3 professionals
Bioderma Congress Reports JDP 2025
Bioderma Congress Reports JDP 2025
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Déborah Salik (dermatologist, Belgium), Nicolas Kluger (dermatologist, Finland) and Ibrahima Traoré (dermatologist, Guinea)

Related topics
Report written by Déborah Salik (dermatologist, Belgium)
Chair: Yvon Perrillat (France)
Speakers: Yvon Perrillat (France), Thierry Fusade (France), Samy Fenniche (France), Kawtar Zouhair (Morocco), Nathalie Gral (France), Sabrina Fourcade Roch (France)
Introduction
The aim of this practical workshop was to introduce participants to different laser technologies. Each participant was able to familiarise themselves with how they work, handle the equipment in real-life conditions and master essential safety rules for day-to-day use.
Techniques and safety
The session began with a reminder of the essential safety instructions. When using lasers in dermatology, you need to wear specific protective eyewear, tailored to the wavelength of the laser used. Patients are strongly advised to use eye shields to prevent any risk of error relating to the type of eyewear.
Vascular lasers and intense pulsed light (IPL) :
Pulsed dye laser (PDL) treatment operates at a wavelength of 595 nm, which corresponds to the absorption spectrum of haemoglobin. It can be coupled with a YAG laser for dual action. Its main indications are flat angiomas (face, trunk, limbs), rosacea, poikiloderma of Civatte and spider angiomas. It is suitable for infants.
Other vascular systems also exist:
CO2 laser
CO2 laser is a powerful ablative tool operating at 10600 nm. UltraPulse can reach a depth of 4 mm and is used for scars, facial resurfacing and the treatment of condylomas. The Déka system combines an ablative CO2 laser (10600 nm) with a non-ablative fractional laser (1540 nm) to prevent post-inflammatory hyperpigmentation, particularly in the resurfacing of atrophic scars.
Lasers for pigmented lesions
They treat pigmented lesions and are also used for tattoo removal. Q-Switched systems use wavelengths of 1064 nm (infrared, for deep lesions such as naevus of Ota) and 532 nm (peak melanin absorption, up to phototype IV). The work must always be carried out at the focal point.
AviClear
This is an innovative laser for treating inflammatory acne at a wavelength of 1726 nm. It acts directly on the sebaceous glands, causing atrophy and reducing sebum secretion.
Hair removal lasers
Alexandrite and Nd:YAG are the most commonly used. These types of lasers are also indicated for conditions such as pilonidal cysts and Verneuil’s disease.
Report written by Déborah Salik (dermatologist, Belgium)
Chair: Henri Adamski (France)
Speakers: Henri Adamski (France), Martine Avenel-Audran (France), Chistophe Bedane (France), Christelle Comte (France), François Aubin (France), Laurent Meunier (France), Manuelle Viguier (France), Jean-Claude Béani (France)
Solar radiation: Composition
Report written by Déborah Salik (dermatologist, Belgium)
Speaker: Henri Adamski (France)
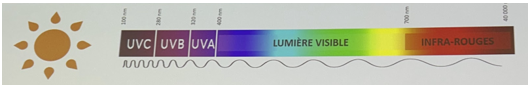
Solar radiation consists of UVA and UVB rays (7%), but also includes visible light (40%) and infrared radiation (53%).
Radiation characteristics
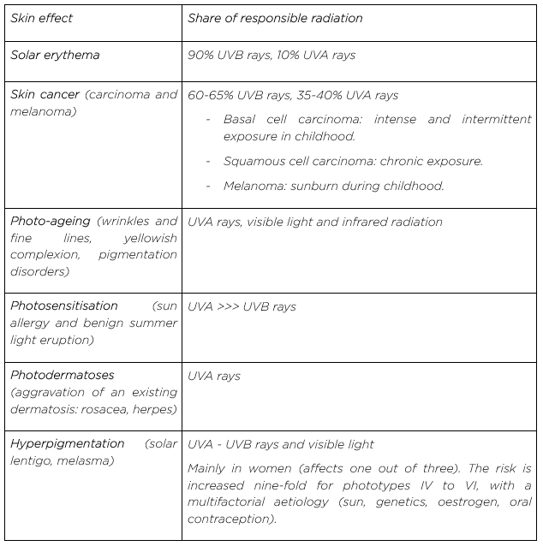
The effects of the solar spectrum on the skin
Beneficial effects
Exposure to the sun has positive effects on seasonal depression and also on vitamin D synthesis (via UVB rays).
The amount of UV radiation needed to synthesise vitamin D is very low. According to the literature, a white child wearing clothes and exposing his hands and face requires 30 minutes to two hours of exposure per week for adequate vitamin D synthesis. For adults, five minutes of exposure per day, three times a week, is mentioned for a light phototype and 10 minutes for a dark phototype (PMID: 16164370). The use of adequate sun protection does not alter patients’ vitamin D status, unlike their exposure habits (seeking shade, clothing).
AFSSAPS recommendations for anti-sun products stipulate that an anti-sun product should meet three criteria: persistence, photostability and protection against all the harmful effects of UV rays.
Report written by Déborah Salik (dermatologist, Belgium)
Speaker: Bertrand Richert
Professor Richert gave an account of his most impressive cases over the last 35 years.
Onychopapilloma
The most frequent diagnoses with nail alterations in children (PMID: 30835872)
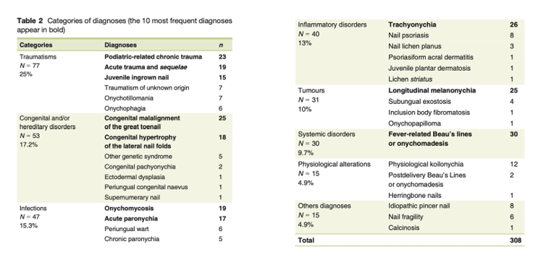
Nail disorders in children are generally benign and often self-limiting.
Iso-Kikuchi syndrome
Congenital onychodysplasia of the index finger (MIM605779), or Iso-Kikuchi syndrome, corresponds to an abnormality of the nail of the index finger revealing underlying bone involvement. Various diagnostic criteria have been described: congenital brachymetacarpia and/or brachydactyly, uni- or bilateral hypoplasia of the index finger and onychodysplasia of variable appearance. X-rays confirm the diagnosis, showing Y-shaped bifurcation and hypoplasia of the distal phalanx of the finger concerned.
Various pathophysiological hypotheses have been put forward: iatrogenic (anticonvulsants during pregnancy), vascular (in utero ischaemic damage to arterioles that depend on the radial artery), or alterations in osteogenesis. None have been confirmed. Several familial cases have been reported, suggesting autosomal dominant transmission of a monogenic Mendelian disease, but no gene has yet been described.
Squamous cell carcinoma
Onychomatricoma
Retronychia
Classic triad in retronychia
(1) Cessation of nail growth
(2) Paronychia
(3) Xanthonychia
Report written by Déborah Salik (dermatologist, Belgium)
Chair: Laura Fertitta (France)
Speakers: Laura Fertitta (France), Aranaud Jannic (France), Sébastien Barbarot (France), Pierre Wolkenstein (France), Mona Amini-Adle (France)
Subcutaneous neurofibromas and differential diagnosis
Speaker: Sébastien Barbarot (France)
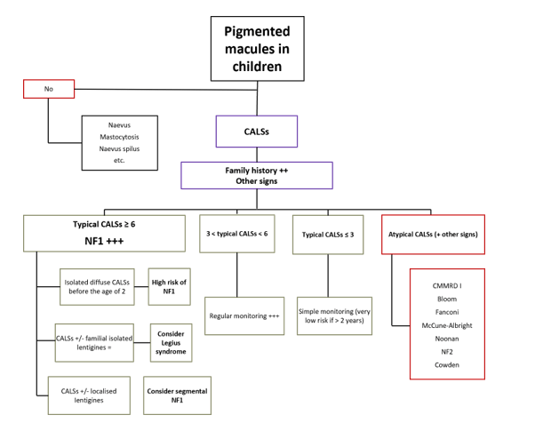
There are six questions to ask when faced with café au lait spots (CALSs)
Algorithm for managing CALSs in children:
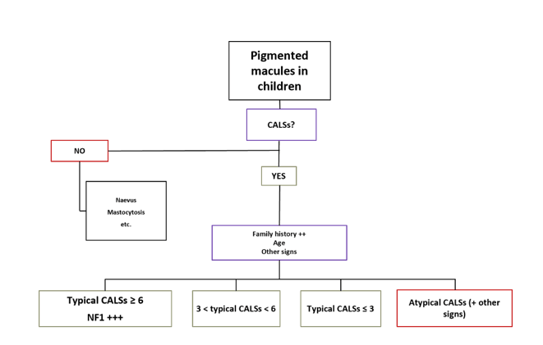
Patients with three CALSs represent 20% of the population.
Differential diagnoses for CALSs:
A CALS suggestive of NF1 is a rounded oval macule with a clear border, sparing the cephalic extremity. Lesions are generally present at birth and lentigines appear around the age of two to three years. Neurofibromas (NFs) appear later and are highly polymorphic. They are either superficial, maculopapular with skin atrophy, or subcutaneous, forming small, firm nodules along nerve pathways. Their presence is a factor for poor prognosis and the presence of internal neurofibromas.
Large CALSs can become progressively hairy and may be associated with the presence of plexiform NFs. Plexiform NFs can also be atrophic, but this is a rarer clinical presentation.
There is also a segmental presentation of NF1, which corresponds to type 1 (due to a postzygotic mutation) or type 2 mosaicism, based on the second-hit hypothesis.
There may be other associated clinical signs:
Other conditions with CALSs:
1. Legius syndrome
2. Noonan-lentigines or LEOPARD syndrome
3. Non-PTPN11 Noonan syndrome
Presence of ulerythema ophryogenes
4. Bloom syndrome: scoliosis, chronic cheilitis, facial erythema (photosensitivity), “butterfly wing” telangiectasias
5. McCune-Albright syndrome
6. Turcot syndrome: Childhood constitutional mismatch repair deficiency
7. CM-AVM: RASA1 - EPHB4
In short:
Complications of NF1
Speaker: Laura Fertitta (France)
NF1 is a multisystem disease with complications that differ according to age.
In children:
1. Optic pathway glioma
2. Neurodevelopmental complications
3. Bone complications
4. Long bone dysplasia
5. Growth and weight-related complications
6. Cardiovascular complication: hypertension
In adults
1. Ophthalmological complications
2. Screening for hypertension
3. Bone demineralisation
4. Specific case of pregnancy
5. Risk of cancer
Management of plexiform NFs
Speaker: Mona Amini-Adle (France)
Plexiform NFs
SPRINT study: Selumetinib
MIRDAMETINIB
There is mucocutaneous toxicity associated with MEK inhibitors, with acne, paronychia, aphthous ulcers and ulceration of the oral mucosa.
Report written by Déborah Salik (dermatologist, Belgium)
Chairs: Thomas Hubiche (France), Sébastien Barbarot (France), Hamida Turki (Tunisia)
Speakers: Isabelle Luchsinger (Switzerland), Malek Cherif (Tunisia), Constance Deblock (France), Juliette Mazereeuw-Hautier (France), Rajaa Bousmara (Morocco)
X-linked hypohidrotic ectodermal dysplasia: specific phenotype in female transmitters
Speaker: Isabelle Luchsinger (Switzerland)
X-linked hypohidrotic ectodermal dysplasia is the most common form of ectodermal dysplasia. The phenotype of female carriers is poorly characterised.
Objective: Describe the symptoms in women who transmit the disorder.
Method: Prospective study including women with a variant in the EDA gene.
Results: 36 women with:
Dental:
Dermatological:
Breast abnormalities:
Conclusion: It is important to be able to identify female transmitters based on clinical criteria. These women deserve appropriate multidisciplinary support.
Palmoplantar keratoderma in autosomal recessive congenital ichthyosis: clinical and genetic features
Speaker: Malek Cherif (Tunisia)
ARCI is a heterogeneous group of non-syndromic ichthyosis.
Aim of the study: to describe the different aspects of palmoplantar keratoderma (PPK) in ARCI and to establish a phenotype-genotype correlation.
Method: A 20-year retrospective study of patients with ARCI. Evaluation of the features of PPK in these patients according to their genotype.
Results: 41 patients
Effectiveness of a targeted high-throughput sequencing panel for the molecular characterisation of ichthyosis
Speaker: Constance Deblock (France)
Inclusion criteria: Molecular analysis and clinical diagnosis
Panel of 38 genes associated with ichthyosis
Patients classified according to conclusive gene: class IV or V
Inconclusive: No pathogenic variant or a single heterozygous variant
Results: 90% of patients obtained a conclusive result
Inconclusive results: 11% (n=33) had whole-genome sequencing: Five had a conclusive result
Conclusion: The panel was of interest because it was very effective, which was a quick step, but regular updating is essential. Whole-genome sequencing is useful for finding non-coding or structural variants.
Ichthyosis linked to variants in the ELOVL1 gene: a rare and poorly understood syndromic form of ichthyosis
Speaker: Juliette Mazereeuw-Hautier (France)
Congenital ichthyosis is classified into three groups:
ELOV1 is essential for the synthesis of long-chain fatty acids in the skin
ELOV1: AD form and AR form
Study of the c.494C>T variant (p.Ser165Phe)
Phenotype
Discussion: This ELOV1 variant is associated with a characteristic triad of dermatological, ophthalmological and neurological signs.
Neurological signs are at the forefront of the disease and are a major cause of its severity.
No correlation between cutaneous and neurological severity.
Pathophysiological hypothesis: dominant negative effect
Enables targeted therapeutic approaches to be considered by inhibiting the mutant mRNA using an antisense oligonucleotide approach.
Efficacy and safety of topical gentamicin 0.1% in inherited epidermolysis bullosa
Speaker: Rajaa Bousmara (Morocco)
Inherited epidermolysis bullosa (IEB) is a genodermatosis that causes skin and mucous membrane fragility.
No curative treatment at present, but an emerging concept: stop-codon readthrough to enable synthesis of a complete protein.
Study: Evaluation of the effect of gentamicin 0.1% applied twice a day for 21 days.
Four patients had DEB and JEB.
The results showed very good, fairly rapid healing after one month, but this was marked by cases of recurrence over the longer term (three months on average).
Gentamicin B1 has strong nonsense mutation suppression activity and promotes collagen VII synthesis.
Gentamicin is a promising therapeutic option for IEB linked to nonsense mutations.
It is an alternative to gene and cell therapies, which are often inaccessible.
Intravenous gentamicin may provide improvement for up to six months and is well tolerated. Studies are under way to determine the appropriate doses for children in order to limit the side effects.
Report written by Nicolas Kluger (dermatologist, Finland) based on:
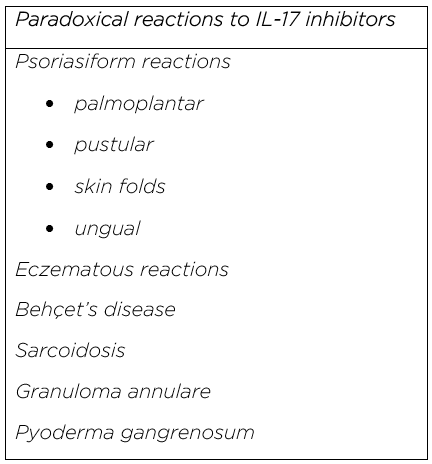
The anti-IL-17 biotherapies currently available in dermatology in France include secukinumab and ixekizumab, two monoclonal antibodies specifically targeting IL-17A; brodalumab, which blocks the IL-17RA receptor and thus inhibits several IL-17 isoforms; and bimekizumab, which simultaneously neutralises IL-17A and IL-17F, offering broader inhibition of the IL-17 pathway. These treatments are used in moderate to severe forms of psoriasis requiring systemic management, after failure or intolerance of conventional treatments and hidradenitis suppurativa in the case of secukinumab and bimekizumab.
Paradoxical cutaneous reactions have been reported with all IL-17 inhibitors. The most common symptoms are psoriasiform (palmoplantar or pustular) and eczematous eruptions.
Desjonqueres et al (poster 245) reported several cases of psoriasiform reactions, particularly in the skin folds, in patients with HS treated with bimekizumab. Histology tended to support an eczematous and lichenoid reaction. Local corticosteroid therapy and methotrexate were proposed and discontinuation was not necessary.
Frédeau et al (poster 231) reported three patients with a similar eruption in the large folds under the breast, but also in the axillary and inguinal folds, for whom histology was again suggestive of eczema; they were taking various treatments for psoriasis (secukinumab, bimekizumab and ixekizumab).
It should be noted that in the SECU-Ped cohort of children with moderate to severe psoriasis treated with IL-17 inhibitors (Communication 022), a few cases of paradoxical eczema were observed with secukinumab (5/139, 3.5%) and ixekizumab (2/21, 9%).
Report written by Nicolas Kluger (dermatologist, Finland) based on:
Anifrolumab is a monoclonal antibody used to treat moderate to severe systemic lupus erythematosus by blocking the type I interferon receptor, an overactive pathway in lupus patients. It has had marketing authorisation since 2022 for systemic lupus with active skin involvement despite standard treatment.
Anifrolumab has rapid and comparable efficacy across the different subtypes of cutaneous lupus: discoid, subacute, acute and chilblain lupus. Efficacy appears to be better in patients with a moderate (rather than severe) CLASI activity score at treatment initiation. However, there are few predictive factors for response, apart from the level of interferon activity and the interferon signature (CO95).
It is administered intravenously (300 mg every four weeks) on an outpatient basis. This raises the question of spacing out infusions in patients in remission. A prospective study (still in progress) aimed to assess the relapse rate during dose spacing. Relapse was noted in a third of cases in a series of 78 patients with a median duration of 11.5 months after the start of spacing (22% at 12 months, with spacing at eight weeks) (CO94).
Le Bellour et al. reported significant efficacy with anifrolumab in a small series of patients with lupus panniculitis (LP). LP is a rare form of cutaneous lupus; it is often resistant to conventional therapies (hydroxychloroquine, oral corticosteroids, methotrexate, etc.). It may be isolated or associated with systemic involvement or other forms such as DL or chilblain lupus. The efficacy of the treatment was noticeable at six months, although some skin sequelae inherent in panniculitis were observed.
These results are encouraging in this form of cutaneous lupus, but the role of anifrolumab remains to be determined.
The main infections associated with anifrolumab are respiratory infections and viral skin infections, in particular herpes.
In the de La Rochefoucaud series, 23% of patients developed an infection, and in the Le Bellour series, 45% developed a viral infection as well as sepsis with a urinary origin.
Mollet et al. reported the case of a 34-year-old woman who developed valaciclovir-resistant chronic genital herpes on anifrolumab and valaciclovir (P186).
Lastly, paradoxical reactions such as psoriasis can occur with anifrolumab. By neutralising the interferon pathway, anifrolumab can disrupt a feedback loop, allowing uncontrolled Th17 hyperactivity and a permissive inflammatory environment for psoriasis, in people with genetic or epigenetic susceptibility to Th17 inflammation (P236).
Report written by Nicolas Kluger (dermatologist, Finland) based on:
Clinically,
Palmar papules are most often associated with anti-MDA5 antibody-positive dermatomyositis (DM) but are by no means specific to this form. Could they be used as markers to identify patients at risk of developing interstitial lung disease? (CO92)
DM can be paraneoplastic and associated with other paraneoplastic syndromes, as in a case of acquired hypertrichosis lanuginosa with a poor prognosis (P345).
On melanin-rich skin, juvenile dermatomyositis (JDM) presents with classic symptoms such as erythema or oedema of the eyelids as well as Gottron papules on the backs of the hands. Emphasis should be placed on the hypopigmented poikilodermic appearance of the trunk, which is particularly noticeable on dark skin and can be disconcerting at first sight. Necrotic lesions appear achromic (P126).
Lastly, periocular/palpebral involvement in DM should not be confused with the fixed, painless, oedema-free periorbital erythema described by Cordel et al. in Still’s disease (P343).
Therapeutically,
Hydroxychloroquine (HCQ) is considered to be effective against the skin damage caused by DM/JDM, either alone or in combination. However, there is little data in the literature and its efficacy varies widely from > 10% to 75%. A multicentre retrospective study compared 57 patients who had received HCQ and 45 who had not. In total, 46% of patients treated with HCQ achieved a complete skin response, compared with 75% in the group without HCQ. In multivariate analysis, only HCQ was significantly associated with a lower rate of complete response. Overall, HCQ appears to be associated with a lower rate of complete skin response. Prospective studies or studies involving larger numbers of patients are needed to confirm these results.
Anifrolumab could be a promising option in severe juvenile forms resistant to conventional therapies (P105).
Report written by Nicolas Kluger (dermatologist, Finland) based on :
Neildez et al. Lymphomes T cutanés au cours d’un traitement par dupilumab : revue systématique de la littérature. CO116
Dupilumab is a human monoclonal antibody that blocks the action of the cytokines IL-4 and IL-13. It is indicated in particular for treating moderate to severe atopic dermatitis (AD), severe asthma, nodular prurigo, eosinophilic oesophagitis, etc.
A few clinical cases and retrospective series have pointed to a possible increase in the incidence of cutaneous T-cell lymphoma (cTCL) in AD patients on dupilumab.
Are these genuine dupilumab-induced cTCL cases, cases unmasked during AD or cases of cTCL misdiagnosed as AD?
A systematic review of the literature carried out by GFLEC and GREAT included 51 studies, consisting mainly of clinical cases (33) with six retrospective cohorts. A total of 547 patients were identified with lymphoproliferation, including 531 who were diagnosed with cTCL and were on dupilumab. The average age of the patients in this group was 58 (47% female), with AD in 95% of cases. cTCL preceded or was concomitant with the diagnosis of AD in 1.7% and 2.9% of cases respectively. A history of atopy was found in 56% of cases. Seventy percent had received systemic treatment, including cyclosporine in 61% of cases and methotrexate in 36%.
In 75% of cases, the cTCL appeared as an aggravation of pre-existing lesions, and in the remaining 25% as the formation of new lesions. The time to onset was nine months after initiation of treatment. In > 70% of cases, there was mycosis fungoides and in > 10%, Sézary syndrome. Retrospectively, five patients were found to have a diagnosis of cTCL prior to initiation of dupilumab, following re-examination of histologic slides. Clinically, the patients presented with erythroderma (23% of cases) and patches of mycosis (12%). Dupilumab was discontinued after cTCL was diagnosed in 75% of cases. For the patients with follow-up, 70% went into remission after treatment and 13% died. There have been cases of spontaneous regression following discontinuation of dupilumab.
Based on this review, an expert consensus was established between the GFELC and GREAT members using the DELPHI method:
All in all, this review of the literature points to a link with patients with late-onset adult AD, with no history of atopy, and with the aggravation of pre-existing lesions. When the bioavailability of IL-13 is increased on dupilumab, this cytokine could bind to the IL13Ralpha2 receptor, which is not blocked by dupilumab, but is over-expressed in certain types of cancer. This suggests that reported cases more likely represent unmasked or previously undiagnosed cTCL. The other anti-Th2 biotherapies used in AD (tralokinumab, lebrikizumab) have a different mechanism to dupilumab, but there is currently insufficient hindsight to rule out a risk.
Report written by Nicolas Kluger (dermatologist, Finland) based on :
Neildez et al. Risque d’événement cardiovasculaire grave chez des adultes traités par inhibiteurs de JAK pour une dermatite atopique : une étude de cohorte nationale à partir du Système national des données de santé. CO117
Several JAK inhibitors are currently available for the treatment of atopic dermatitis (AD). However, an increase in the risk of major adverse cardiovascular events (MACE) observed in patients over the age of 50 with at least one cardiovascular factor who were treated with tofacitinib for rheumatoid arthritis prompted the health authorities to issue recommendations regardless of the indication, including AD.
Using the French National Healthcare Data System, patients > 18 years of age who had received a JAKi (n = 4300) or a biotherapy (n = 23,574) for AD between 2018 and 2024 were identified and each cohort was compared to a general population cohort.
In the cohort of AD patients taking a JAKi, there was no increased risk of MACE (heart attack, ischaemic stroke) compared with the general population. This may have been due to the application of the health authorities’ recommendations, with limited use of the treatment in at-risk patients and with appropriate patient selection. Other foreign studies also have found no link between MACE and the use of JAKis in AD.
An increased risk of MACE was noted in the biotherapy group before initiation of treatment and during the 1st year of exposure, which raises the question of the role of systemic inflammation in severe AD as an independent cardiovascular risk factor.
Report written by Nicolas Kluger (dermatologist, Finland)
Speaker: Prof Marie-Sylvie Doutre (France)
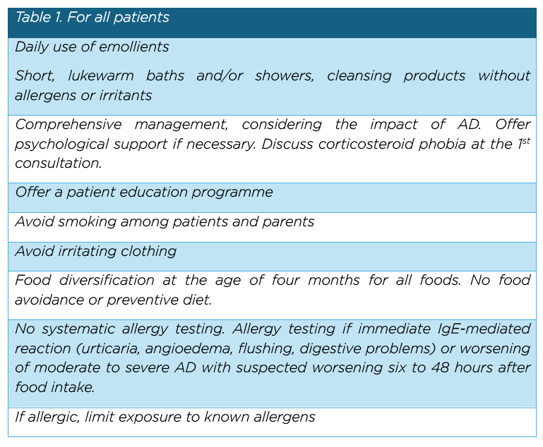
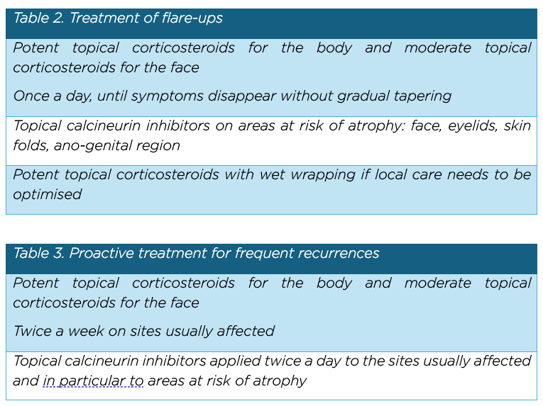
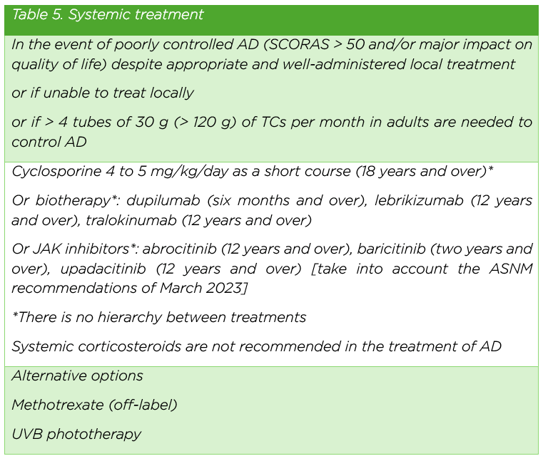
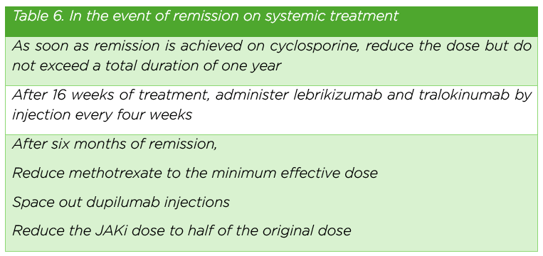
During the Hot Topics session, Prof Marie-Sylvie Doutre presented the new French recommendations for the management of atopic dermatitis (AD), which were developed and adapted based on the European recommendations published in 2022. They were also published in full in the December 2025 issue of Les Annales de Dermatologie et de Vénéréologie - FMC.
Report written by Nicolas Kluger (dermatologist, Finland) based on :
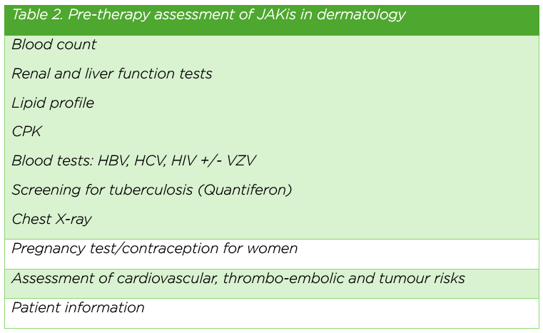
Dereure O. Autres indications, tolérance et suivi. FMC01 Anti-JAK : les dermatologues aussi !
The side effects of JAK inhibitors (JAKis) are frequent, especially with first-generation broad-spectrum “pan-JAK” inhibitors.
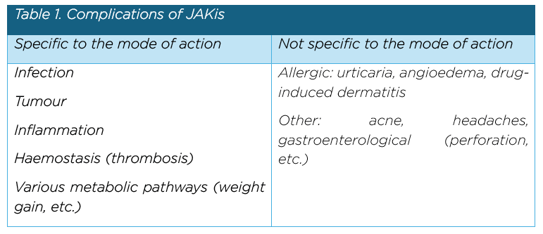
Infectious complications are the most common, particularly with broad-spectrum JAK inhibitors, and include bacterial, viral and fungal infections. However, they are usually benign.
Serious infections include urinary tract infections, digestive tract infections (colitis), skin infections (secondary infection of wounds) and viral infections such as herpes and shingles, which is why it is so important to keep up to date with shingles vaccinations. Live vaccines are not permitted during treatment, and it is strongly recommended that vaccinations be updated before treatment. For vaccination with a live vaccine on JAKis, treatment should be discontinued for three months and resumed one month after vaccination.
To minimise the risk of serious side effects (cardiovascular disease, thrombosis, cancer and serious infections), the Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency has issued the following general recommendations for JAKis and for all chronic inflammatory diseases; they also apply to atopic dermatitis and alopecia.
However, it should be remembered that, at present, patients with AD or alopecia generally do not have the same profile as elderly patients with inflammatory diseases such as rheumatoid arthritis. Furthermore, the literature relating to our populations is reassuring as to the risks of serious morbidity associated with the use of JAKis. Nevertheless, these risk factors should be borne in mind for specific patients (smokers, patients on combined oestrogen-progestin contraception, obese patients, etc.). An article was published in 2024 in Les Annales de Dermatologie et de Vénéréologie - FMC (Staumont Sallé D, et al. Aide à la prescription des inhibiteurs de JAK en dermatologie : évaluation du risque cardiovasculaire et thrombotique veineux et conduite à tenir).
Lastly, in terms of tumours, there is an increased risk of squamous cell skin cancer, mainly in the head and neck region, only with ruxolitinib and exclusively in haematological indications (to date).
Report written by Nicolas Kluger (dermatologist, Finland) based on :
Boccara O. Naevus chez l’enfant. Quand faut-il s’inquiéter ?
Forum FO13 Proliférations mélanocytaires de l’enfant
Olivia Boccara gave a reassuring lecture on naevi in children. It is important to remember that the rules of surveillance as applied to adults in terms of the diagnosis and monitoring of naevi do not apply to children. In fact, childhood is a period when naevi physiologically appear (acquired naevi) and, by definition, are growing, sometimes even from birth. In addition, there is little or no cumulative sun exposure. The appearance of a new naevus is nothing to worry about and its growth, whether in appearance or size, is a normal phenomenon. It should also be remembered that trauma does not increase the risk of melanoma.
The incidence rate of melanoma in 0-14-year olds is 1.74 per 1 million people/year, i.e. 60 times lower than in adults and children aged over 15, according to an American study. SSM is virtually non-existent in children, even though it is “the” type of melanoma in adults. Melanoma in naevi is very rare, especially in children under 10, and melanoma in giant congenital naevi is also uncommon. On the other hand, a child with several dozen naevi needs more attention.
The ABCDE criteria should not be applied to children.
In the latter, melanomas are often raised and unpigmented. They are not irregular and not very wide. An ABCD acronym has been proposed for children: Amelanotic; Bump, bleeding; uniform Colour; De novo, any Diameter. In short, we should be concerned about a recent achromic/erythematous nodule that is growing rapidly. However, even with these criteria, a classic (benign) Spitz naevus can meet them.
Lastly, isolated longitudinal melanonychia in children is almost exclusively benign and simple monitoring is sufficient, with pigmentation that sometimes regresses.
Report written by Nicolas Kluger (dermatologist, Finland) based on:
Focal epithelial hyperplasia (FEH or Heck’s disease) is a benign condition of the oral mucosa caused by HPV infection, mainly types 13 and 32. It mainly affects children and teenagers, but can also occur in adults. It is rare. In Europe, it is common in cases of HIV infection or organ transplantation. It manifests as multiple small, soft, painless, non-ulcerated pinkish or whitish lesions, mainly on the lips, cheeks and tongue. The disease is non-cancerous and often self-limiting, disappearing spontaneously within a few months or years. Diagnosis is usually clinical and is sometimes confirmed by biopsy with HPV PCR for typing. Treatment is not always necessary, and observation may be sufficient, but curettage, cryotherapy, imiquimod or CO2 laser ablation may be proposed for functional or aesthetic reasons.
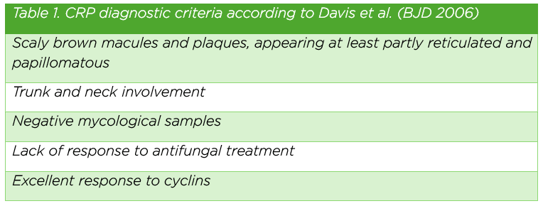
Confluent and reticulated papillomatosis (CRP) of Gougerot and Carteaud is a rare, benign dermatosis that mainly affects adolescents and young adults. It presents as brownish, warty patches that are confluent in the centre and reticulated around the edges and are located mainly on the trunk and neck. Its origins are poorly understood, involving disordered keratinisation and sometimes abnormal bacterial flora. Diagnosis is clinical, ruling out mycosis. Treatment is based mainly on antibiotics (minocycline) or keratolytic agents, with good results.
Facial discoid dermatosis is a rare chronic inflammatory condition mainly affecting the face; it was first described in 2010 by Ko et al. (Int J Dermatol 2010). It presents as rounded or discoid plaques that are erythematous, pink or orange, sometimes scaly, and well demarcated Lesions occur mainly on the cheeks, forehead and chin. They can be pruritic but are often not very symptomatic. Some 40 cases have been described to date. It seems to affect women more frequently. Histology is not very specific, showing psoriatic epidermal hyperplasia, hyperkeratosis with parakeratosis, lymphohistiocytic perivascular infiltrate, follicular plugs, spongiosis and demodex. The aetiology remains poorly understood. Diagnosis is clinical and is sometimes supplemented by a biopsy. Differential diagnoses include discoid lupus, superficial pemphigus and seborrhoeic dermatitis. Treatment is based on topical corticosteroids with or without calcipotriol and acitretin. The condition is generally chronic, with lesions remaining stable for years and with a disappointing therapeutic response. However, it is benign, with no systemic involvement. Its individualisation is not clear. Is this a distinct condition or a specific presentation of psoriasis, seborrhoeic dermatitis or demodecidosis?
Linear lupus panniculitis of the scalp is a rare form of cutaneous lupus that mainly (but not exclusively) affects young men from South-East Asia. It is asymptomatic and progressive, with a linear, annular or arciform distribution, following Blaschko’s lines and affecting any region of the scalp.
It results in non-scarring alopecia with possible regression and regrowth of hair, and rarely with systemic involvement. Antinuclear antibodies are positive in 50-60% of cases. Treatments include hydroxychloroquine, local or oral corticosteroids and even methotrexate.
Prurigo pigmentosa is a chronic inflammatory and pruritic dermatosis that develops in flare-ups. It was described by Nagashima in the 1970s and the condition is well known in Japan and Korea. It tends to affect younger women (aged 11-30).
It has a particular proximal distribution, affecting the neck, trunk, back and shoulders. The initial papular lesions become crusted, giving way to hyperpigmented macules that last for several months. As the disease progresses in flare-ups, lesions of different ages coexist and some coalesce, giving a reticulated appearance. A ketogenic diet, diabetes and anorexia nervosa, as well as friction and stress, are factors that can trigger the disease. Treatment is based on antibiotic therapy with cyclins, macrolides or dapsone.
Cutaneous plasmacytosis is a chronic “haematological” disease that most frequently affects individuals from South-East Asia. It takes the form of macules or papules that are not very specific and are hyperpigmented, asymptomatic and chronic, appearing mainly on the trunk. Skin biopsy shows a perivascular infiltrate of mature plasma cells in the dermis and hypodermis. Biologically, there is an inflammatory syndrome with hypergammaglobulinaemia (more polyclonal than monoclonal). If a second internal organ is affected, with an infiltrate of mature, well-differentiated plasma cells without atypia, the disease is classified as “systemic” plasmacytosis. Obviously, “classic” causes of cutaneous plasmacytosis such as syphilis and borreliosis should be ruled out. In addition, every effort should be made to rule out lymphoma. Plasmacytosis may be associated with Castleman disease, IgG4-related disease, lymphoma, etc. Various treatments can be proposed, including oral corticosteroid therapy, thalidomide and PUVA therapy. This is a disease generally managed in a university setting.
Eosinophilic polymorphic and pruritic eruption associated with radiotherapy (EPPER) syndrome is a rare skin complication associated with radiotherapy. It manifests as a pruritic polymorphic eruption on all four limbs (sparing the head and beginning at the radiotherapy site) that is made up of papules, plaques or vesicles. Blood eosinophilia is frequently observed. Histology shows an eosinophilic perivascular infiltrate in the dermis. The exact mechanism is poorly understood, but an immuno-allergic reaction induced by irradiation is suspected. The syndrome generally appears during or after radiotherapy. It can sometimes be delayed by several months. Treatment is based on topical or systemic corticosteroids and antihistamines. The outcome is usually favourable after treatment, but it may resolve spontaneously.
Accidental exposure to mercury is still possible in France, as illustrated by the case of an auctioneer who developed acute generalised exanthematous pustulosis (AGEP) with pulmonary involvement and an inflammatory syndrome. Exposure to mercury was probably occupational via the handling of antiques.
Report written by Nicolas Kluger (dermatologist, Finland) based on :
Tristan A. Quand Staphylococcus Aureus s’attaque à la peau. Le staphylocoque doré dans tous ses états FMC047
Dr Anne Tristan from the French National Research Centre for Staphylococci outlined the epidemiology, bacteriology and different presentations associated with Staphylococcus aureus toxins.
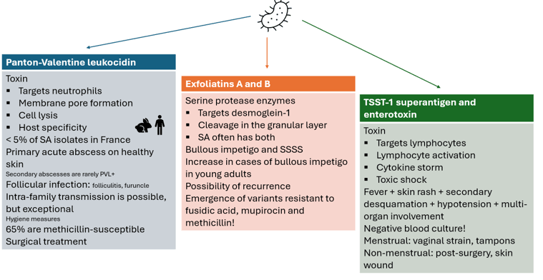
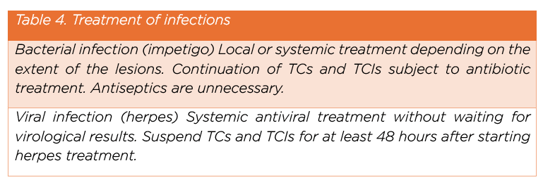
Figure 1. Toxin-mediated clinical presentations of Staphylococcus aureus
Reports written by Ibrahima Traoré (dermatologist, Guinea)
Chair: Fatimata Ly (Senegal)
Speakers: Fatimata Ly (Senegal), Mariem Kebe Dia (Mauritania), Mame Thierno Dieng (Senegal)
Voluntary cosmetic depigmentation (VCD): Background and motivations
Speaker: Mame Thierno Dieng (Senegal)
Mame Thierno Dieng introduced the issue of VCD by briefly tracing its historical background and socio-cultural roots. He explained how this practice, initially limited to certain social groups, has gradually spread in many countries in sub-Saharan Africa.
Key points
Prof Dieng stressed the need to understand the underlying motivations in order to better guide prevention and management strategies, which should include an educational and socio-cultural component.
Infectious complications of voluntary cosmetic depigmentation
Speaker: Mariem Kébé Dia (Mauritania)
Mariam Kébé Dia discussed the infectious complications associated with VCD, focusing on skin immunosuppression induced by the prolonged use of corticosteroids and other depigmenting agents.
Key points
Prof Kébé Dia pointed out that management should combine anti-infectious treatment, discontinuation of dangerous depigmenting products and education about the risks of these practices.
Non-infectious complications of voluntary cosmetic depigmentation
Speaker: Fatimata Ly (Senegal)
Fatimata Ly presented the non-infectious complications, which are often severe and largely underestimated, with a particular focus on the risk of cancer.
Key points
Prof Ly stressed the urgent need to step up the regulation of depigmenting products, improve community awareness and develop appropriate management strategies, including rigorous dermatological monitoring.
Dermatology on black skin: images to help you see more clearly
Report written by: Ibrahima Traoré (dermatologist, Guinea)
Chair: Émilie Baubion (Martinique University Hospital)
Speakers: Émilie Baubion (Martinique University Hospital), Emmanuelle Amazan (Martinique University Hospital), Gladys Ferrati-Fidelin (Martinique University Hospital)
The three speakers offered a session focusing entirely on clinical imaging, with the aim of improving the recognition of dermatoses on black skin, as this is an area that is still poorly represented in traditional dermatological literature. Rather than traditional theoretical teaching, they opted for an interactive approach based on the projection and discussion of numerous clinical photographs, promoting visual learning and diagnostic analysis.
The main objective was to improve diagnostic skills in the face of the multiple dermatological clinical presentations observed on dark skin. The speakers illustrated:
A secondary objective was to point out any particular therapeutic considerations when these diseases occur in black skin, particularly in cases where there is an increased risk of post-inflammatory dyschromia.
Key points
It enabled participants to significantly improve their ability to recognise dermatoses on black skin thanks to the wide variety of clinical examples. The speakers demonstrated the need for specific training for this phototype, and enabled the dermatologists present to gain in diagnostic confidence and therapeutic relevance.