell DF, Tang MLK. Probiotics for treating eczema. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD006135. DOI: 10.1002/14651858.CD006135.pub2. Accessed 09 September 2022.)
Speakers: Dr. Martin Steinhoff, Dr. Eszter Baltas and Dr. Gabriella Fabbrocini
Report written by Dr. Marcela Cirigliano
Anna Di Nardo (San Diego, United States)
Conference speaker Dr Martin Steinhoff in replacement of Dr Anna Di Nardo.
Rosacea is a chronic inflammatory skin disorder, characterized by dysregulated inflammatory infiltrate, vascular and lymphatic dilation, glandular hyperplasia and fibrotic processes, and this combination of factors reflects the multivariate process of the disease. Regarding the pathogenic mechanisms, the increased levels and activity of cathelicidin and kallikrein (KLK) in the stratum corneum, have been implicated in the pathogenesis of rosacea. It may be possible that doxycycline can inhibit activation of KLK through an indirect mechanism by inhibition of matrix metalloproteinases (MMPs) in keratinocytes and can inhibit the release of peptide LL-37 from precursor hCAP18, which is dependent on KLK activation. The number of mast cells (MC) and fibroblasts is increased in rosacea and there is an upregulation of receptors for mediators released by MC or sensory nerves, suggesting the neuroimmune and vascular interaction: neuropeptides can condition MC and turn them more susceptible to environmental triggers for rosacea inflammation. Dr Steinhoff also refers to the MFGX family, a family of G protein-coupled receptors expressed in peripheral sensory neurons, that function as itch receptors in non-histaminergic itch. MRGPRX2 is a mast cell (MC)-specific receptor that mediates non-histaminergic itch. Also, TRPV2 and TRPV4 are expressed in rosacea skin and there is evidence that LL-37 increases TRPV channel expression. MRGPRX2 activates TRPV in rosacea mast cells. TLR2 is increased in rosacea skin and its ligands may up-regulate KLK 5 in keratinocytes. Increased MC are found in all subtypes of rosacea which appear to be central to the neurogenic genesis of this condition.
Dr Eszter Baltas (Szeged, Hungary)
Dr Baltas opens her talk expressing the many challenges that dermatologists faced during the pandemic, mainly the reduction of face-to-face consultations, difficulties in the follow up of patients with chronic disease or skin cancer and monitoring of biologic and immunosuppressive treatments. Specifically referring to rosacea, she points out the increase in the severity of rosacea in relation to the use of masks and shares a multicenter, real life, telemedical and observational prospective study with 36 stable untreated rosacea patients in whom at 6 weeks of quarantine all severity scores significantly increased. Regarding the occupational dermatosis related to personal protective equipment (PPE) she mentions skin irritation (mechanical injury, irritant contact dermatitis), allergic contact dermatitis, acneiform eruptions and contact urticaria (rare). Regarding adverse skin reactions to N95 masks, Dr Baltas mentions nasal bridge scar, facial itching, skin damage and dry skin as the most frequent according to published evidence. Allergic contact dermatitis on the face from PPE may be elicited by allergens present in the elastic bands (thiuram, carbamate, N-phenyl-p-phenylendimine between others), the nose piece (nickel, aluminium, cobalt), the textiles ( polypropylene, dyes, formaldehyde) or the preservatives used in the manufacturing (bronopol, toluene-2,4-diisocyanate, between others). Due to lockdown periods, it was challenging to perform patch tests in this patients. Maskne refers to new diagnosis, appearance of lesions after 6 weeks of mask use, or aggravation of preexisting condition, mainly localized in the area of the mask or O-area. Another frequent diagnosis registered during this period was hand dermatitis.
Some measures for prevention of facial skin adverse reactions due to PPE according to the European Task Force on
 Contact Dermatitis, National Pressure Injury Advisory panel and other publications are:
Contact Dermatitis, National Pressure Injury Advisory panel and other publications are:
 Facial skin care: application of a non-comedogenic facial moisturizer before using the mask (30-60 m) and skin protective topical (silicone or dimethicone barrier cream)
Facial skin care: application of a non-comedogenic facial moisturizer before using the mask (30-60 m) and skin protective topical (silicone or dimethicone barrier cream) Treatment of underlying skin diseases
Treatment of underlying skin diseases
Dr Gabriella Fabbrocini (Naples, Italy)
Dr Fabbrocini points out three aspects to consider for the selection of the therapeutic option for rosacea
Systemic therapies currently available, in accordance with the British Association of Dermatologists guidelines for the management of people with rosacea 2021, are:
 Intermittent courses of low-dose isotretinoin in people with persistent and severe rosacea. Oral propranolol in people with rosacea where the main presenting feature is transient facial erythema(flushing)
Intermittent courses of low-dose isotretinoin in people with persistent and severe rosacea. Oral propranolol in people with rosacea where the main presenting feature is transient facial erythema(flushing)(British Journal of Dermatology (2021)185, pp725–735)
Antibiotics and antibacterials
 Low-dose doxycycline has shown to provide similar results with less adverse effects in rosacea compared with doxycycline 100 mg daily. Oral tetracycline is recommended for subtype II rosacea patients. Oral azithromycin and oral clarithromycin may also be used for this subtype, but the available evidence is stronger for the tetracyclines. Oral Metronidazol may be used for subtype II rosacea
Low-dose doxycycline has shown to provide similar results with less adverse effects in rosacea compared with doxycycline 100 mg daily. Oral tetracycline is recommended for subtype II rosacea patients. Oral azithromycin and oral clarithromycin may also be used for this subtype, but the available evidence is stronger for the tetracyclines. Oral Metronidazol may be used for subtype II rosacea Oral Zinc may be used for subtype II rosacea
Oral Zinc may be used for subtype II rosacea Minocycline not recommended any longer (rarely autoimmune hepatitis)
Minocycline not recommended any longer (rarely autoimmune hepatitis)Isotretinoin: Low dose isotretinoin treatment (0.3 mg/k) can be recommended for subtype II rosacea patients.
(Swiss S1 guideline for the treatment of rosacea)
Oral β-blokers: nonselective β-blokers can reduce flushing. Carvedilol seems to be effective in some patients. Propranolol hardly used ( hypotension and bradycardia) Nadolol seems ineffective
There is some available evidence of combination treatments that may be used in patients with severe forms or multiple rosacea features: oral anti-inflammatory dose doxycycline + topical metronidazole or topical ivermectin + oral doxycycline 40 mg modified release
Other systemic therapies in investigation: Secukinumab in moderate to severe papulopustular rosacea, Hydroxychloroquine and Erenumab.
Rifaximin: non absorbed, gut active, oral antibiotic. Eradication of SIBO with Rifaximin 400 mg 3 times daily has shown complete resolution of rosacea features in up to 78% of patients. (Weinstock LB, Steinhoff M. Rosacea and small intestinal bacterial overgrowth: prevalence and response to rifaximin. J Am Acad Dermatol. 2013 May;68(5):875-6.)
Speaker: Dr. Christopher Griffiths (Manchester, United Kingdom)
Report written by Dr. Marcela Cirigliano
The global Psoriasis Atlas (GPA), as explained by Dr Griffiths is a long-term project oriented to drive continuous improvement in the understanding of psoriasis and how it affects the patient and the society. It is a collaboration between three leading international organizations in world dermatology: International Federation of Psoriasis Associations (IFPA); International League of Dermatological Societies (ILDS); and International Psoriasis Council (IPC).
GPA vision is to ensure that people with psoriasis have access to the best available care, wherever they live in the world. All the information about this organization can be found in their website that contains data on the number of psoriasis cases in adults and children worldwide.
The site has many resources like training, statistics, the voice of the patients through their stories, scientific publications, events, annual reports, and the possibility to subscribe to receive their newsletter.
The GPA website launched on World Psoriasis Day 29/10/19: www.globalpsoriasisatlas.org
Speakers: Patrick Brunner, Mirjana Gajic-Veljic, Kim A. Papp
Report written by Dr. Marcela Cirigliano
Patrick Brunner (Vienna, Austria)
The JAK (Janus kinase)-signal transducer and activator of transcription (STAT) signaling, and spleen tyrosine kinase pathways have been implicated in AD and other autoimmune and inflammatory diseases. These proteins modulate the inflammatory process by activation of intracytoplasmic transcription factors called signal transducer and activator of transcription (STAT). Once activated, these proteins form dimers that translocate into the nucleus and modulate the expression different genes. JAK inhibition is not only restricted to systemic drugs but has also been developed as a topical treatment option. The list of JAK inhibitors with molecules already registered for AD and other indications and others under investigation is growing.
There is a relative lack of antimicrobial peptides in AD compared with psoriasis. The skin microbiome of AD is deficient in coagulase-negative Staphylococcus (CoNS) that can kill S aureus.
Bacteriotherapy with an autologous strain of skin commensal bacteria can decrease S aureus colonization and may provide an alternative treatment for patients with AD. (Nakatsuji T et al. JAMA Dermatol. 2021;157(8):978-982).
Regarding disease recurrence upon termination of immunosuppressive treatments in AD, Dr Brunner presents a study where specific immune cell populations persisted after remission with dupilumab treatment: mature dendritic cells, Th2A and Tc2 cells possibly indicative of a persisting disease memory.
A study is presented by Dr Brunner about how spontaneously resolved atopic dermatitis skin show melanocyte and immune cell activation distinct from healthy control skin. Among different cell types in spontaneously healed AD, melanocytes harbored the largest numbers of differentially expressed genes in comparison to healthy controls, with upregulation of potentially anti-inflammatory markers.
Mirjana Gajic-Veljic (Belgrade, Serbia)
Antimalarials: Especially hydroxychloroquine (HCQ are recommended as first line systemic treatment for CLE patients with widespread or severe skin lesions.
Biologics: Rituximab has shown benefit in the management of SLE but there is insufficient evidence to support use in CLE, so it has to be considered in a case basis in patients with treatment resistant CLE.
Belimumab: Insufficient evidence to support its use in people with CLE. It can be considered in people with SLE with cutaneous involvement that is refractory to conventional therapies.
New targeted therapies
New drugs for CLE and SLE
Kim A. Papp (Waterloo, Canada)
Dr Papp talks about the importance of both the target and the vehicle of the topical that must cross the skin barrier to deliver that target.
With respect to the latter, Dr Papp mentions a number of new technologies that are being investigated and developed such as nanoparticles, aptamers, cell-based carriers and nanocarriers (polymeric nanoparticles, lipidic nanoparticles, metallic and nonmetallic nano particles), virus like particles and nano particles.
 Some new Targets mentioned:
Some new Targets mentioned:
(Pap K et al. J Am Acad Dermatol. 2021 Oct;85(4):863-872.)
 (Lebwohl M, Gold LS, Strober B, Papp K A et al. N Engl J Med 2021; 385:2219-2229)
(Lebwohl M, Gold LS, Strober B, Papp K A et al. N Engl J Med 2021; 385:2219-2229)
 (Lebwohl M, Papp KA, Gold LS, Gooderham MJ, N Engl J Med 2020; 383:229-239)
(Lebwohl M, Papp KA, Gold LS, Gooderham MJ, N Engl J Med 2020; 383:229-239)
 A3AR [Piclidenoson]
A3AR [Piclidenoson]Speakers: Prof. Brigitte Dréno, Prof. Enzo Berardesca and Dr. Stéphane Fauverghe
Report written by Dr. Marcela Cirigliano
Dr Dréno explains that the skin microbiome creates a new organ in homeostasis with the environment from birth. Each newborn has its own microbiome and its profile on the skin changes during life. Skin microbiome comprises:
 Resident microbiome: commensal microorganisms in homeostasis with the skin host: S. epidermidis, C.acnes between others
Resident microbiome: commensal microorganisms in homeostasis with the skin host: S. epidermidis, C.acnes between others Transient microbiome: pathogen microorganisms from the environment that temporarily live on the skin. Streptococcus pyogenes, S. aureus, between others.
Transient microbiome: pathogen microorganisms from the environment that temporarily live on the skin. Streptococcus pyogenes, S. aureus, between others.Two commensal microorganisms play a crucial role in the pathogenesis of acne and rosacea: C.acnes and Demodex. In both cases there is an alteration of the skin barrier function that induces dysbiosis with activation of innate immunity and penetration of pathogen bacteria.
Dysbiosis in acne is not related to the proliferation of C.acnes. It is the balance of metagenomic elements that shapes the skin microbiome in acne and health. Acne is associated with C.acnes predominant phylotype IA1.This acne related strains carry virulence genes compared with healthy strains for the same phylotype IA1 that generate more porphyrins and reactive oxygen species and induce higher level of lipase activity.
This loss of diversity in skin microbiome is identified in both facial and truncal (back) acne, it activates the innate immunity with the subsequent secretion of inflammatory cytokines. IL-1β produced by keratinocytes, sebocytes and monocytes drives this inflammatory response. Restoration of the diversity of the skin microbiome suppress the inflammatory response via down regulation if the innate immunity activation.
The dysbiosis in acne would not be limited to C.Acnes, since both this and Staphylococcus epidermidis (S.epidermidis) interact, in such a way that C.Acnes inhibits the development of S.epidermidis maintaining an acidic pH in the pilosebaceous unit and through the secretion of propionic acid, and S.epidermidis inhibits the proliferation of C.acnes favoring the fermentation of the glycerol that the skin naturally produces and inducing the proliferation of succinic acid.
Dr Dréno, also refers to the relationship between cancer and microbiome. Cancer microenvironment has been recently recognized as able to modulate cancer progression and treatment response. One of these microenvironments is human microbiome: among the ~1012 distinct microbial species on earth, 11 are labeled human carcinogens or “oncomicrobes” by the International Association for Cancer Registries. These oncomicrobes cause an estimated 2,2 million cases per year (~ 13% of global cancer cases). Dr Dréno shares some published evidence on the topic:
 Melanoma and cutaneous microbiota: A commensal strain of Staphylococcus epidermidis protects against skin neoplasia by producing the molecule 6-hydroxyamino purine (6-HAP) that inhibits DNA polymerase activity
Melanoma and cutaneous microbiota: A commensal strain of Staphylococcus epidermidis protects against skin neoplasia by producing the molecule 6-hydroxyamino purine (6-HAP) that inhibits DNA polymerase activity Epithelial skin cancer and cutaneous microbiota: studies on lesional skin of patients with actinic keratosis (AK) and Squamous cell carcinoma (SCC) vs normal skin show that Staphylococcus aureus is strongly associated with both AK and SCC. S.aureus secretes a virulence peptide called modulin which induces the secretion of IL-1, IL-6 and TNFα with subsequent activation of Th17 and Tregs which release IL-17. IL-17 and IL-22 regulates de cutaneous colonization of S.aureus by triggering a self-maintenance inflammatory mechanism. Additionally S.aureus proliferation and overgrowth is associated with a high secretion of hBD-2 which could play a role in the maintenance of a state of chronic inflammation.
Epithelial skin cancer and cutaneous microbiota: studies on lesional skin of patients with actinic keratosis (AK) and Squamous cell carcinoma (SCC) vs normal skin show that Staphylococcus aureus is strongly associated with both AK and SCC. S.aureus secretes a virulence peptide called modulin which induces the secretion of IL-1, IL-6 and TNFα with subsequent activation of Th17 and Tregs which release IL-17. IL-17 and IL-22 regulates de cutaneous colonization of S.aureus by triggering a self-maintenance inflammatory mechanism. Additionally S.aureus proliferation and overgrowth is associated with a high secretion of hBD-2 which could play a role in the maintenance of a state of chronic inflammation.In her concluding remarks, Dr Dréno summarizes the 4 main roles of microbiota
 Protective role against UV radiation
Protective role against UV radiation Maintenance of the physicochemical properties of skin barrier
Maintenance of the physicochemical properties of skin barrier
Dr Berardesca opens his talk with a summary of the skin barrier function and the different barriers of protection: against physical and chemical assaults (mechanical injuries, UV radiation, allergens, irritants), antimicrobial barrier and permeability barrier, for prevention of excessive water loss and desiccation.
The environmental threats comprise: UV radiation, cigarette smoke, Ozone and UV, aldehyde formation (ozone + smoke), soot, traffic associated particles. The pollution induces skin damage, the organic compounds present in particulate matter (PM) may penetrate the skin and affect epidermal cells (keratinocytes and melanocytes) and produce oxidative stress and skin inflammation. Dr Berardesca presents published evidence of the influence of air pollution on skin ageing and as a possible risk factor for melasma and other pigmentary disorders. Other external factors relate to microplastics that may produce changes in the structure of the cell membrane and may be internalized in the cell due to their tridimensional structure, altering cell metabolism, causing oxidative stress, and inducing apoptosis.
Particulate matter (vehicles exhaust, industry emissions, cigarette smoke) produces reactive oxygen species (ROS) that in turn produce DNA damage, induction of matrix metalloproteinases (MMPs) and proinflammatory cytokines, via activation of Aryl Hydrocarbon Receptor (AhR) and mitogen-activated protein kinase (MAPK) pathway. This results in development and exacerbation of different inflammatory skin diseases.
Atopic Dermatitis presents a good barrier model to understand these interactions between environment, skin barrier and immunity, where genetic plus environmental factors induce structural and functional alterations that result in skin barrier breakdown, with increased percutaneous penetration of allergens and pollutants and impaired antimicrobial activity.
As a conclusion, Dr Berardesca points out the importance of protection of the skin barrier which is relevant in maintaining skin health but also remarks the protection of the environment which is important to accomplish these goals.
Dr Fauvergue explains through the pathogenesis of atopic dermatitis the consequences of an impaired skin barrier, basically:
 Facilitation of allergen presentation
Facilitation of allergen presentation Reduced natural moisturizing factor (NMF) linked to Fillagrin deficiency
Reduced natural moisturizing factor (NMF) linked to Fillagrin deficiency Increase of transepidermal water loss (TEWL) linked to deficiency of the hydrolipidic film and inadequate lipids ratio
Increase of transepidermal water loss (TEWL) linked to deficiency of the hydrolipidic film and inadequate lipids ratio Skin Inflammation (clinical signs)
Skin Inflammation (clinical signs) Cutaneous dysbiosis: less diversity of skin microbiome with S.aureus overgrowth
Cutaneous dysbiosis: less diversity of skin microbiome with S.aureus overgrowthEmollients are part of AD management and daily use of emollients is recommended in national and international guidelines. Used regularly they improve skin barrier function and skin hydration, reduce disease severity and the need for pharmacologic intervention.
It is important for emollients to combine clinical efficacy and safety, optimal tolerability for all skin types and adapted texture to encourage compliance. Dr Fauverghe presents results from a double- blind placebo-controlled trial in which 130 (65/65) children aged 6 months to 15 years, with moderate AD were followed for 6 months. Patients with moderate AD all received topical corticosteroids (TCS) or topical calcineurin inhibitors (TCI) in combination with a moisturizer containing ingredients such as sunflower oil, canola oil and a lipid complex of omega 3/-linolenic acid, omega 6/linolenic acid, ceramides 1, 3, 6 as well as phytosphingosine and cholesterol (Atoderm intensive baume) or the placebo emollient. Skin condition (SCORAD) significantly improved (p<0.05) in the moisturizer group compared to the placebo treated patients. Additionally, the number of flares had reduced as well as the amount of time TCS or TCI were used. He also shared evidence of in vitro reduction of S.aureus biofilm and reduction of itch and scratching in subjects with dry sensitive skin and AD patients with the use of Atoderm intensive baume.
Speakers: Ehrhardt Proksch, Vicente Navarro López
Report written by Dr. Marcela Cirigliano
Ehrhardt Proksch (Kiel, Germany)
pH in the whole body is strongly regulated and organ specific. Deviations of it may result in disease conditions. In accordance with this concept, microbiome is also specific for every organ.
The acidic mantle of the skin is responsible for its acidic pH: trans urocanic acid, Na/H pump and FFAs derived from ceramide and phospholipid metabolism collaborate with its production:
Increased pH in axilla, genital area and anus. Sebum increases scalp pH. pH is increased in newborns (pH about 6), in inflammatory skin diseases and in bacterial infections. Microbiome also shows differences according to same areas and conditions as pH.
Reducing skin pH to 5 reduces colonization with S. aureus. Topical lactic acid reduces S. aureus colonization in AD. Growth of Propionibacterium acnes is reduced by treatment with an acidic leave on product with pH=4
Dr Proksch explains that like pH, lipid composition differs between body sites and between patients with AD and healthy individuals. Staphylococcus colonization in AD skin is positively correlated with AS, ADS, NS and NDS ceramides (Emmert H, Baurecht H, Thielking F, Stölzl D, Rodriguez E, Harder I, Proksch E, Weidinger S. Stratum corneum lipidomics analysis reveals altered ceramide profile in atopic dermatitis patients across body sites with correlated changes in skin microbiome. Exp Dermatol. 2021 Oct;30(10):1398-1408.)
Staphylococcus epidermidis ferments glycerol producing short chain fatty acids, particularly lactic acid, and lactic acid inhibits the growth of pathogenic bacteria without effect on commensal bacteria. This fermentation also upregulates expression of skin barrier genes. (Salgaonkar N et al. Exp Dermatol. 2022 Sep; 31(9): 1364-1372)
Reducing skin pH may reduce disease severity in both acne and AD. Emollients with pH 8,5 or 5,5 used in patients with AD didn’t regulate greatly clinical features biophysical values and microbiome
Vicente Navarro López (Murcia, Spain)
Dr Navarro López explains the bidirectional connection between skin and gut that links skin homeostasis with gastrointestinal health.
Gastrointestinal disorders are frequently associated with skin manifestations which indicates that gut microbiome may be participating in the pathogenesis of these inflammatory disorders
Short chain fatty acids (SCFFAs) that are generated by fermentation of dietary fiber by gut microbiome demonstrate a protective effect against these inflammatory diseases like psoriasis, AD or acne.
Intestinal dysbiosis increase epithelial permeability and proinflammatory cytokines enhance this permeability inducing a condition of chronic systemic inflammation.
Probiotics influence the immune system:
 Contribute to the recovery of skin barrier function (tight junctions’ proteins) Production of SCFFAs
Contribute to the recovery of skin barrier function (tight junctions’ proteins) Production of SCFFAs Inhibition of inflammatory cytokines (IL-4, IL-17, IFNγ) and induction of anti-inflammatory cytokines (IL-10, TGFβ)
Inhibition of inflammatory cytokines (IL-4, IL-17, IFNγ) and induction of anti-inflammatory cytokines (IL-10, TGFβ)
Dr Navarro López shares evidence about the identification of bacterial DNA in peripheral blood of patients with active psoriasis, and this bactDNA was associated with increase in level of different inflammatory cytokines and identifies a subset of patients with a more severe disease. Intestinal permeability is increased in patients with psoriasis.
Dr Navarro López shares the results from a randomized, double-blind, placebo-controlled trial to determine the efficacy and safety of a probiotic mixture in the reduction of psoriasis severity (N=90). At 12-week follow-up that 66.7% of patients in the probiotic group and 41.9% in the placebo group showed a reduction in PASI up to 75% (p < 0.05) and follow-up 6 months after the end of the study showed a lower risk of relapse after the intake of the probiotic mixture. (Navarro-López V at al.
Efficacy and Safety of Oral Administration of a Mixture of Probiotic Strains in Patients with Psoriasis: A Randomized Controlled Clinical Trial. Acta Derm Venereol. 2019 Nov 1;99(12):1078-1084)
Oral administration of probiotic mixture in patients with moderate AD showed reduction in SCORAD index and the reduction in the use of topical steroids. (Navarro-López V et al. Effect of Oral Administration of a Mixture of Probiotic Strains on SCORAD Index and Use of Topical Steroids in Young Patients With Moderate Atopic Dermatitis: A Randomized Clinical Trial. JAMA Dermatol. 2018;154(1):37–43).
Some preliminary data of a randomized, double blind and placebo controlled clinical study to evaluate effectiveness of a probiotic preparation in acne patients (intermediate analysis N=40) also show improvement in the acne severity in the probiotc group.
Speakers: Robert Artur Dahmen and Prof. Henry W. Lim
Report written by Dr. Marcela Cirigliano
Robert Artur Dahmen (Zürich, Switzerland)
 Actions with topical use:
Actions with topical use:

 Inhibition of melanosome transfer
Inhibition of melanosome transfer
 Sebostatic
Sebostatic4% Niacinamide has proved to be similarly effective as 4% Hydroquinone in the treatment of melasma with less side effects and similarly effective as clindamycin gel 1% for the treatment of moderate inflammatory acne
Actions topical use:
Henry W. Lim (Grosse Pointe, MI, United States)
 Currently available filters cover UVB and short wavelength UVA
Currently available filters cover UVB and short wavelength UVA
 There is a need for agents that would protect against long wavelength UVA and visible light
There is a need for agents that would protect against long wavelength UVA and visible light

 Tinted sunscreens protect against visible light. Color match is a challenge
Tinted sunscreens protect against visible light. Color match is a challenge Filters that cover long wavelength UVA and VL:
Filters that cover long wavelength UVA and VL: Incorporation of antioxidants for improved free radical protection: 50 % of free radicals are generated by visible light
Incorporation of antioxidants for improved free radical protection: 50 % of free radicals are generated by visible light Sunscreen with photolyase, antioxidant, and peptide: repaired signs of photoaging
Sunscreen with photolyase, antioxidant, and peptide: repaired signs of photoaging Speakers: Klaus Fritz, Karim Magdi Elsharkawi, Peter Velthius, Helga van de Elzen
Report written by Dr. Marija Buljan
Klaus Fritz (Lanadau, Germany)
In this lecture, the method and indications of the microneedling were presented covering cosmetic and medical indications (fine lines, hyperpigmentations, various types of scars, stretch lines…)
For rolling scars microneedling works best - during procedure one has to remember to stretch the skin to achieve maximum results.
It is important to know and inform the patient that it takes time (up 6 weeks) to see results of microneedling. This has to be told to the patient before making a decision to perform the treatment. This method is efficient in percutaneous collagen induction therefore it treatment of choice for atrophic and contraction burn scars! It was emphasized that with microneedling better quality and function of the burned area is achieved as well as inducing repigmentation of the afected skin.
Aesthetic indications in which microneedling shows good results are fine lines, as well as age related wrinkles.
In treating stretch marks, local anaesthesia with cooling may be applied to reduce pain.
Additionaly, the usage of topical HA in sterile conditions with microneedling has shown immediate effect of refreshenig dermis and stays longer in the skin therefore gives better results in terms of skin rehydration.
Karim Magdi Elsharkawi (Frechen, Germany)
The presentation was focused on lasers in cosmetic dermatology and the use of dermoscopy
The utility of the dermoscopy in association to laser treatments was adressed on several levels:
 Pretreatment for differentiating diagnoses, treatment planing (the choice of device, planning the number of treatments);
Pretreatment for differentiating diagnoses, treatment planing (the choice of device, planning the number of treatments); Intraoperative (eg detecting whether the full pigment clearance was achieved with laser treatment of nevus or solar lentigo);
Intraoperative (eg detecting whether the full pigment clearance was achieved with laser treatment of nevus or solar lentigo); Posttreatment (eg postlaser treatment of scars where reduction or absence of vascular structures can be appreciated upon dermoscopy)
Posttreatment (eg postlaser treatment of scars where reduction or absence of vascular structures can be appreciated upon dermoscopy)In conclusion, dermoscopy should be considered as a part of routine practice in cosmetic dermatology.
Peter Velthius (Rotterdam, Netherlands)
The results of the study of Onabotulinum toxin application in patients with rosacea were presented- this treatment shows effectiveness in reduction of flushing and burning
 Up to 25 iu in total of onabotulinum toxin was applied superficially intradermally into both cheeks in areas 1 cm apart- approximatelly 30 punctures on both sides (it is rather painful)
Up to 25 iu in total of onabotulinum toxin was applied superficially intradermally into both cheeks in areas 1 cm apart- approximatelly 30 punctures on both sides (it is rather painful) Treatment is simple but the toxin should be superficially and evenly applied to treated area (very important)
Treatment is simple but the toxin should be superficially and evenly applied to treated area (very important) The results in terms of reducing flushing are good, but limited in duration
The results in terms of reducing flushing are good, but limited in durationThe effectiveness of the btx application for the treatment of pores, seborrhoic dermatitis and acne was also mentioned (the effects are due to change in the sebum secretion caused by btx)
 During discussion it was mentioned that there were cases of persistent blanching areas on the face caused by this treatment described
During discussion it was mentioned that there were cases of persistent blanching areas on the face caused by this treatment described
Helga van de Elzen (Naarden, Netherlands)
Dr van de Elzen discussed the complexity of possible situations that doctors may encounter when practicing aesthetic medicine due to psychological traits of (large part of) clients who are in demand for cosmetic procedure. These clients often bring with them both, “YES” and “NO” list regarding what they want or don’t want from aesthetic procedure and they often think that multiple corrections they potentially could have, should be performed with one or (max) two syringes of filler (?!).
Listening to our clients and recognizing their needs, as well as making them realize what could be achieved (and acting according to that) is crucial.
I find that most important message from this lecture is: “It does not matter how you look but how you feel!”
Speakers: Aimilios Lallas, Claudio Conforti, Gabriella Brancaccio, Bengu Nisa Akay, Chrysoula Papageorgiou, Sebastian Podlipnik
Report written by Dr. Marija Buljan
Aimilios Lallas (Thessaloniki, Greece), President of the IDS
A. Lallas gave the audience updates on the last 20 years of the history of dermoscopy and IDE adressing the highlights of the period from 2000 to 2020 during which dermoscopy became extremely developed, popular and implemented wolrdwide and, dermoscope became a sthetoscope for dermatologist.
IDS counts today 20000 members (!!) and now the validation of the membership will be asked from the members to provide info on the number of active members.
 Also, the areas where dermoscopy played an important role were pointed out;
Also, the areas where dermoscopy played an important role were pointed out;

 Reduced number of unnecessary biopsies
Reduced number of unnecessary biopsies  Dermoscopy Practical and Conceptual, an official journal of the IDS achieved IF of 2,75 in 2021, great news!
Dermoscopy Practical and Conceptual, an official journal of the IDS achieved IF of 2,75 in 2021, great news!
Claudio Conforti (Trieste, Italy)
Talked about the importance and use of inflammoscopy
IDS published concensus on inflammoscopy defining 5 main structures in analysing inflammatory dermatoses- blood vessels, folicular findings, scales, other structures, specific clues.
IDS also published a paper on dermoscopy of mycosis fungoides defining dermoscopic criteria of various types of MF including rare subtypes which may be challenging to diagnose (follicular, erythrodermic, poikilodermatous MF)
Gabriella Brancaccio (Naples, Italy)
Gave an overview of the most successful papers on melanoma published in the last year
One of the clinically important features described are those that might give a clue on the potential aggressiveness/level of invasion (in situ or <1mm thickness or >1 mm thickness).
The study on tiny pigmented melanomas (<5 mm diameter) -starburst pattern was the most frequent feature of these tiny pigmented melanomas.
SDDI dermoscopic changes - nevi vs melanoma- a paper on The long term evolution of nevi in adult population.
Bengu Nisa Akay (Ankara, Turkey)
Where the difficulties in differentiating bcc from desmoplastic trichoepithelioma were adressed (in bcc more commonly founf DS features are ulceration, pink white and yellow structures).
However, dermoscopic features are overlaping in these two groups of tukours thetefore biopsy and phd remains gold standard in ddg of bcc and trichoblastic tumours.
Chrysoula Papageorgiou (Thesaloniki, Greece)
A study on mucoscopy of lip scc (these type of studies are rare) was mentioned- no new DS features were described (lip scc shares the same features as scc on other body areas) (Jha AK et co. Indian J Derm 2021)
Regarding other papers on dermoscopy of SCC, one of the important facts one needs to think about is that in SCC spectrum of tumours dermoscopic features vary according to the degree of histological differentiation- therefore:
 In well differentiated scc DS features are: white yellow background and white yellow perifollicular halo
In well differentiated scc DS features are: white yellow background and white yellow perifollicular halo In moderately differentiated scc DS features are: pink background
In moderately differentiated scc DS features are: pink background In poorly differentiated scc DS features are: red background and densly distributed blood vessels occupying >50% of lesion
In poorly differentiated scc DS features are: red background and densly distributed blood vessels occupying >50% of lesion
Sebastian Podlipnik (Barcelona, Spain)
Nowadays, many studies confirmed that good quality AI-based support of clinical decision- making improves diagnostic accuracy over that of either AI or phisicians alone
One of the most important things today is to standardize the AI evaluation.
Speakers: Prof. Henry W. Lim, Prof. Thierry Passeron and Dr. Stephane Fauverghe
Report written by Dr. Marija Buljan
Introduction in photobiological effects of sunlight.
Some of the important updates given:
 Blue light induces sustained tyrosinase activity.
Blue light induces sustained tyrosinase activity.
 New data- effects of tinted sunscreen were adressed
New data- effects of tinted sunscreen were adressed  New data - the use of sunscreens for different phototypes was adressed and a recent study on artificial intelligence analysis and recommendations was presented (Flamment et co, JEADV 2022).
New data - the use of sunscreens for different phototypes was adressed and a recent study on artificial intelligence analysis and recommendations was presented (Flamment et co, JEADV 2022).
The question with which this presentation started was: “Can we protect our skin from visible light?”
The presenter gave an overview of the recommendations to assess visible light protection of sunscreens emphasizing that the methods based on ROS should not be used to assess the protection effects against VL- induced hyperpigmentation.
In vitro pigmentation protection factor (PPF) based on transmission reduction of visible light appears to be the most adequate in vitro method for topical formulation and, in vivo models should be considered the gold standard.
 As take home messages the following was emphasized:
As take home messages the following was emphasized:
 Transmittance measurements between 400 to 469 nm is a good way to predict the protection against visible light- induced pigmentation
Transmittance measurements between 400 to 469 nm is a good way to predict the protection against visible light- induced pigmentation PVL-PR is an easy way to know the protective properties of sunscreen against VL.
PVL-PR is an easy way to know the protective properties of sunscreen against VL.Therefore, it is possible to protect the skin from visible light and this can be measured.
Introduced an innovative solution against hyperpigmentations- PHOTODERM M bluelight protection 66 - clarifying gel-cream as a patented innovation.
This product provides sun active defense based on SPF 50+, as well as blue light protection based on high pigment concentration (10.7.%), iron oxide, blocking 61-66% of blue light.
It is efficient in the prevention of development and recurrences of hyperpigmentations such as pregnancy mask.
Speakers: Iris Zalaudek, Danica Tiodorovic and Monika Arenbergerova
Report written by Dr. Marija Buljan
Globules at the periphery are seen in pregnancy but also on convex parts of the body- the explanation is junctional nests of melanocytes (growing nevi)
During pregnancy DS changes in nevi include:
 Color changes (darker during pregnancy and lightening postpartum)
Color changes (darker during pregnancy and lightening postpartum) Thickening of the network and Development of new globules are the most common features Increased vascularization
Thickening of the network and Development of new globules are the most common features Increased vascularization Most changes disappear 3-6 months postpartum
Most changes disappear 3-6 months postpartumDuring pregnancy if you see globules - a short term follow up is recommended - after 1 month, and then decision on further follow up or excision (to see if this lesion is growing symmetrically so we can follow or asymmetrically and then excise)
Pregnant women- when to worry? - the same as in non-pregnant woman!
Worrisome!!! Are black globules- correspond to very thick and proliferating melanocytes at the dermo epidermal junction.
Criteria for growing melanomas were adressed in the lecture.
The life cycle of melanocytic nevi is a complex and dynamic process that can be affected by various endogenous and exogenous factors.
Dermoscopic features of nevus involution:
 Fading of nevi and/or decrease in size (apoptosis or transapidermal elimination of melanocytes) Granularity, scar-like areas, blue white structures
Fading of nevi and/or decrease in size (apoptosis or transapidermal elimination of melanocytes) Granularity, scar-like areas, blue white structures Halo nevi
Halo nevi Whitening of the nevi
Whitening of the neviInvolution and fading of nevi can be seen in pediatric population, too (most commonly in form of halo nevi or fading).
Spitz nevi may involute spontaneously- often.
This is why we usually don’t find Spitz nevi in adults.
Dysplastic nevi may involute, too- especially in patients with Sy ND. Nevi in patients with autoimmune diseases may also involute.
But one should remember that …Melanoma may completely regress, too..
There are three groups of causes associated to delay in prognosis of melanoma in elderly: (Lasithiotakis et al.):
 LMM in the elderly - LMM is typical type of melanoma of the elderly population and makes 4-15% of all melanomas and has a rising incidence
LMM in the elderly - LMM is typical type of melanoma of the elderly population and makes 4-15% of all melanomas and has a rising incidence Nodular melanoma in the elderly - No difference in the DS aspects in comparison to other age groups
Nodular melanoma in the elderly - No difference in the DS aspects in comparison to other age groups Remember black blue rule for NM! Vulvar melanoma in the elderly
Remember black blue rule for NM! Vulvar melanoma in the elderly Ring like pattern?? and hyperpigmentations Palpable, solitary lesion
Ring like pattern?? and hyperpigmentations Palpable, solitary lesionSpecific features of elderly skin
commonly there are multiple skin cancers in the same patient….
Also, a lower rate of SLN positivity in elderly patients is registered which influences the therapeutic approach in the treatment of elderly melanoma patients.
Speakers: Giuseppe Argenziano, Nicole Ariana Kukutsch, Elvira Moscarella and Bengu Nisa Akay
Report written by Dr. Marija Buljan
 Differential diagnosis of pink tumours includes a variety of benign and malignant lesions:
Differential diagnosis of pink tumours includes a variety of benign and malignant lesions:
 Malignant- scc, bcc, melanoma and rare entities like Merkel cell cai
Malignant- scc, bcc, melanoma and rare entities like Merkel cell caiThere are 3 simple rules for diagnosis of pink lesions:
Three most common tumors are: bcc, scc, mm (The “three musketeers” among pink tm)
Prof. Argenziano emphasized that there will always be “difficult to diagnose lesions” and we cannot change that regardless the experience and knowledge, HOWEVER it is acceptable as long as we have the management strategy and as long as we recognize that we are facing something that should be excised.
In conclusion:
 Pink tm are the most difficult lesions thus RULES must be followed!
Pink tm are the most difficult lesions thus RULES must be followed! Morphology and not history is important and a lesion must be excised when diagnosis is not certain!
Morphology and not history is important and a lesion must be excised when diagnosis is not certain! Always combine clinical and dermoscopic features in pink lesions!
Always combine clinical and dermoscopic features in pink lesions!
Differential diagnosis of blue lesions includes variety of benign and malignant lesions:
 Benign: Blue nevus/Reed nevus, seb k, vascular lesions (angioma, angiokeratoma, pyogenic granuloma, hemorrhage), hydrocystoma, tattoo fibers)
Benign: Blue nevus/Reed nevus, seb k, vascular lesions (angioma, angiokeratoma, pyogenic granuloma, hemorrhage), hydrocystoma, tattoo fibers) Malignant: Nodular melanoma/melanoma metastatsis, angiosarcoma/kaposi sarcoma, pigmented bcc
Malignant: Nodular melanoma/melanoma metastatsis, angiosarcoma/kaposi sarcoma, pigmented bcc Blue black rule for diagnosis of nodular melanoma was emphasized- blue black color in more that 10% of lesion, and if angioma/seb k are excluded- excise the lesion to rule out nodular melanoma!
Blue black rule for diagnosis of nodular melanoma was emphasized- blue black color in more that 10% of lesion, and if angioma/seb k are excluded- excise the lesion to rule out nodular melanoma!(BB Rule: Absence of features of seb k or angioma + presence of irregular globules/blotches=nodular melanoma!)
According to a study by Lallas et al.(Dermatology 2022), probability of malignancy increases when there are:
 Blue color in clods
Blue color in clods Blue color asymmetrically distributed
Blue color asymmetrically distributed AND
 Probability of benign lesion increases when there is:
Probability of benign lesion increases when there is:

 Blue color in more than 75% of the surface
Blue color in more than 75% of the surface Also, melanomas are generally dermoscopically “more chaotic” than blue nevus/combined blue nevus.
Reed nevus may also be bluish and there are guidelines from 2017 on management of Spitzoid lesions.
Pigm. Bcc dermoscopic features were also adressed (bcc is an important simulator of melanoma). In the discussion, prof. Argenziano emphasized that, just like with pink lesions, NO follow up for blue lesions if it is not certain that the lesion is benign!
Black lesions differentially include various benign and malignant lesions;
Benign: trombosed angioma, nevus Reed, heavily pigmented seb k, hyperpigmented nevus(!) Malignant: melanoma- thin or invasive
Black nevi are more common in darker skin types.
Ddg of black nevus is thin early melanoma- melanoma is asymmetric - black blotch is eccentrically located whereas in nevus it is symmetric (centrally located black area).
Recently (Lallas et al) Irregular hyperpigmented areas were described as a feature of early melanoma (MIS).
The difference between streaks (in melanocytic lesions) and fat fingers (seb k) was addressed.
This topic is becoming very popular in the last years and up to date there are not so many studies reporting on dermoscopy of coloured skin.
The reason why dermoscopy of dark skin is different than the fair skin - melanosomes in dark skin are bigger, homogeneous and produce more melanin whereas in fair skin- melanocytes are less active and clustered and produce less pigment, feomelanin. Additionally, lability of pigment, and sclerotic reactions are more common in dark skin which reflects on dermoscopic features.
Multiple, very interesting cases of dark skin lesions vere presented (clinically and dermoscopically) in this presentation:

 Ashy dermatosis- perifoll. pigmentation
Ashy dermatosis- perifoll. pigmentation  Facial discoid lupus erythematosus
Facial discoid lupus erythematosus Riehl melanosis (pigmented contact dermatitis)
Riehl melanosis (pigmented contact dermatitis)
 Sarcoidosis (vessels are less focused in darker skin but orange colour is a good clue)
Sarcoidosis (vessels are less focused in darker skin but orange colour is a good clue)
 Pityriasis rosea (background is lighter but the peripheral jagged rim of scales are the same)
Pityriasis rosea (background is lighter but the peripheral jagged rim of scales are the same)  Vitiligo in dark skin patient
Vitiligo in dark skin patient
 Hypomelanosis idiopatica guttata vs vitiligo (in vitiligo hairs are depigmented, too)
Hypomelanosis idiopatica guttata vs vitiligo (in vitiligo hairs are depigmented, too)The colour of the scale also differs according to the skin type; eg. Darrier disease (in darker skin types we dont see typical yellow scales)! Interestingly, in solar lentigo and seb k in dark skin- perifollicular grey circles are common!
Pigmented Bowen disease- the same
SCC- pigmented variants are more common!
Dermatofibroma- purple coloration is more commonly encountered in dermoscopy of dermatofibroma in dark skin
Kaposi sarcoma- very colorful in dark skin!
Speakers: Aimilios Lallas, Luc Thomas, Wilhelm Stoltz and Caterina Longo
Report written by Dr. Marija Buljan
Lallas proposed 7 step procedure for the evaluation of pigmented nail lesions;
Exclude hemorrhage (Red color, sharp border, not arising from the proximal nail fold, Periphery is very characteristic- blood spot and lines at the periphery)
However, male sure there is not smt else coexisting with hemorrhage! (Scc, mm…) age matters!!!
In children everything is benign (congenital nail matrix nevus) When do we worry in children? Never!
Until 30 yrs of age it looks like every nail/acral pigmentation is benign… Other nails invoved?
One nail involved- local cause
More than one nail involved- systemic reason for nail discoloration more probable
Decide whether melanonychia is due to melanocytic proliferation (brown) or melanocytic activation (grey)?
If it is melanocytic (brown) what is the size of the lesion?? In adults size is important-large is suspicious!
However…Nothing is large before being small and becoming large;) Is the line regular (benign) or irregular (melanoma)??
**Micro-Huthinson sign- pay attention to possible traces of pigment periungually and may be seen upon dermoscopy only!
Follow up or follow back? Follow back meaning one can analyse how the lesion was developing by looking at the lesion.
In conclusion, 7 steps to evaluate nail lesions are:
Prof. Luc Thomas is one of the most distinguished experts in the field od acral lesions (diagnosis and treatment) and, as always, he gave a splendid lecture on acral regions.
First, he explained the anatomical reasons of the peculiar dermoscopic patterns of acral lesions. Furthermore, he explained and gave an overview of all variants of possible patterns of melanocytic lesions on the acral skin (benign and malignant patterns and exceptions to the rules as well).
Index of protection of nail is around 80 so no one gets sunburn of the nail bed, therefore UV is not involved in the etiology of ALM. (Nail lacquer - uv protection- not necessary)
Prof Stoltz explained anatomical anatomical reasons for specific dermoscopic features seen on the face
He also gave an overview of dermoscopic features of facial lesions.
Practically, when analyzing facial lesions, one should be able to differentiate between the following entities:

 Flat seborrhoic keratosis/lentigo senilis/lentigo solaris
Flat seborrhoic keratosis/lentigo senilis/lentigo solaris
 Pigmented bcc
Pigmented bccBut also other types of melanoma may develop on the face
One of the most difficult differential dg of LM is pigm AK; lentigo maligna has normal follicles and grey circles around it and, in pAK follicles are yellow and filled with keratine with no pigm circles around.
Algortithm for facial lesions by Stoltz was presented:

 Evaluation of classic features of solar lentigo (parallel lines, moth eaten borders, jelly sign)
Evaluation of classic features of solar lentigo (parallel lines, moth eaten borders, jelly sign) Pigmented AK has scaly surface
Pigmented AK has scaly surface
 If these features are not present, consider carefully biopsy or close follow up
If these features are not present, consider carefully biopsy or close follow upAlso, a new approach to dg LM/AK/solar lentigo was mentioned (published recently by Lallas and Argenziano).
Mucosal lesions can be divided into pigmeted and nonpiebted and are numerous. In the lecture, the most frequent entities and their dermoscopic patterns were discussed- Melanoma- Nevus- Melanosis.
Remember! The ABCD rule does not work for flat lesions on mucosa Melanosis- usually multiple and in younger population than melanoma
Thin vulvar melanoma are rare 😞
3 scc cases
Authors: Nika F et al., Ariasi C et al., Rogowska P, et al.
Report written by Dr. Nicolas Kluger
Nika F et al. Flat warts confirmed to the black pigment of a tattoo: a rare tattoo-associated complication. P1139
Nika et al from Zagreb reported the case of a 43-year-old patient who developed multiple asymptomatic verrucous papules restricted to one 15-year-ol black tattoo on the lower leg. He had no other symptoms and only one tattoo was affected. All the other tattoos have been spared. Punch skin biopsy confirmed the diagnostic of verruca plana within a tattoo. No HPV typing had been performed. Warts were treated by curettage without any scars. This case is a reminder that warts can develop even years after a tattoo has been performed. Tattoos could act as a nitidus for warts reactivation.
Ariasi C et al. Role in dermatology of non-invasive tools for the diagnostic of tattoo pseudolymphoma: potentiality of confocal microscopy and optical coherence tomography. P0936
The team from Brescia has used reflectance confocal, icroscopy and line-filed confocal optical coherence tomography to analyse five tattoo reactions, pseudolymphoma type. They showed that it could be a potential useful tool in the diagnostic of tattoo pseudolympohoma; to identify the most representative area for biopsy especially. In the future, such non-invasive tools may prevent from taking biopsies for diagnostic purposes.
Rogowska P, et al. A multi-center study of tattoo-associated granulomatous reactions. P1287
A multicentric retrospective study from Poland and Finland reviewed the cases of granulomatous tattoo reactions in 26 patients. In 23% of the cases, systemic sarcoidosis has been diagnosed.
Granulomas affected mainly black color (81% of cases), on the extremities (81%), with a papulo- nodular pattern (77%). Lesions were itchy or painful in half of the cases. Granulomatous tattoo reactions are not uncommon reactions that can sometimes disclose systemic sarcoidosis.
Author: Cuenca-Barrals C, et al.
Report written by Dr. Nicolas Kluger
Cuenca-Barrals C, et al. Impact of hidradenitis suppurativa on quality of life and sexual function of patients’ partners. P0008
Hidradenitis suppurativa (HS) has a non-negligeable impact on the quality of life (QoL) of the patients. A multicentric cross sectional study aimes to explore QoL and sexual function of patients’s partners and the factors associated with their impairement and to compare the QoL and sexual function of single patients versus those in a relationship. This was a small study that included 34 single patients and 28 patients in a stable heterosexual relationship. Body mass index, disease duration, Hurley stages and IHS4 scores were comparable. Single patients were younger than patients in a stable relationship. The proportion of erectile sexual dysfunction was similar in both group (63% of men) while the proportion of women reporting sexual dysfunction was higher among single women (46.7% vs 35.3%). Among the partners, men reported sexual dysfunction (58.8%) while only 9% of the women reported sexual dysfunction. The poster failed unfortunately to report any statistical analysis and no information about the location of HS has been given. HS affects not only the sexuality of the patients but also the sex life of their partners. This factor has to be taken into account when managing the patients.
Author: Soto-Garcia D, et al.
Report written by Dr. Nicolas Kluger
Soto-Garcia D, et al. Prevalence of dermatological self-treatment among medical doctors of a tertiary Spanish hospital. P1698
Self-medication is frequent among doctors. The authors tried to assess the prevalence of self- treatment for skin diseases among medical doctors. The study was a questioned based survey completed by 283 physicians (women 62%, mean age 43 y). 77% treated themselves for diseases other than those of their own pathology et 55% used self-treatment for dermatological conditions. Conditions in most of the cases were of acute duration <1 month, 63%) and on visible areas (44%). Corticosteroids ointments were the most frequently used (69%) followed by anti-fungal treatments (47%) and local antibiotics (21%). Fungal infection was the first identified skin condition (20.5% of cases), followed by bacterial infections (14%) and atopic dermatitis (9%). The skin problem was cured in 95%. In only 16% of the cases in which a consultation with the dermatologist was required, the dermatologist indicated that the self-administered treatment was correct. The physicians who self- administered a treatment were older than those who did not. The limitations of the studies include the self-reporte nature of the data, especially diagnosis may be erroneous. Besides, the study does not specify the specialities of the respondents or the strength of corticosteroid used.
To conclude; physicians are used to self-treat in case of recent cutaneous diseases. Fortunately, in most of the cases, the lesions resolved at the end of the treatment!
Authors: Freeman E. and Catala A.
Report written by Dr. Nicolas Kluger
D3R04.2C Freeman E. Skin manifestations in COVID-19 “long haulers”
D3R04.2D Catala A. Long term sequelae of COVID-19
The term “Long COVID” was introduced in May 2020 and several other terms have been used such as Post-acute COVID, post-COVID, COVID Long Haulers, Chronic COVID or Persistent COVID. The current accepted term since October 2021 is “Post COVID-19 condition”.
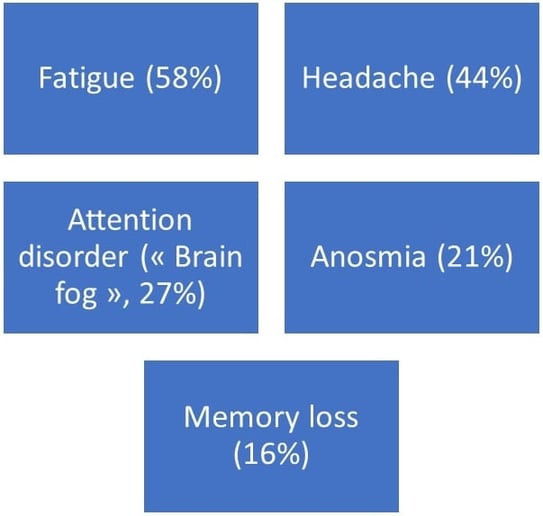
According to WHO, post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 and that last for at least 2 months and cannot be explained by an alternative diagnosis. Symptoms can persist from the initial illness or be new onset, after initial recovery. They can fluctuate and wax-and-wane. There is a myriad of symptoms that have been reported by patients (Figure 2). There are no minimum symptoms you need to read to be diagnosed with “Long COVID”. Long term manifestations and their severity varies according to acute infection symptoms, vaccination status and variants that has infected the host. Individuals that are at-risk of long COVID include: advanced age; women; patients from ethnic minorities; socioeconomic deprivation; smoking; severe acute infection (intensive care) and those who had multisystemic inflammatory syndrome during or after COVID-19; underlying comorbidities; non vaccinated patients. Vaccination clearly diminishes the risk of long COVID from 15 to 50%.
The physiopathogeny of long COVID-1) remains unknown. Current hypotheses include: sequelae of COVID-19 organ during acute infection; virus in several potential tissue reservoirs; delay viral clearance due to immune exhaustion resulting in chronic inflammation and impaired tissue repair; cross-reactivity of SARS-CoV2 and alterations of microbiome.
Is there dermatologic manifestations that are related to long COVID? Most of the cutaneous manifestations last about 7 to 12 days.
Hair loss has been a well reported complication after COVID-19. It is associated with disease lenght and inflammatory sympto ms (fever, dyspnea, myalgia) and develops mostly within the first 3 months after COVID-19. Trichodynia is not infrequent.
A very small proportion of patients may present with pernio/chilblains like lesions, sometimes papulosquamous/psoriasiform for more than two months. In a study in the UK based on self-reported symptoms on an App associated with COVID-19 testing (UK ZOE COVID Study App), authors could show that the cutaneous manifestations were different according to the variants (delta vs omicron).
Omicron variant was clearly less responsible for cutaneous manifestations of any kind compared to the Delta variant. Omicron and Delta variants are also responsible for different other COVID-19 manifestations but Omicron is also less responsible form long COVID-19 compared to Delta. The question whether we may see less cutaneous long COVID manifestations remain open. It should be kept in mind that Omicron is more contagious so that if more individuals are infected, the total number of people with long-COVID may increase.
Lastly, Ester Freeman put emphasis on cases of chronic spontaneous urticaria after COVID-19 vaccination usually after the third vaccination and booster dose. Those patients in her experience usually need systemic therapies like omalizumab.
Author: Fiorillo L, et al.
Report written by Dr. Nicolas Kluger
Fiorillo L, et al. Efficacy and safety of Apremilast in paediatric patients with moderate to severe plaque psoriasis: 16-week results from a Phase 3, randomised, double-blind, placebo-controlled study. D1T101.3E
Apremilast (APR) is a phosphodiesterase-4 inhibitor. The SPROUT study was a 16-week-long randomised, double-blind, placebo-controlled (1:2 randomisation) study that assessed the efficacy of APR after 16 weeks in children aged six to 17 years with moderate to severe psoriasis who had not responded to topical treatments. The dose of APR was 20 mg twice daily, if the child’s body weight was > 20 kg and < 50 kg, and 30 mg twice daily for a body weight > 50 kg. The study’s primary endpoint was efficacy at 16 weeks as determined by a PGA score of 0-1; its secondary endpoint was achieving PASI-75 at W16. In total, out of 245 children included, 221 completed the 16 weeks of treatment. At W16, a PGA score of 0-1 was achieved for 33.1% vs 11.5% (p<0.0001).
PASI-75 was achieved for 45% of subjects in the APR group vs 16% of those in the placebo group (p<0.0001). Age and body weight did not affect the efficacy of treatment, as determined by the PGA score and PASI-75. The side effects occurring during treatment with APR are well known: 20% of children experience diarrhoea, nausea and vomiting, and 10% present with headaches. Few treatment options are available for children with psoriasis. Oral APR has some short-term efficacy for this indication but with known side effects.
Author: O’Connor C, et al.
Report written by Dr. Nicolas Kluger
O’Connor C, et al. Spotting fake news: a qualitative review of misinformation and conspiracy theories in acne vulgaris. P0096
Dermatologists from Ireland have reviewed the various type of misinformation and conspiracy theories that can be found on various social medias, such as TikTok, Twitter, Facebook or Instragram. These are summarized on the Figure below. The psychological impact of acne on teenagers makes them particularly vulnerable to misinformation on the Internet and on social medias. Dermatologists should be prepared to discuss such misleading health information during the consultation.
Figure. Various forms of misinformation and conspiracy theories on social medias
Author: Yale M.
Report written by Dr. Nicolas Kluger
Yale M. Patient involvement in care and treatment D1T08.4B
Marc Yale is a patient who suffers from mucous pemphigoid. He shared his experience as a patient and relationship with physicians and dermatologists.
The patients’ experience is not limited to the patient – doctor encounter during the consultation. It includes:

 Ease of making an appointment
Ease of making an appointment Wait time
Wait time

 Active listening by clinician
Active listening by clinician
 Good communication is the key
Good communication is the key

 Better understanding competence and willing to participate
Better understanding competence and willing to participate Care plan compliance
Care plan compliance

 Providers, patients, and their families are partners
Providers, patients, and their families are partners  Use clear and simple language when educating patients
Use clear and simple language when educating patients  Acknowledge the individuals as an expert in their own care
Acknowledge the individuals as an expert in their own care Author: Nowak M, et al.
Report written by Dr. Nicolas Kluger
Nowak M, et al. Skin hypersensitivity reactions to herbal remedies and dietary supplements. Case series. P0111
Dietary supplements and natural remedies are widely advertised in the medias and social networks. However, they are not regulated as medications but can be responsible for skin reactions. Dermatologists from Gdansk is Poland reported a series of 5 patients (4 women) that developed various reactions such as maculo-papular rash; erythema multiforme; urticaria or photoreaction after either oral intake; local injection or local application of a therapeutic. For instance, one used a cocktail of pills containing kale, spirula, bee pollen, Chinese skullcap, selenium and vitamins; others “detox” pill or energy drink. Patients were treated by antihistamines; IV or oral corticosteroids. Unfortunately, the poster lacks additional informations such allergological explorations or blood tests. This poster acts as a reminder that natural remedies and dietary supplements can be responsible for “drug induced” rash and should always searched after when taking anamnesis.
Speakers: Prof. Henry W. Lim and Prof. Thierry Passeron
Report written by Dr. Nicolas Kluger
Ultraviolet radiation and visible light (VL) both have biologic effects on the skin. VL can induce erythema in light-skinned individuals and pigmentation in dark-skinned individuals. Reasons for the tendency for such hyperpigmentation are related to several characteristics of the skin pigmentation in individuals with dark skin phototype. Indeed, the melanosomes are larger, more melanized and distributed individually within the keratinocytes rather than in aggregates. Melanin can filter 2 to 5 times more UV than melanin in light skinned individuals. Their epidermis has an intrinsinc sun protection factor of 13.4 versus 3.3 in light phototypes. Regarding sun light, 50% is composed of
VL (400-700 nm) and 5% only of UV (280-400 nm). The higher the wavelength, the deeper it penetrates in the skin. Thus, VL can reach the dermis and generate free radicals in the skin. As a matter of 50% of free radicals generated by sunlight and induced by VL. In Dark-skin, VL is responsible for a persistent hyperpigmentation. This hyperpigmentation induced by VL is only observed in darker skin and not in light phototype and develop in association with UVA-1. On biological level, Opsin 3 is the key sensor in melanocytes responsible for hyperpigmentation induced by the shorter wavelengths of VL. It leads to the increase of the melanogenesis enzymes: tyrosinase and dopachrome tautomerase. Furthermore, blue light induces the formation of a protein complex to be formed by tyrosinase and dopachrome tautomerase. This multimeric tyrosinase/tyrosinase-related protein complex is mainly formed in dark-skinned melanocytes and induces a sustained tyrosinase activity, thus explaining the long-lasting hyperpigmentation that is observed only in skin type III and higher after blue light irradiation. OPN3 thus functions as the sensor for visible light pigmentation.
Furthermore, VL and UVA-1 may have a role on conditions aggravated by sun exposure such as post- inflammatory hyperpigmentation and melasma.
Regarding preventive treatments, tinted sunscreens have grown in interest. Currently available chemical UV filters are not sufficient to protect the skin, and there is a growing interest in tinted sunscreen that are able to block visible light. Besides, antioxidants in sunscreen do also play a role in prevention of both erythema in light skin phototype and pigmentation and delayed tanning in darker skin phototype. In vivo studies comparing sunscreen without antioxidants, tinted sunscreens and sunscreen with antioxidants.
Oral agents such Polypodium leucotomos extract (PLE), derived from the tropical fern of Polypodiaceae family, has photoprotective properties against VL. In a study among subjects that received a 28-day supply of PLE (480 mg daily) and irradiation, there was a statistically significant decrease in persistent pigment darkening and delayed tanning post-PLE. PLE may be used as an adjuvant to traditional means of photoprotection to protect against the effects of VL. PLE stimulates tissue inhibitor of metalloproteinases, induces the expression of collagen and elastine, inhibits the expression and enzymatic levels of matrix metalloproteinases and is an antioxidant.
There is currently a trend toward the use of different sunscreens according to different phototypes as illustrated by a recently published recommendation from an expert panel (Figure). Sunscreen should protect against UVB, UVA and VL. Dark skinned individuals need only UVB SPF30 protection, a higher protection against UVA and visible light, because of the risk of hyperpigmentation.
Figure:
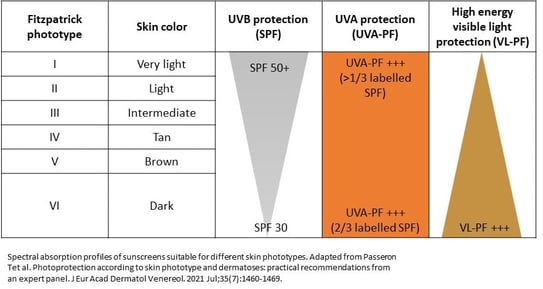
Besides the well-known damaging effects of UV, visible (400-700 nm) can induce damage which contributes to photoaging. We already know that iron oxides and other pigments can be used to reduce the metabolic pathway leading to hyperpigmentation as showed by in vitro and in vivo studies. It is mainly iron oxides that can absorb VL. There is however still issues with the colors of the sunscreens that may not match the skin tones of the patients, in case of extreme skin tones especially. Besides, there is no label for VL protection on sunscreen and sunscreens may claim protection to VL even though they don’t.
To assess VL protection of sunscreens, in vitro pigmentation protection factor based on transmission reduction of VL is most adequate for topical formulation, but the gold standard would be in vivo models. The team of Thierry Passeron aimed to evaluate the correlation between in vivo and in vitro methods in assessing protection against visible light induced pigmentation. They first analysed the in vitro protective properties of the 10 commercially available sunscreens using transmission measurements in the visible spectrum. Then, they performed a monocentric, double-blind, randomized controlled study with intra-individual comparisons in 20 healthy subjects and measure the VL-PF in vivo of those sunscreens. They found a strong significant correlation between in vivo VL protection factor and in vitro transmittance measurements, with the highest correlation factor at 420 nm and in the spectrum covering from 400 to 469 nm. Transmittance measurements were found to be a good predictive tool to evaluate sunscreen visible light photoprotection efficacy and could be used to select formulations for final in vivo testing.
Speakers: Dr. Alia Ahmed, Prof. Anna Zalewska-Janowska, Prof. Mohammad Jafferany, Dr. Piotr Krajewski, Prof. Iknur Altunay, Dr. Maria Jose Tribo-Boixareu, Prof. Laurent Misery, Dr. Sylvia van Beugen and Dr. Maria-Angeliki Gkini
Report written by Prof. Anna Zalewska
The session was chaired by 3 distinguished psychodermatologists – prof. Anthony Bewley from London, prof. Francoise Poot from Brussels, both dermatologists and prof. Lucia Tomas Aragones from Zaragoza, psychologist.
Dr Alia Ahmed from London accustomed the audience with the newly developed British Association of Dermatologists guidelines for the management of people with delusional infestations (Ahmed A et al, Br J Dermatol 2022). By definition delusional infestation is a fixed false belief of pathogenic infestation of the skin or body without objective medical evidence. This condition leads to considerable suffering of the patients and their close relatives. In general, the patients seek consultation with general practitioners and mainly dermatologists due to their skin symptoms, rather than psychiatrists, who are professionally trained with dealing with such patients. The guidelines are available on the webpage as a open access and they are supplemented with a 7-slide power point presentation on communication skills helping when seeing the patient with delusional parasitosis. This power point presentation contains examples of questions that are very useful when consulting the patient with delusional infestations by a dermatologist, but also are of relevance to other specialists.
Prof. Anna Zalewska-Janowska presented current knowledge on neuro-immunological aspects of selected allergic diseases focusing on what is going on in the skin. Of note, currently there are more and more diagnostic methods available like functional magnetic resonance imaging (fMRI) allowing for better evaluation of nervous system activity both central and peripheral. The most powerful systemic stress axis hypothalamus-pituitary gland – adrenal gland has its counterpart in the skin and their interactions with immunological system are more and more widely investigated. Existence of brain- skin and brain-gut axes are now uniformly accepted and investigated in chronic skin diseases encountered also in allergology namely atopic dermatitis, urticaria or contact dermatitis. Pure cartesian i.e. technical approach to our patients did not fulfilled their expectations. Holistic care based on bio-psycho-social approach with good communication skills of professionals is very helpful in everyday practice both for the patients and their medical health providers. Such approach leads to relation and trust improvement together with prevention of burn-out.
Prof. Mohammad Jafferany from Saginaw in the USA accustomed the audience with personality disorders (PDs) in dermatology and focused on the role of a dermatologist in managing those patients. The speaker briefly accustomed the audience with 3 clusters of personality disorders namely cluster A (paranoid, schizoid, schizotypal), cluster B (antisocial, borderline, histrionic, narcisstic) and cluster C (avoidant, dependent and obsessive compulsive). Then, he focused on 3 most commonly encountered PDs in dermatology namely borderline, narcisstic and obsessive compulsive and illustrated the topic with his patients presentations. Professor Jafferany underlined the dermatologic role in the therapeutic process of such patients. Frist, dermatologists should be able to recognize the personality disorder and adjust accordingly. They should be flexible, adaptable patient, accommodative, non-confrontational and non-judgmental and understand that there are underlying psychological conflicts and needs. A sick person is a sick person and we as dermatologists are professionals and we should not take anything personally. Take home messages from the talk: try to identify specific personality disorder and underlying psychological conflict manifesting as skin complaints or the patient specific demeanor. Of importance, interact with the patient in ways to satisfy the underlying psychological needs while maintaining control of the patient encounter. Deliver appropriate medical care and avoid unnecessary medical procedures intervention. And last but not least and extremely important in clinical practice don’t take things personally!
Doctor Piotr Krajewski from Wroclaw in Poland shared his experience on itch and psychological burden presented by his cohort of renal transplant patients. Chronic kidney disease affects 13.4% of the global population and sooner or later leads to troublesome uremic pruritus/itch and causes substantial burden to the patients including depression, anxiety and impaired psychological functioning that should be addressed by health care professionals in the holistic therapeutic process.
Professor Iknur Altunay from Istanbul in Turkey presented her experience on delusional infestations based on running a psychodermatology clinic. The speaker pointed out that despite the fact that delusional infestation (DI) is a primary psychiatric disorder, 90% of patients seek help from a dermatologist. Clinical suspicion is the most important step in the diagnostic process. Of importance, antipsychotic and antidepressant drugs are used together in the treatment. Prof. Altunay presented her experience based on 44 DI patients treated in her clinic since 2012. She pointed to important triggering factors revealed by the patients during the diagnostic process, namely loss of close family member, marriage betrayal, family conflict, physical trauma, dental extraction, acupuncture treatment, accident of a family member or diagnosis of an infectious disease. All patients were examined together by dermatologist and psychiatrist and the most prescribed antipsychotics were risperidone (21 patients), pimozide (5), aripiprazole (4), quetiapine plus antidepressant i.e. fluoxetine or sertraline (2), olanzapine (1), amisulpride (1) and 1 patient was treated with isolated psychotherapy. In conclusion, atypical second generation antipsychotics (risperidone, olanzapine, aripiprazole) are often used in the treatment of DI. Pimozide with 80% effectiveness is not preferred due to its high side effect profile (tardive kinesia, QT interval prolongation).
Doctor Maria Jose Tribo-Boixareu from Barcelona in Spain presented a clinical case of self-inflicted lesions or Morgellons Syndrome. The speaker demosntrated a female patient with generalized pruritus since 2009, who developed neurotic excoriation disorder in 2013. In 2020 diagnosis of Morgellons disease was put forward and the patient started 2.5 mg of olanzapine every 24 hours, gradually increasing to 7.5 mg, with topical high potency corticosteroids and topical antibiotics. Active listening to the patient was also executed. Probably due to not sufficient compliance the patient experienced relapses when the dose was decreased, than restarted on olanzapine 5 mg daily and finally perfenazine was introduced at a dose of 4 mg daily. Academically speaking Morgellons disease is a subtype of delusional infestation and in general requires antipsychotic treatment. As for non- pharmacological strategies establishing a good patient-doctor relationship if of high importance. In conclusion, Morgellons disease must be included within the spectrum of delusion of infestation. Social networks play an important role in the spread of psychodermatological diseases. Morgellons disease requires multidisciplinary management by dermatologists and psychiatrists. And finally training of the dermatologists in skills for the management of patients reluctant to psychiatric treatment is essential.
Professor Laurent Misery from Brest in France accustomed the audience with the idea of creation a new classification of psychodermatological disorders. First, he characterized all up to date published different classification of psychodermatological diseases. The overall aim of this idea is to provide a new, inclusive and very simplified classification and labeling it as international classification of psychodermatological disorders with the hope of being smoothly adopted by all parties involved in the subject.
Doctor Sylvia van Beugen presented the results of the ESDaP 2 study on stigmatization in dermatological patients. Above 5000 dermatological out-patients and almost 3000 skin-healthy controls were recruited in 17 European countries. The following predictors of stigmatization were revealed: lower age, male gender, being single, clinician-rated disease severity, existence of current itch, longer disease duration, higher BMI, worse current health status, higher level of perceived stress and suicidal ideation, more body dysmorphic concerns and lower satisfaction with appearance. In conclusion, patients with skin disease, mainly those suffering from psoriasis, atopic dermatitis, alopecia areata, other alopecias, bullous disorders, experience higher levels of stigmatization than controls.
Doctor Maria-Angeliki Gkini from London in the UK shared her experience on hair disorders and psychosocial comorbidities. The speaker accustomed the audience with the name trichopsychodermatology pointing at significant psychological impact of alopecias. Patients suffering from allopecia present with low self-esteem, poor self-image, feeling of isolation, anxiety, depression or even suicidal ideation. Of importance, patients’ complains about hair loss are often disregarded as only purely cosmetic. Early recognition and management through a true holistic approach is crucial. The speaker underlined that it is of critical importance to inform and empathically reassure telogen effluvium patients about the temporary nature of this condition. As for trichopsychodermatology it is of vast importance to decide about the treatment plan together with the patient – “we are together on this journey”. Support group is absolutely crucial.
Speakers: Prof. Henry W. Lim, Prof. Johann Bauer and Prof. Bruno Lina
Report written by Prof. Anna Zalewska
Professor Henry W. Lim from Grosse Pointe in the USA presented an overview of photo-protection status in 2022. First, he focused on National Academies report released on 9th August 2022 entitled “Review of Fate, Exposure, and Effects of Sunscreens in Aquatic Environments and Implications for Sunscreen Usage and Human Health”. Of note, the report comprises 416 pages and is available at the following link https://nap.nationalacademies.org/catalog/26381/. This report presented entry of UV filters into water when swimming, with stormwater runoff and waste water. When UV filters reach the environment their partitioning occurs into water, air, sediment or organisms. Of importance, organic filters are mainly hydrophobic and partition into particles and sediments occur. Of interest, oxybenzone is moderately water soluble, whereas TiO2 and zinc oxide are found in the sediments. The report demonstrated that highest measured concentrations of UV filters in water ranged between 1 and 10 µg/L, but in the majority of measurements was below 1 µg/L, whereas in sediment concentration of all filters was below 0.1 µg/g dry weight, with the exception of octocrylene and octinoxate, which ranged from 0.1 to 2.4 µg/g. Of note, in high enough concentrations, UV filters can be toxic to algae, invertebre and fish but there are no studies on different species and there is also lack of standard test methods to evaluate this effect like for example for corals in coral reefs. Looking at the environment we should remember that benefits of sunscreen use and photoprotection for human being are very well established and imposing restriction on certain UV filters use may have a profound negative impact on health if it results in reduced use of sunscreen by Homo sapiens representatives. Of importance, only 1/3 of the US population uses sunscreens regularly. For the time being it was concluded that The US Environmental Protection Agency should conduct an ecological risk assessment study on UV filters. Professor Lim accustomed the audience with the issue of photoprotection against longwave UVA1 and visible light, demonstrating their biologic effects on the skin namely pigmentation in dark-skinned individuals and immediate erythema in both light- and dark- skinned human beings. The speaker underlined the following protection measures against visible light and longwave UVA1: tinted sunscreens, new filters and antioxidants. The following paper on the subject could be recommended: Lim et al. Impact of visible light on skin health: the role of antioxidants an free radical quenchers in skin protection. JAAD March 2022;86:S27.
Professor Johann Bauer from Salzburg in Austria delivered a lecture on gene therapy in skin diseases and its current status. He pointed out that currently gene therapies are employed mainly in cancer and genodermatoses treatment. On note, gene therapy could be either transient or persistent i.e. integrated into the genome. In the latter case it could be a classical retroviral gene therapy based on introduction of a synthetic copy of a functional gene r gene editing (CRISPR/Cas), namely in-situ repair. Epidermolysis bullosa (EB) is a good example where classical gene/cell therapy is used. Spectacular clinical photographs demonstrated permanent wound closures on the skin of EB patient were shown.
Professor Bruno Lina from Lyon in France made the audience accustomed with the process of SARS- CoV-2 variants formation and vaccination issues. He clearly demonstrated subsequent phases of virus evolution pointing at the changes which allowed the virus to be more transmissible and able to more and more successfully develop immune-escape mutations. As the take home messages Professor Lina pointed out the following issues: SARS-CoV-2 will remain with us for a very long time and currently we have just started to learn how we can live with COVID being around us. Secondly, immune pressure has become the driving force for selection and evolution, so new variants of the virus are likely to be immune-escape ones. Thirdly, we all the time keep on learning about vaccine effectiveness and duration of protection. Still Wuhan-virus-based vaccines remain protective against severe infections and reduce transmission. Of importance, vaccine strain adaptation has not demonstrated longer immunity or protection but still may reduce transmission. In conclusion we should be prepared on a long-distance “fight” and being vaccinated “fairly regularly”.
Speakers: Prof. Sandrine Dubrac, Prof. Neil Rajan, Prof. Sabine Eming and Prof. Kilian Eyerich
Report written by Prof. Anna Zalewska
Professor Sandrine Dubrac from Innsbruck in Austria presented a lecture on atopic dermatitis (AD) in a format of issues beyond the current paradigms. The speaker gave a concise and informative overview on the pathogenesis of AD pointing out that AD responds best to IL-13/IL-4 targeting. Furthermore, detection of S. aureus on patients skin correlates with severity of AD symptoms. Of interest, skin of AD patients with mild symptoms is rarely colonized with S. aureus, regardless of fillagrin status. Furthermore, the expansion of Staphylococcus on AD skin might be supported by surrounding fungi. Of importance, treatment with dupilumab reduces S. aureus in AD patients. Then, prof. Dubrac focused on role of mitochondria in AD demonstrating that mitochondrial activity is increased in non-lesional AD skin, furthermore inhibition of mitochondrial activity ameliorates AD. Moreover, peroxisomal fatty acid oxidation is increased in lesional AD. Increased glycolysis in AD lesions but not non-lesional AD skin was also observed. The above point out at the importance of metabolic changes in AD and their targeting in not too distant future treatment perspectives.
Professor Neil Rajan from Newcastle upon Tyne in the UK delivered a lecture entitled “Sebaceous tumors: is it time for reflex testing of mismatch repair status?” The speaker gave a brief overview of sebaceous tumors (ST) and ST in cancer families with Lynch/Muir-Torre syndrome. He point out that ST are difficult to diagnose clinically and they comprise only less than 5% of skin adnexal tumors (SATs). Furthermore, ST are a marker of Lynch/Muir-Torre syndrome. The speaker underlined the importance of national registry of rare cancer patients in order to overcome inequity of care also due to limited data to support guideline development and make the policy makers effectively aware of this issue.
Professor Sabine Eming from Cologne in Germany made the audience accustomed with immunological checkpoints in fibrotic skin diseases. First, she presented hallmarks of tissue fibrosis namely inflammation, increase of extracellular matrix (ECM) deposition, altered composition of ECM molecules, altered crosslinking of ECM components, decrease of fat tissue, increased tissue stiffness, loss of tissue/organ function and destruction/loss of skin appendages. The speaker also focused on the observation that cytokine networks drive distinct repair patterns in the skin. Following skin injury when Köbner phenomenon develops and type 1 immunity with TNF-α, IL-12, IL-23, IL17 scare-less healing and regeneration is observed just like in psoriasis. Second pathway is barrier defect with type 2 immunity and IL-4, IL-13, IL-4 when injury resolves with modifications in ECM just like it is observed in eczema. In the third pathway it is hypothesized that after injury TGF-b, IL-4 and IL-13 leads to fibrosis development and modifications in ECM quantity and structure. As regards new treatment options, currently an investigator initiated clinical trial – a randomized, placebo-controlled phase IIa to evaluate safety of subcutaneous dupilumab in localized scleroderma in under way. The regimen is the following – 300 mg of dupilumab bi-monthly for 6 months with 6 months follow-up. The treatment is well tolerated and no major side-effects observed so far. Completion of the study is expected in 2023. There is also romikimab - an engineered, humanized bispecific immunoglobulin G4 antibody that binds and neutralizes IL-4/IL-13 making it an ideal option for exploration in fibrosis. Professor Eming also pointed to a very interesting study entitled “Early-life inflammation primes a T helper 2 cell- fibroblast niche in skin” published by Boothby et al. in Nature in 2021. The authors put forward the idea that inflammation early in life can prime the local immune milieu of peripheral tissues, which can cause lasting changes in immunological tone that confer disease protection or susceptibility. As for take home messages the following issues were raised: tissue fibrosis, not only concerning the skin many internal organs, is an unresolved, major heath issue. Secondly, tissue fibrosis could be regarded as a misregulated healing response. Thirdly, macrophage-fibroblast crosstalk determines outcome of the healing response. Finally, type 2 immunity drives the repair response and fibrosis formation and modulating type 2 immunity by repurposing of IL-4/IL-13 inhibitors might emerge as a new modifying drug to treat fibrosis.
The closing lecture of the session was presented by professor Kilian Eyerich from Freiburg in Germany on special transcriptomics in inflammatory skin diseases focusing on the method both possibilities and limits. At first, the speaker accustomed the audience with technological spectrum of special transcriptomics. Then, prof. Eyerich gave a thorough overview of special transcriptomic possibilities demonstrating that this technique allows to localise RNA transcripts in tissues. The audience learned that T cell mediated inflammation occurs in spots rather than whole areas in the tissue. This technique provides insights into organizational structures including granuloma and sebaceous glands. As for limitations, it is a very expensive technique. Its current resolution is beyond single cell. Furthermore the yield is not perfect and the method is dependent on studied tissue quality (fresh-frozen). As for opportunities, it should be stated that overcoming the limits, especially the resolution issue, could open the possibility to study interactions of cells and tissue structures in health and disease in situ. Special transcriptomics could be further combined with other omics including proteomics, microbiome and lipidome, or phenotyping. Of note as always - right scientific question would open new horizons in research.
Speakers: Prof. Emek Kocatürk Göncü, Dr. Clive Grattan, Dr. Sabine Altrichter and Dr. Heike Rockmann
Report written by Prof. Anna Zalewska
Prof. Emek Kocatürk Göncü, Turkey
Professor Emek Kocatürk Göncü originally from Istanbul in Turkey, currently working in Berlin, introduced the audience with the broad pathogenetic mechanisms of urticaria. Mast cells (MC) still remain the core cells in this disease, however more players are coming to the stage including basophils, eosinophils and T cells. Of note, MC in CSU present lower threshold of stimulation i.e. weaker trigger leads to MC degranulation and the whole cascade of events including wheal and flare reaction develops. Currently CSU is regarded as a systemic disease. Mast cells, eosinophils and microvascular changes persist in uninvolved skin suggesting that non-lesional skin is primed for subsequent wheal formation. It could be concluded that there is a minimally persistent inflammation in the uninvolved skin. Activation of coagulation cascade in chronic spontaneous urticaria (CSU) is worth mentioning with D-Dimers correlating with the disease activity. Furthermore CSU often coexist with autoimmune disorders. About 28% of CSU patients present at least one autoimmunity disorder, thyroid disease being the most prevalent (25.4%), followed by vitiligo (2.3%) and rheumatoid arthritis (1%). Of importance, up to 32% CSU patients present antinuclear autoantibodies (ANA) and above 53% anti-thyroid antibodies. In those patients, a good response to immunosuppressive treatment including intravenous immunoglobulins (IVIG) or plasmapheresis is observed. We can distinguish type I autoimmune (autoallergic) CSU and type 2b autoimmune CSU patients, which - among others - differ in their response to omalizumab (OMA). Type I CSU patients demonstrate quick and good response to OMA whereas type IIb CSU patients are slow in responding to this drug and success rate is also low.
Dr. Clive Grattan, United Kingdom
Professor Clive Grattan from London in the UK delivered a lecture on diagnosis, differential diagnosis and biomarkers in chronic urticaria. He provided the audience with a very practical “urticaria clock”, namely if the wheals persist for 1 hour we could think of inducible urticaria, if for 2 hours – of contact urticaria, if for 24 hour - spontaneous or delayed pressure urticaria should be considered and if for 48 hours – urticarial vasculitis should be in mind. Of importance, practitioners should take into consideration that if the patient, apart from wheals, reports fever and/or pain - autoinflammatory syndrome or vasculitis should be taken into account. Taking home message from the talk were the following: if urticarial wheals are present in a patient – is the diagnosis of urticaria correct. If so, what is the subtype of urticaria and/or what else could it be. Comorbidities should be also addressed and Patient Reported Outcome Measures (PROMS) including Urticaria Control Test (UCT) introduced to the patients regularly to obtain the most reliable dynamics of the disease course and state of the patient.
Dr. Sabine Altrichter, Austria
Dr Sabine Altricher who works both in Linz and Berlin presented a lecture on diagnosis and management of inducible urticarias. She pointed out that symptomatic dermographism, the most common type of inducible urticaria, cause itch and the patients report to their doctors with this symptom predominantly and they do not in general complain of the wheals. Dr Altricher showed, in a concise manner, all the devices allowing to diagnose/confirm the specific type of inducible urticaria. Cold urticaria, which is the second common cause of inducible urticaria, is diagnosed using TEMP TEST. The scope of temperatures for this device is between 4 and 44oC and apart from confirming the diagnosis, threshold of wheals formation could be determined thus severity of the disease and its response to treatment monitored easily. The speaker pointed out that test with the ice cube should be carefully performed. The naked ice cube should not be placed on the patients skin directly due to its high possibility of damaging the skin. The ice cube should be placed in the plastic bag and thus applied to the skin. In this case a mixture of water and ice is much more “friendly” to the skin and allows for diagnosis, of course threshold of wheals development could not be determined using this method. Dr Altricher underlined a very useful information namely that cholinergic urticaria, which presents as small pin-point wheals after being sweat, develops in about 20% of 26-28 year-olds and the diagnosis of this type of urticaria is based on exercising until the patient sweats and practitioners should check wheal formation not earlier than after another 10 minutes of exercising after sweating develops. The presenter also pointed out at the possibility of co-existence of different types of urticaria when diagnosing the patient as for example CSU and dermographism, cold and cholinergic urticaria etc. Practitioners should bare this fact in mind.
Dr. Heike Rockmann, Netherlands
The final talk of the session was delivered by dr Heike Rockman from Utrecht in Netherlands and focused on management of chronic urticaria. The speaker gave a very informative overview of the latest guidelines of urticaria treatment (Zuberbier et al, Allergy 2022, 77,734-66) and concisely presented a step-wise approach to the patients. Dr Rockman underlined that the first generation antihistamines should not be used in urticaria treatment due to its side effects – drowsiness and cardiological ones. Second-generation H1 blockers are the drugs of choice in CSU and when 1 tablet daily is not efficient the dose should be increased up to 4 tablets daily. New information in the guidelines is that when this augmented dose of antihistamines is not effective, the patient should be switched to omalizumab, not cyclosporine and further if OMA in the standard dose i.e. 300mg every 4 weeks is ineffective – dose augmentation up to 600 mg and/or interval of injections diminished (i.e. every 2 weeks). The latter regimen is however off-label and practitioners should inform the patients about this fact. Then cyclosporin comes to the stage and - if ineffective - combination of OMA and cyclosporine could be offered.
In the very lively discussion of the session it was underlined that more than 4 tablets daily of second generation H1 blockers is another option and still effective, however not put in the guidelines.
However, safety issues of higher doses were not evaluated in the published peer-review literature. As for CRP prof. Grattan suggested that in patients with urticarial lesions who present CRP above 30 – autoinflammatory syndrome or vasculitis should be taken into account in the diagnostic process. It just could not be a “simple urticaria”.
Speakers: Dr. Clive Grattan, Prof. Marcus Maurer, Dr. Dorothea Terhorst, Prof. Emek Kocatürk Göncü
Report written by Prof. Anna Zalewska
Dr. Clive Grattan, United Kingdom
Professor Clive Grattan from London in the UK presented a lecture on differential diagnosis of urticaria lesions stressing how important it is to differentiate between urticaria and urticarial. Urticaria is one disease whereas urticarial lesions look like wheals but are not urticaria. Urticarial are rather description than disease. Professor Grattan presented a concise table demonstrating differences between urticaria and urticarial. Namely in urticaria lesions last hours, usually with severe itch, the lesions never leave any marks and never go scaly, they are commonly associated with angioedema, patients never have fever and rarely are unwell and complain for example from arthralgia. Whereas urticarial lesions last for days, severity of itch is variable, the lesions may leave mars, and sometimes go scaly, there is no association with angioedema except for lesions triggered by UV, patients sometimes complain of fever and being unwell could be a key feature patients present. The speaker stressed the usefulness of skin biopsy in differential diagnosis of urticarial lesions. He further presented dermatosis that may be urticarial namely insect bites in a form f popular urticaria, acute dermatitis (including contact dermatitis and atopic eczema), urticaria pigmentosa i.e. cutaneous mastocytosis, immunobullous dermatoses (e.g. pemphigoid, dermatitis herpetiformis), autoinflammatory syndromes (e.g. CAPS, Schnitzler Syndrome), rare dermatoses (e.g. Sweets syndrome, Wells syndrome, connective tissue disorders, infections (prodromal rash in viral hepatitis an COVID-19), urticaria vasculitis (normo- and hypocomplementaemic). The speaker presented 3 subtypes of urticarial vasculitis: normocomplementaemic variant (NUV), hypocomplementaemic (HUV) and the most severe hypocomplementaemic urticaria vasculitis syndrome (HUVS). Professor Grattan concluded his talk with the issue why correct diagnosis really matters namely it allows to perform appropriate investigations, management (both medications and avoidance of triggers), evaluate prognosis and predict inheritance in hereditary autoinflammatory syndromes and last but not least give appropriate patient advice and information. There are simple things but quite often underestimated.
Prof. Marcus Maurer, Germany
PD Dr. med. Dorothea Terhorst, Germany
Professor Marcus Maurer from Berlin in Germany delivered 2 lectures – one in the name of his assistant dr. Dorothea Terhorst on the new finding in cold-induced urticaria and another one in his name and the role of IgE in chronic urticaria.
Concerning cold urticaria, first the speaker presented concise characteristics of cold urticaria: features vary from localized wheals, through throat angioedema induced by cold foods and beverages to systemic reactions (mostly from swimming), females are twice more often affected than males, can occur at any age, is a self-limiting disease (on average lasts 5-9 years) and 4 different types can be differentiated namely primary cold contact urticaria, atypical and secondary cold contact urticaria and finally familial cold autoinflammatory syndrome. Then the speaker focused on findings in cold urticaria concerning pathophysiology, diagnostics, clinical picture, cold induced anaphylaxis and new therapies. As for pathophysiology, autoallergy and autoimmunity come to the stage i.e. circulating IgE directed against an unknown autoantigen that is exposed by low temperature leading to IgE- dependent mast cell degranulation, additionally mast cell-activating IgE and IgM autoantibodies that induce release of histamine from dermal mast cells and basophils have been found in single cold urticaria patients. Of importance, a current meta-analysis of above 1000 cold urticaria (ColdU) patients showed a very low prevalence of cryoproteins in patients with ColdU suggesting that ColdU pathogenesis is driven by another mechanisms and there is no need to check cryoproteins level inthose patients. Prof. Maurer pointed to usefulness of specific Patient Reported Outcome Measures (PROMs) to monitor disease activity, quality of life and disease severity. The available, validate PROMs for ColdU are: ColdUAS 0Cold Urticaria Activity Score, ColdUQoL – Cold Urticaria Quality of Life Questionnaire, SICU – Severity Index of Cold Urticaria. As for diagnostics of not generalized urticarial rashes triggered by cold exposure they are characteristic for certain monogenic autoinflammatory diseases (AIDs) caused by pathogenic variants in the NLRP3, Nlrp12, NLRPC4 and PLCG2 genes. Studies showed that ColdU is not related to post-zygotic or germline pathogenic variants of the above genes and AIDs needs to be differentiated from ColdU. Then, the speaker focused on cold induced anaphylaxis (ColdA) which can be defined as acute cold-induced involvement of the skin and/or visible mucosal tissue and at least one of the following: cardiovascular manifestations, breathing difficulty or gastrointestinal symptoms. Intramuscular adrenaline is the first- line treatment for anaphylaxis. Adrenaline autoinjector should be carried as first aid by patients at risk. In a study by Bizjak M et al (Allergy 2022, 77, 2224-2229) on above 400 patients with ColdU – cold anaphylaxis was diagnosed in 37% of the patients. It is a lot. Bearing in mind safety issues we should remember about important criteria for adrenaline prescription and very important risk factors for cardiovascular manifestations in ColdA namely presence of angioedema, oropharyngeal/laryngeal symptoms and itch of earlobes. The study also demonstrate that ColdA was more common in temperate than cold climate countries. Of importance, ColdA is undertreated and ColdU patients need to be screened by specialists and non-specialists to identify those with ColdA risk factors. As for treatment, a systematic review by Kulthanan TK et al (J Allergy Clin Immunol 2019, 143, 1311-31) revealed greater dosages of non-sedating anti-histamines were more effective than standard doses in controlling ColdU symptoms, increased doses were not significantly associated with higher adverse event rates and finally omalizumab at 150 and 300 mg every 4 wees was effective for ColdU patients refractory to antihistamines. Then, the speaker mentioned syk-inhibitor therapy (Entospletinib), which unfortunately turned out to be not safe in oral form but now is evaluated as a local agent namely “anti- syk cream”. The speaker also underlined the potential effectiveness of barzolvolimab which considerably deplete skin mast cells and serum tryptase. Bearing in mind that urticaria is a mast cell driven disease and when mast cells are decreased the disease have chance to go away. Clinical trails are on the way. Of note, in the diagnostics of ColdU TEMP test instead of ice cubes is recommended.
The second talk of professor Marcus Maurer was focused on the role of IgE in chronic urticaria. The speaker pointed that chronic spontaneous urticaria (CSU) is a true mast cell driven disease, without mast cells urticaria does not exist. Furthermore, CSU is not an allergy. Comparison between autoimmune CSU (type IIb, drived by IgG) – lower omalizumab (OMA) response rate, slow response to OMA, to CyA higher rate of responders, fenebrutinib - fast, good and sustained response and autoallergic CSU (type I) – high OMA response rate, fast onset of OMA effects, unknown response to cyclosporine and fenebrutinib. CSU is autoallergic in most patients. The following finding were demonstrated in CSU patients: positive IgE-anti TPO - in 37% of CSU patients, positive IgE anti-IL-24 in 33%, positive IgE anti-TPO or IL-24 or both – in 56%, single positive IgE-anti-TPO or IL-24 – 42%, double positive IgE-anti-TPO and IL-24 – 14%. Auto-IgE can form complexes with autoallergens.
Auto-IgE crossreacts with auto- and exoallergens. IgE-anti-TPO/IL-24 also bind exoallergens. CSU patients can have IgE-anti-FceRI. Of clinical importance, if Urticaria Control Test (UCT) score is below 12 - urticaria in not controlled and the treatment should go up. UCT between 12 and 15 – urticaria is well controlled (optimize). If UCT is 16 there is a complete control and we can step down with the treatment (Zuberbier et al, Allergy 2022, International Urticaria Guideline). Prof. Maurer demonstrated very useful application for mobile phones i.e. CRUSE for chronic urticaria self evaluation. CRUSE’s mission is to become the biggest platform for patients with chronic urticaria worldwide for disease monitoring, therapy optimization and data generation. Of importance IgE in chronic urticaria explains phenotypes, explains treatment responses and novel targeted treatments. Professor Maurer also demonstrated urticaria registry (www.urticaria-registry.com) and invited the audience to join it and participate in the Global Urticaria Forum (GUF) which is being organized in Berlin between 7th and 8th December this year.
Prof. Dr. Emek Kocatürk Göncü, Turkey
The final lecture of the session was presented by professor Emek Kocatürk Göncü originally from Istanbul in Turkey, currently working in Berlin, on new treatment perspectives for chronic urticaria. The speaker presented numerous factors leading to mast cell (MC) degranulation and releasing vast armamentarium of different mediators. Of note, stimulation of different MC receptors may lead to different granule secretion and thereby different inflammation patterns. Of clinical importance, treatment according to recent guidelines still leave 15-30% of patients with not-controlled disease due to lack of effectiveness, adverse effects and fear of immunosuppression/cancer/organ toxicity.
Different biomarkers, like IgE, anti-TPO, anti IL-24 can help navigate the treatment. The speaker presented vast options of possibilities for CSU treatment including combination of OMA and cyclosporine, meprolizumab, Bruton Tyrosine kinase (BTK) inhibitors, originally launched for B-cell malignancy - fenebrutinib, remibrutinib, ibrutinib, acalabrutinib, tezepelumab - anti-TSLP human monoclonal antibody, C-kit inhibitor – barzolvolimab and siglec-8 monoclonal antibody – lirentelimab. Of note, OMA licence expired in Europe and USA and now a lot of biosimilars are coming. Of interest, ligelizumab, a new anti-IgE in phase 2 studies showed superior efficacy compared with placebo and OMA and higher rates of complete response comparing with OMA together with longer time to relapse after treatment discontinuation (10 weeks), however in phase 3 studies the above observations were not confirmatory and the manufacturer discontinued development of this compound. There are also further treatment possibilities in development like those targeting IL-2, H4R, KIT, cannabinoid receptors, tryptase, BTK, mesenchymal stem cell therapy and still IgE. However, we as clinicians should remember that despite new compounds development we should not forget about good communication skills and having enough time for the patients. It is still crucial! The speaker also invited the audience to join UCARE centres network which is distributed worldwide. Now 126 centres are in the network cooperating for the good of urticaria patients (https://www.ga2len- ucare.com/centers/centers.html).
Speakers: Prof. Kilian Eyerich, Dr. Alan Irvine and Prof. Giuseppe Argenziano
Report written by Prof. Anna Zalewska
Prof. Kilian Eyerich, Germany
This year René Tourraine plenary lecture was delivered by professor Kilian Eyerich from Freiburg in Germany on the precision medicine approaches for inflammatory skin diseases. The speaker introduced the audience with the notion that classification of diseases ontology is based on pure observation. Currently we have numerous techniques that allow for better description of the diseases and we have to re-classify the diseases. Of importance, precise diagnosis matters in the era of specific therapies. We could ask the question – do we really treat the disease that our specific therapy is meant for? The speaker presented a graph with most important techniques and findings in diagnostics of disease starting from 1890 with immunohistochemistry, via 1941 and immunofluorescence, through 1971 and radioallergosorbent test, 2008 with RNA-sequencing to 2021 when spacial transcriptomics came to the stage. Professor Eyerich acquainted the audience with an immune-driven classification of non-cancerous inflammatory skin diseases presenting the following patterns: lichenoid, eczematous, blistering, psoriatic and fibrogenic. He also showed a busy table with current disease ontology – we have hundreds of diagnoses and our disease classification does not fit the molecular targeted therapies that we have currently available. Prof. Eyerich presented the scheme of Freiburg/Karolinska Translational Dermatology with precision medicine, artificial intelligence and biomarker discovery. This scheme is based on 3D full body imaging with clinical examination, questionnaires, blood sampling information from lesional and healthy biopsies, a lot of omics and special transcriptomics coming together for optimal characterisation of the disease we are dealing with. Hopefully, such approach allows to create a basis of new disease ontology and thus implementation of most efficient therapies for each individual.
Dr. Alan Irvine, Ireland
ESDR (European Society for Dermatology Research) plenary lecture was presented by professor Alan Irvine from Dublin in Ireland on the issue of a decade of transformation for patients with moderate-to-severe atopic dermatitis (AD). After introduction of pathological changes observed in non-lesional, acute lesional and chronic lesional AD skin being a Th2 driven disorder, the speaker focused on AD endotypes based on exosome, immune profile, genome, sensitization profile, age of onset and ethnicity. Of note, also non-lesional AD skin is characterized by immune dysregulation, skin barrier dysfunction and subclinical inflammation. Furthermore, prof. Irvine pointed out at increased expression of pruritogens including TSLP, IL-4, IL-13 and IL-31 which signal via histamine- independent molecular pathways as being the most important factors for induction of itch in atopic dermatitis. Of note, itch cytokines directly act on sensory neurons. Moreover, histamine is less important for the induction of itch in AD. Professor Irvine also commented on a very important systematic review and meta-analysis on skincare intervention in infants for preventing eczema and food allergy published by Kelleher MM et al in 2021. The authors draw the following conclusion: regular emollients use during infancy probably do not prevent eczema and probably increase local skin infections. So, in practice we as professionals should be careful as regards any “overdoing”, too much seems to be worse than “not enough”. Definitely the above conclusion requires more careful selectin of infants at risk of AD development for the regular emollient use. The speaker also pointed out at 3 major pathways in AD namely: skin barrier dysfunction, microbiome and immunology (both cutaneous and systemic), all of them intermingled with itch and thus peripheral and central nervous system. Immune pathways seem to be the most tractable ones for targeting. The speaker reviewed recently approved systemic treatments for AD since 2017 by EMA: dupilumab, baricitinib, tralokinumab and upadacitinib. Of importance, many of the pro-inflammatory cytokines that drive AD pathology convey their signals via the JAK1 pathway. The speaker demonstrated informative table comparing JAK inhibitors and biologics pointing out at JAKs as very promising therapeutics for AD. OX40 pathway seems to be a new target for AD. OX40 is a costimulatory molecule on antigen- presenting cells that promotes Th2 polarization of naïve OX40 bearing T cells. Available data so far suggest that OX40 antagonism suppresses activated T cells, mainly atopic Th2 inflammation, and potentially increases T regulatory cells, which may achieve immunologic tolerance and thus lead to disease modification. Professor Irvine mentioned also phase 2 clinical studies disappointments namely keratinocyte cytokines including IL-26, IL-33, TSLP, IL-17C and IL-1α. The speaker also underlines importance and usefulness of classical systemic treatments in AD like cyclosporine and methotrexate. Finally, he summed up future therapeutic aspirations as the following: disease modifying or remission inducing therapies, employment of combination therapies including older ones (like methotrexate, cyclosporine A), employment of bi-specific monoclonal antibodies, elaboration of affordable, potent and non-steroid topical therapies and of importance a greater focus on neuroimmunology and mutual interaction between immunological and both systemic and peripheral nervous systems.
Prof. Giuseppe Argenziano, Italy
Last but not least the session finished off with the third plenary lecture delivered by professor Giuseppe Argenziano from Naples in Italy on present and future aspects of dermoscopy. The speaker presented 3 facts from presence namely: dermoscopy allows for better differentiation of melanocytic lesions and earlier melanoma diagnosis, due to dermoscopy there is a 50% decrease in excision of benign lesions (huge patients and economic savings) and finally there are more than 200 different indications for dermoscopy including tinea capitis, alopecia areata incognito, lupus vulgaris, pigmented purpuric dermatoses, xantogranulomas, skin infections and infestations, epidermodysplasia verruciformis, follicular red dots, porokeratosis, port wine stains etc. He also pointed out at NNT coefficient i.e. number needed to treat which means how many benign naevi are excised for 1 melanoma. NNT for melanoma is 30. It means that we excise 30 benign naevi for 1 melanoma and gave an example from the USA, where this year 100,000 melanomas were excised which means that 3 mln benign lesions were excised as well. Then, professor Argenziano presented 3 future aspects of dermoscopy development entitled “what is very close”, “what is still remote” and “what I wish it were possible”. Polarized total body photography, archiving it and marking and enlarging suspected lesions allowing for close observation in time is very close. Still remote is human- computer collaboration in skin cancer recognition (Schandi et al, Nature Medicine). And the third aspect focuses on changing the behavior of the most aggressive melanomas, the solution is to excise them as soon as possible. Professor Argenziano asked himself a very fundamental question namely “Why people still die of melanoma and what we can do?”. According to the speaker there are 3 culprits of such situation: tumor, patient and doctor. Of note, incidence of thick melanomas and mortality are on the same level since 1975, whereas incidence of thin melanomas increases due to better detection methods. Patients are very often afraid of reporting to the doctor even if they, or their families suspect that it could be something dangerous. Doctors should be more careful and educate patients about the lesions. Taking care and time seem to be crucial. Professor Argenziano dream is also to have in textbooks, apart from clinical and histopathological picture of each disease, also dermoscopic one. A very nice dream. Such a dream should come true as soon as possible Keep our fingers crossed!
Speakers: Dr. Aimilios Lallas, Dr. Luc Thomas, Dr. Wilhelm Stolz and Dr. Caterina Longo
Report written by Dr. Marta Cantarero
Dr Aimilios Lallas from Greece explained the 7 main steps to follow in diagnosing melanonychia striata in the nail unit. The 7 steps are as follows:
Dr Luc Thomas from Lyon first explained the anatomy of the palms and soles of the feet with their characteristic dermatoglyphic structures. The familiar parallel furrow pattern indicates a benign lesion, and the parallel ridge pattern indicates malignancy, as does irregular diffuse pigmentation. He explained that the fibrillar pattern should not always lead us to assume a benign lesion, and showed cases in which this pattern was not benign.
Dr Wilhelm Stolz first explained the types of pigmented lesions we may encounter on the face: flat seborrhoeic keratosis, solar lentigo, senile lentigo, pigmented actinic keratosis, lichenoid keratosis, basal cell carcinomas, lentigo maligna or melanoma. It is important to know that the criteria used for benign vs. malignant lesions in other locations do not apply to facial lesions. It is important to know that benign lesions tend to have more of a brownish colour, like solar lentigo or seborrhoeic keratosis. In contrast, malignant lesions often have a bluish or greyish pigmentation, such as lentigo maligna, melanomas, pigmented actinic keratosis, or basal cell carcinomas.
Solar lentigos are usually lesions which do not present any colouration, never grey or dark brown; they may have milium cysts, parallel patterns and homogeneous pigmentation around the follicle. In contrast, lentigo maligna shows asymmetrical pigmentation of the follicle openings, greyish colouration in dot/globule patterns, and rhomboidal perifollicular pigmentation. To differentiate pigmented actinic keratosis from lentigo maligna, we look at the follicular openings, where we will see keratin.
In any case, if the lesion in question is recurrent and continually growing, we will have to consider performing a biopsy on it.
Dr Caterina Longo gave us a look at dermatoscopy for pigmented lesions of the skin mucosa, which are highly important areas. In these areas, we may encounter pigmented lesions including melanosis (more frequent), nevi, melanomas, Bowen’s disease, seborrhoeic keratosis, basal cell carcinomas, angiomas and others, as well as other non-pigmented lesions such as Zoon’s balanitis, psoriasis, lichen, squamous cell carcinomas, Paget’s disease, warts and others.
In general, any melanosis will present a parallel pattern together with a FISH pattern and brown colour, and is generally multifocal.
If we see diffuse melanotic pigmentation on the lips, the most common causes are syndromic; we need to rule out Peuts-Jeghers, Carney, Bannayan-Riley-Ruvalcaba or Dowling-Degos.
A blue, grey or white colour in a mucosal lesion is always indicative of malignancy, and must therefore be ruled out. A bluish colour may indicate depth.
Nevi usually manifest with globules at any age. Melanosis usually appears with a brown or black colour with parallel or FISH pattern at any age. In contrast, melanoma usually presents with blue, grey or white colouration and does not maintain any structure, primarily in adults over 50 years of age.
Dermatoscopy provides information on other non-pigmented lesions such as: Zoon’s balanitis (linear vessels), Bowen’s disease or squamous cell carcinoma (glomerular vessels and ulceration), psoriasis and lichen (punctiform vessels and Wickham striae), angiokeratomas (gaps), seborrhoeic keratosis (cerebriform patterns) or BCC (vessels).
Speakers: Dr. Andre Lencastre, Dr. Georgios Gaitanis, Dr. Marta Sar-Pomian and Dr. Elisa Cinotti
Report written by Dr. Marta Cantarero
Dr Andre Lencastre captivated the audience with multiple cases in which dermatoscopy can be useful in helping to diagnose different nail pathologies. Onychoscopy can be useful to differentiate onychomycosis from onycholysis following trauma and in connective tissue diseases, and primarily in psoriasis.
In onychomycosis, we can observe longitudinal lines in an aurora borealis pattern, as well as melanonychia, there are usually more than 2 colours, with subungual keratosis and inverted triangular patterns. Traumas usually present with thickened nails, producing onycholysis.
Dr Georgios Gaitanis explained the basics of Raman spectroscopy. This is a rapid and reproducible technique that offers the ability to rapidly diagnose onychomycosis caused by T. rubrum and differentiate it from candidiasis of the nails.
More investigation is needed into other pathologies like psoriasis, dystrophic nails and non- dermatophyte onychomycosis. This technique may also be useful in evaluating nail changes during treatment.
Together with Dr Marta Sar-Pomian, we looked at nail lichen planus, a very important dermatological pathology. It usually appears between the fifth and sixth decades of life, and presents in 15% of patients with cutaneous LP. The fingernails are usually more affected than the toenails, and men tend to be affected more frequently. Usually accompanied by oral lichenoid pathology as well, which is important because it can cause permanent damage in 4 to 12% of cases. Isolated lichen planus of the nail only occurs in 1-2% of cases, and is more frequent in childhood. There are different types: classic, trachyonychia, idiopathic atrophy, erosive or bullous types, and yellow nail syndrome. In 40- 100% of cases the matrix is involved; this may be asymptomatic or may cause itchiness, stinging or pain. It may present with onychorrhexis (longitudinal lines), fragmentation, thinning, pitting, melanonychia, pterigium or anonychia. Treatment with intralesional triamcinolone is provided between
2.5 and 10% at 0.1ml per nail and quadrant; it must be diluted in saline or lidocaine and can be repeated every 4-5 weeks for 6 months. Another possibility is to inject intramuscular triamcinolone in children or adults, with or without intralesional therapy, at a dose of 0.5-1 mg/kg for 3-6 months. Other possible treatments include oral corticosteroid treatment, oral retinoids (acitretin, alitretinoin); azathioprine; cyclosporine or mycophenolate mofetil. We should always provide early treatment for this pathology.
Dr Elisa Cinotti gave a fascinating talk in which she emphasised that longitudinal pigmented bands in the nails should be considered suspicious in the following cases: acute appearance or appearance during adolescence, monodactylic appearance, rapid growth with triangular shape, irregular and multicoloured pigmentation, and especially in the absence of other causes (pharmacological, traumatic, inflammatory, ethnic). In case of doubt, a biopsy of the nail matrix should be taken in all cases.
Over 2/3 of melanomas present in the form of longitudinal pigmentation.
There is an ABCDEF rule specific to differential diagnosis of ungual melanoma:
Speakers: Prof. Brigitte Dréno, Dr. Carmen Salavastru, Prof. Lajos Kemény and Dr. Trinidad Montero
Report written by Dr. Marta Cantarero
Prof. Brigitte Dréno from Nantes captivated listeners with a wonderful talk that updated us about all the latest studies around the physiopathology of acne, which continues to be studied more and more extensively. Her key points related to three factors: sebaceous glands, microbiota and immune system, and keratinocytes.
I will now review the key points presented in her update.
 Polyunsaturated fatty acids inhibit the NLRP3 inflammasome and could therefore help to control acne. Topical creams with 2 polyunsaturated fatty acids have excellent tolerability with no side effects.
Polyunsaturated fatty acids inhibit the NLRP3 inflammasome and could therefore help to control acne. Topical creams with 2 polyunsaturated fatty acids have excellent tolerability with no side effects. Clascoterone cream 1% in a new topical treatment approved by the FDA causes a reduction in sebum and inflammatory activity.
Clascoterone cream 1% in a new topical treatment approved by the FDA causes a reduction in sebum and inflammatory activity. Scars are induced by sebaceous gland atrophy caused by chronic inflammation. They must therefore be treated from the first appearance of the lesions.
Scars are induced by sebaceous gland atrophy caused by chronic inflammation. They must therefore be treated from the first appearance of the lesions. Tacrolimus 0.1% reduces macular erythema.
Tacrolimus 0.1% reduces macular erythema. C. acnes produces a biofilm leading to alterations in the keratinocytes in the microcomedone, thereby contributing to comedone formation.
C. acnes produces a biofilm leading to alterations in the keratinocytes in the microcomedone, thereby contributing to comedone formation. C. acnes is also capable of inducing secretion of inflammatory cytokines.
C. acnes is also capable of inducing secretion of inflammatory cytokines. The dysbiosis that occurs with acne is not limited to C. acnes; S. epidermidis interacts with C. acnes to produce an equilibrium between the two, triggering the activation of inflammatory cytokines.
The dysbiosis that occurs with acne is not limited to C. acnes; S. epidermidis interacts with C. acnes to produce an equilibrium between the two, triggering the activation of inflammatory cytokines.
 Mask acne causes an increase in humidity and sebum production. The role of vitamin D in acne remains controversial.
Mask acne causes an increase in humidity and sebum production. The role of vitamin D in acne remains controversial. The future may lie in treatments like bacterial transplants, TLR inhibitors, anti-IL1 and IL17 biologics, vaccines (anti-CAMPs) and biofilm inhibitors.
The future may lie in treatments like bacterial transplants, TLR inhibitors, anti-IL1 and IL17 biologics, vaccines (anti-CAMPs) and biofilm inhibitors.
Dr Carmen Salavastru from Bucharest explained the particularities of acne in these types of patients. Hormonal acne is caused in part by endogenous androgen overproduction. We know that both androgens and estrogens affect the pilosebaceous unit. It is important to be aware of the possibility of acne during testosterone therapy: it usually starts about 4-6 months after starting testosterone and lasts for about 2 years. Between 50 and 94% of testosterone therapy patients develop acne on their face, thorax and back. Treatment of mild and moderate acne will be the same, using retinoids, benzoyl peroxide, topical and oral antibiotics, bearing in mind that when using tetracyclines together with testosterone therapy, the liver function profile will need to be monitored due to the risk of hepatotoxicity. In addition, even for patients receiving testosterone, oral contraceptives can be considered as another treatment to suppress endogenous estrogens and menstruation without interfering with the exogenous testosterone treatment.
In cases of severe, nodular or recalcitrant acne, isotretinoin is necessary, although we then have to monitor the patient’s state of anxiety for suicidal ideation. We must also keep the patient’s liver function profile in mind if we add tetracyclines, testosterone and isotretinoin.
Topical testosterone therapy is indicated for transgender patients as part of masculinising hormone therapy.
Prof. Dr. Lajos Kemény shared an update on treating acne with isotretinoin.
Oral isotretinoin remains the best drug for controlling acne, providing a major increase in patients’ quality of life. We are currently celebrating its 40th year on the market. However, even today there is still some controversy over the best daily dose, cumulative dose and treatment time. The risk factors for acne flare-ups are: prepubescent acne, family history of acne, location on the torso, excessive seborrhoea and associated endocrine diseases. The doctor concludes that low doses of isotretinoin are also a good option in cases of severe acne; however, in patients with risk factors, prescribe isotretinoin at a dose of 0.5mg/kg. Treatment should be continued for 2 more months after the acne clears up.
Dr. Trinidad Montero from Spain provided an overview of anti-androgen treatment for acne. Anti- androgen treatment is indicated for women with premenstrual skin outbreaks, women with signs and symptoms of hyperandrogenism (hirsutism, polycystic ovaries) and women for whom isotretinoin treatment is contraindicated. Alternatives to anti-androgen treatment are:
 Topical treatments: clascoterone 1% cream is an androgen receptor antagonist, reducing inflammation with rapid onset and few side effects. It is applied twice daily.
Topical treatments: clascoterone 1% cream is an androgen receptor antagonist, reducing inflammation with rapid onset and few side effects. It is applied twice daily. Systemic antibiotics. Tetracyclines. Seracycline is a new tetracycline with a low risk of resistance, but it is more expensive. Azithromycin and amoxicillin/clavulanic acid alone, used for acne during pregnancy. Never use antibiotics as monotherapy, and only for a maximum of 4 weeks.
Systemic antibiotics. Tetracyclines. Seracycline is a new tetracycline with a low risk of resistance, but it is more expensive. Azithromycin and amoxicillin/clavulanic acid alone, used for acne during pregnancy. Never use antibiotics as monotherapy, and only for a maximum of 4 weeks. Hormonal therapies: oral contraceptives, spironolactone, metformin and bicalutamide. Spironolactone at a 50mg dose is the most effective, but it is important to know that it can cause irregular menstruation, gynaecomastia, reduced libido and hyperpotassemia which we will need to monitor. Metformin has an anti-inflammatory effect that is very useful in cases of polycystic ovaries at a dose of 850mg/day, and also improves ovulation. Bicalutamide is a nonsteroidal anti-androgen for which we need to monitor liver function. Other treatments are zinc and probiotics.
Hormonal therapies: oral contraceptives, spironolactone, metformin and bicalutamide. Spironolactone at a 50mg dose is the most effective, but it is important to know that it can cause irregular menstruation, gynaecomastia, reduced libido and hyperpotassemia which we will need to monitor. Metformin has an anti-inflammatory effect that is very useful in cases of polycystic ovaries at a dose of 850mg/day, and also improves ovulation. Bicalutamide is a nonsteroidal anti-androgen for which we need to monitor liver function. Other treatments are zinc and probiotics.Speakers: Dr. Zrinka Bukvic Mokos, Dr. Burhan Engin, Dr. Christoforos Vlachos and Dr. Zsanett Renáta Csoma
Report written by Dr. Marta Cantarero
Dr Zrinka Bukvic Mokos from Croatia gave us a global overview and review of the pathology of acne. Acne is a chronic inflammatory disease with a significant emotional impact. A combination of therapies should be started early, and we must attack the causes of acne in its pathogenesis. Various algorithms have been proposed, but we must always adjust the treatment to each patient. We can classify acne into mild/moderate comedonal or papulopustular acne, and severe nodular acne or acne conglobata. In the case history, we need to know the time of progression, when the acne started, and a list of medications that may make acne worse, and we must also evaluate the patient’s psychological situation. In addition, we must look at pigment changes involved in the pathology, as well as scarring and evidence of hyperandrogenism (or lack thereof). With women in whom hyperandrogenism is suspected, blood testing is needed for total and free testosterone, DHEAs, 17- hydroxyprogesterone, LH and FSH. A differential diagnosis must always be performed to rule out pathologies like rosacea, perioral dermatitis, gram-negative folliculitis, malassezia folliculitis and milia. For comedonal acne, retinoids are the first line of treatment. To treat mild/moderate inflammatory acne, the first line of treatment is a combination of adapalene with benzoyl peroxide and clindamycin. Never use antibiotic therapy as monotherapy. For severe acne, isotretinoin continues to be the treatment of choice. Anti-androgen hormonal therapy should also be considered for women with signs of hyperandrogenism, women who do not respond to the standard treatment, and those with premenstrual outbreaks.
Dr Burhan Engin from Istanbul gave us an update on rosacea. Rosacea is a common chronic inflammatory disease characterised by persistent erythema in the centre of the face, papules, pustules, flushing, telangiectasias and phymatous skin outbreaks. It tends to occur more often in women, mainly after the age of 30. The most commonly affected phototypes are phototypes I and II. There is chronic inflammation. Demodex mites are involved and are proposed as a trigger; however,
H. pylori is also observed in these patients, though the relation is not yet known. There are four types of rosacea: erythematotelangiectatic, papulopustular, phymatous and ocular. A differential diagnosis must be performed to distinguish from sun damage, seborrhoeic dermatitis, dermatomyositis, other disorders that cause flushing, long-term use of topical corticosteroids, or keratosis pilaris rubra. Treatment should be individualised for each patient.
Dr Christoforos Vlachos from Greece talked about folliculitis in regions like the face and trunk. There is an exceptional immune balance in the hair follicle. Infectious folliculitis is the norm, but there are a few exceptions. Dermatoscopy can be of considerable help in diagnosing folliculitis. There has been an increase in folliculitis in the Covid era – but this increase is due to the garments used to prevent Covid, not the virus itself. Staphylococcus aureus is the most frequent cause of folliculitis. Fungal folliculitis is also possible, with malassezia as the most frequent agent, forming monomorphic and pustular papules on the upper trunk and face. Other agents, such as candida, are rare. Some types of folliculitis fall within the category of chronic inflammatory diseases, such as folliculitis ketoidalis and decalvans or perifolliculitis capitis abscedens et suffodiens. Eosinophilic pustular folliculitis usually manifests in childhood. Certain drugs can induce folliculitis: antibiotics, halogens, immunosuppressive agents, antiepileptics.
Dr Zsanett Renáta Csoma gave a masterful talk presenting multiple clinical photographs of eczema cases in newborns and infants. Eczematous disorders in children are a frequent subject of consultation. Some cases are easy to diagnose, such as atopic dermatitis manifesting as bilateral malar eczema, and other less frequent cases like perioral dermatitis, in which we see inflammatory papules and pustules in the perioral, nasolabial and occasionally periocular regions, together with plaques and granulomatous forms, itching and stinging. A differential diagnosis should always be performed for seborrhoeic dermatitis. Other differential diagnoses are those for systemic lupus erythematosus, Zn deficiency, atopic dermatitis, Langerhans cell histiocytosis (affecting scalp, retroauricular and nappy areas), Omenn syndrome. With seborrhoeic dermatitis, we frequently see patients affected between the 4th and 6th weeks of life, with scalp affectation in an oily, scaly form; the forehead, eyelids, nasolabial folds, and retroauricular areas may be affected, as well as the nappy area and intertriginous areas. Scabies and congenital ichthyosiform erythroderma are also among the differential diagnoses that the doctor presented in her numerous photographs.
Speakers: Dr. Christos C. Zouboulis, Dr. Joana Cabet, Dr. Thrasyvoulos Tzellos and Dr. Gregor B.E. Jemec
Report written by Dr. Marta Cantarero
Dr Christos C. Zouboulis updated us with the latest on the pathogenesis of hidradenitis suppurativa. It is important to understand that there are many epidermal cells involved in hidradenitis suppurativa, and genetic mutations have been identified. About 59 mutations of the gamma secretase complex NCSTN have been identified. Genetic mutations are not sufficient to induce hidradenitis suppurativa. Mutations of the gamma secretase complex affect signalling in the pathway involved in keratinocyte differentiation and proliferation. The molecular pathways detected in HS are related to antimicrobial peptides and cytokines. There is a possible combination of innate immunity and triggering by microbial factors. Smoking and obesity are clearly the most significant aggravating factors for this disease.
Dr Joana Cabet from Portugal summarised the different phenotypes of patients with HS. There are still many gaps preventing us from understanding the full spectrum of hidradenitis suppurativa.
Investigations of the relationship between polymorphisms, molecular endotypes and phenotypes are under way. This knowledge is essential for identifying biomarkers of the disease, its activity and its response to treatment. It is also the key to treatment and the development of new treatments. There is currently no consensus with regard to the classification of phenotypes; however, clinical presentation will influence the immediate treatment of the disease. Dr Cabet emphasised that the most important step with hidradenitis suppurativa patients is to determine in which patients an aggressive course is most likely, and to be able to differentiate the inflammatory phenotype (abscesses, fistulas and scarring) from the follicular phenotype (comedones, folliculitis, papules and pustules, nodules and acneiform scarring). We need to be proactive with the inflammatory phenotype, treating the inflammation and not postponing biological treatment.
Dr Thrasyvoulos Tzellos from Norway explained how the bacterial microbiome has been characterised in patients with hidradenitis suppurativa. Commensal bacterial flora and anaerobic bacteria are associated with Hurley stages 1, 2 and 3. Each successive stage involves greater antibiotic resistance. Clostridium difficile infection is greater in patients with hidradenitis suppurativa, leading to increased mortality among these patients. Hospitalised patients and elderly patients are more vulnerable. The key points of the talk are as follows:

 There is no evidence for the use of specific antibiotics.
There is no evidence for the use of specific antibiotics.  Eliminate the minimum dose.
Eliminate the minimum dose. Only an antibiotic of the same class should be used, for a maximum of 12 weeks.
Only an antibiotic of the same class should be used, for a maximum of 12 weeks.
 Use antibiotics for up to 3 months, and reintroduce in case of recurrence if they were effective.
Use antibiotics for up to 3 months, and reintroduce in case of recurrence if they were effective.
Dr Gregor B.E. Jemec from Denmark spoke about the future of hidradenitis suppurativa treatment. Hidradenitis suppurativa and Crohn’s disease respond to treatment with infliximab; this result was published in 2001, and since then the age of biologics has begun. In 2009, research was published on treating HS with TNF alpha inhibitors. Apremilast, brepocitinib (TK2/JAK1), and INCB054707 (JAK1) represent the present and near future in the treatment of this disease.
Speakers: Dr. Paolo Custurone, Dr. Nanja van Geel, Dr. Viktoria Eleftheriadou, Prof. Khaled Ezzedine
Report written by Dr. Marta Cantarero
Dr Paolo Custurone gave us an update on the mechanism by which hypopigmentation forms. Nonsegmental vitiligo presents a complex pathogenesis. The best-characterised hypothesis is currently the autoimmune hypothesis. Finding the primary stimulator is essential, and treating the factors that fight the disease is equally important. Factors being studied in the pathogenesis of vitiligo include adhesion molecules, interleukins, the role of oxidative stress, mRNAs, haplotypes, and genes.
Dr Nanja van Geel told us that for the first time, we now have international guidelines for managing and treating vitiligo, developed with the participation of 42 expert dermatologists and 4 patients’ associations. The key points are as follows. First, a proper diagnosis must be done to differentiate segmental vitiligo from the nonsegmental and mixed types. We need to know how the disease has developed in the past few months and whether it has been active or stable, mainly on the basis of photographs; we need to detect any signs of activity like the confetti pattern, the Koebner phenomenon, and inflammatory edges of hypochromic areas; and we need to standardise it with quantitative variables. As for treatment, it will depend on the diagnosis and the phase of activity.
Treatment must be at an early stage, and in case of rapid progression, we will need to consider whether it is subsidiary to systemic treatment. A combination of treatments has been found to be more effective than monotherapy. Treatment should be re-evaluated every 3-6 months.
Dr Viktoria Eleftheriadou explained that we should follow the recently published international guidelines for treating vitiligo, and that the proposed algorithms are safe and effective. The first line of treatment is high-potency topical corticosteroids applied daily; in the facial area, tacrolimus 0.1% should be considered primarily for the periocular region, and we should consider prescribing tacrolimus 0.1% under occlusion in non-facial regions. As a second line of treatment, NB-UVB phototherapy can be used either alone or in combination with topical corticosteroids and calcineurin inhibitors. In rapidly progressing cases, we should consider prescribing betamethasone at 0.1mg/kg twice a week or on two consecutive days for 3 months. For the third line of treatment, we can use excimer laser therapy together with calcineurin inhibitors for localised vitiligo, cell transplants for segmental vitiligo, and CO2 laser with 5-fluorouracil in adults with nonsegmental vitiligo; and depigmenting therapies should be considered for very extensive cases of vitiligo.
Prof. Khaled Ezzedine emphasised vitiligo’s importance in the psychosocial realm, noting that it is not merely a skin disease. He discussed how 168 studies have shown that patients with vitiligo experience comorbidities such as stigmatisation, sleep disorders, reduced self-esteem, sexual problems, insomnia, anxiety disorders, inappropriate social behaviour, increased dependency on alcohol and other drugs, and even suicide. In light of all this, then, our treatment and diagnosis must be based on a multidisciplinary principle to address all the psychosocial aspects that affect patients with vitiligo.
Speakers: Dr. Jelena Stojkovic-Filipovic, Dr. Sergio Schalka, Dr. Mauro Picardo and Dr. Zoe Apalla
Report written by Dr. Marta Cantarero
Dr Jelena Stojkovic-Filipovic from Belgrade explained that hyperpigmentation has many production pathways, that it is influenced by hormones, age and inflammation, and that cells such as keratinocytes, fibroblasts, endothelial cells and inflammatory cells are also involved in its development. Hyperpigmentation is a complex occurring in most dark phototypes starting at III. We can classify pigmentary pathologies into diffuse and circumscribed, linear, and reticulate hyperpigmentation, as well as dyschromias. Among the different types of hyperpigmentation, we must distinguish those that are produced by an increase in melanin (reactive or non-reactive) and those that are produced by increased cell proliferation involving either keratinocytes or melanocytes. As for postinflammatory hyperpigmentation, we need to understand that skin inflammation produces prostaglandins, leukotrienes and thromboxane, and that this in turn produces melanocytic hypertrophy and increases melanin synthesis.
Dr Sergio Schalka from Brazil talked to us about the power that visible light has within the solar spectrum, and about its consequences. Visible light can produce hyperpigmentation. Within the visible light range, high-energy blue light has the greatest ability to cause hyperpigmentation. The tints used in current photoprotection products offer protection against the pigmentation effects of visible light.
New active ingredients, filters and antioxidants present new opportunities to protect against visible light. Protection from visible light is especially important in melasma with dark phototypes. As for mobile devices and the production of blue light, we know that one hour of sun exposure is equivalent to 99 hours of TV and 700 hours of light from mobile devices, so there is a big difference here. High- energy visible light represents 13% of total solar radiation, i.e. more than both UVA and UVB combined, hence its increasing importance.
Dr Mauro Picardo talked about the various agents used in treating hyperpigmentation. With regard to tyrosinase inhibitors, he mentioned hydroquinone, which plays an important role in degrading melanosomes. Kojic acid inhibits tyrosinase, azelaic acid, thiamidol is better than hydroquinone 2%. In addition, adapalene, tazarotene, azelaic acid and isotretinoin have shown an effect in improving hyperpigmentation. Tranexamic acid is a plasmin inhibitor that promotes the inhibition of tyrosinase activity to block keratinocyte interactions with melanocytes. Microneedling and radio frequency treatment may help to promote these agents. Kligman’s triple combination remains the most effective approach for melasma.
Dr Zoe Apalla from Greece presented an excellent talk on melasma. Melasma is a very common and important chronic cosmetic pathology. It also has a negative impact on patients’ quality of life. We need to differentiate melasma from exogenous ochronosis, and this distinction can be made with dermatoscopy alone. Other differential diagnoses are fixed drug eruption and malignant lentigos.
Before treating the patient, we need to know where the pigment is: epidermal (brown reticulum, dark with telangiectasia), dermal (with a more greyish reticulum, annular and cellular structures), or mixed. A Wood’s lamp test can also help us with this diagnosis: A positive Wood’s result means epidermal pigment, and a negative result shows no contrast. In terms of the range of treatments, options include: topical treatments applied by the patient, peelings, energy devices, PRP; and systemic treatments like tranexamic acid, polypodium leucotomus, beta carotenes, melatonin and procyanidin, and of course photoprotection as well.
Speakers: Dr. Piergiacomo Calzavara-Pinton, Dr. Giovanni Leone, Dr. Salvador González Rodríguez and Dr. Eva Remenik
Report written by Dr. Marta Cantarero
Dr Piergiacomo Calzavara-Pinton from Italy presented the many studies about the benefits of photoprotection with regard to melanoma and non-melanoma skin cancer and actinic keratosis. But in the real-life statistics we’re seeing for skin cancer, the numbers are continuing to increase, and we have to wonder why. Years ago, photoprotectors showed poor uniformity, while others produced toxic photoproducts, incorrect (insufficient) application of photoprotectors, lack of reapplication, long-term photoprotection, and a lack of physical methods of photoprotection. The future of photoprotectors will go hand in hand with organic filters, the nanotechnology to produce them, and apps which will identify our geographic location and tell us what kind of photoprotection we need to apply, whether physical or chemical.
Dr Giovanni Leone from Italy talked about primary and secondary photoprotection, and about natural substances used as filters.
The most important factor in the development of new filters is safety. The most recently developed filters are: Bis-diethylaminohydroxybenzoyl-piperazine (BDBP), phenylene bis-diphenyltriazine, and methoxypropylamine cyclohexylidene ethoxy ethyl cyanoacetate. Secondary photoprotection refers to molecules that provide photoprotection after sun exposure, such as antioxidants. As far as botanical particles, experts are working on new tests, norms and efficacy standards that could represent an opportunity for the future.
Dr Salvador González Rodríguez from Madrid discussed photoprotection. Needless to say, oral photoprotection occupies an important position in photoprotection in general. It cannot substitute for conventional photoprotection, however. It can prevent photodamage to DNA and improve the DNA repair process, prevent a drop in Langerhans cell count, and reduce melanin oxidation and melanogenesis induced by visible light.
It should be used in at-risk populations such as: lighter phototypes, patients with photodermatitis and photoaggravated skin, patients with skin cancer, patients receiving phototherapy as adjuvant treatment, and in patients with dark phototypes to prevent hyperpigmentation.
Dr Eva Remenik from Hungary discussed skin pathologies involving exaggerated cutaneous reactions to sunlight and abnormal reactions to normal doses of sunlight. Photodermatoses may have a genetic or context-induced basis or may be idiopathic or due to photoaggravated photodermatosis or immunological causes. Among the endogenous or metabolic causes is porphyria, for which UVA protection is important. We must also take account of drug-induced photodermatoses, for which UVA radiation is the most important type to protect against. Other pathologies for which photoprotection is indispensable are juvenile spring eruption, actinic prurigo, actinic folliculitis, solar urticaria, photosensitive dermatitis and hydroa vacciniforme.
BIODERMA Congress Reports IMCAS 2022



BIODERMA Congress Reports WCRSD 2022

BIODERMA Congress Reports CILAD 2022