1 professionals
Skin of Color Update 2024 Bioderma Congress Reports
Skin of Color Update 2024 Bioderma Congress Reports
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Dr. Susanna Margaretha Hendrina Kannenberg (Dermatologist, South Africa)
Related topics
Speakers: Valerie M. Harvey, Andrew F. Alexis, and Cheryl Burgess
Valerie M. Harvey, MD, MPH, FAAD
Dr. Valerie Harvey highlighted the ongoing lack of progress in improving diversity within dermatology trials, which continues to exacerbate health disparities. Despite efforts, only 30% of psoriasis trials have demonstrated adequate diversity. Dr. Harvey emphasized the urgent need for more diverse cohorts in clinical studies, which would help rebuild trust and improve access to life-saving treatments for underrepresented populations. Increased diversity will also provide valuable insights for the safe and effective use of medical products across different demographic groups.
In response to this issue, the FDA has drafted a "Diversity Action Plan," which will impact all clinical studies enrolling participants 180 days after the final guidance is published, expected by June 2025.
Dr. Harvey also pointed to the need for improved definitions and instruments to describe skin of color (SOC) in clinical dermatology. She stressed the importance of removing biased SOC descriptors and eliminating gender classification in trials. Additionally, there is a need for better validated tools to measure SOC, moving beyond the outdated Fitzpatrick Skin Type classification. The new tools should be feasible in terms of time, cost, and reliability.
Emerging tools in development include the Eumelanin Human Skin Color scale, the Individual Typology Angle, and the Monk Skin Tone scale, which aim to more accurately assess and represent SOC in clinical trials.
Andrew F. Alexis, MD, MPH, FAAD
Dr. Andrew Alexis recently discussed significant drug approvals that expand the medical dermatology armamentarium for patients with skin of color. Among the notable approvals is the PDE4-inhibitor: Roflumilast 0.3% cream, approved for the treatment of psoriasis in patients aged 6 years and older. Additionally, Roflumilast 0.15% cream has been approved for mild-to-moderate atopic dermatitis (AD) in patients aged 6 years and older with very rapid relief of pruritus (even after only one application). Roflumilast 0.3% foam for the treatment of seborrheic dermatitis in patients aged 9 years and older has also been approved. The foam formulation offers a convenient option for managing seborrheic dermatitis, particularly in areas like the scalp, which can be challenging to treat, especially in patients with SOC. These formulations act as phosphodiesterase-4 (PDE4) inhibitors, which increase cyclic AMP (cAMP) levels, suppressing pro-inflammatory mediators and enhancing the production of anti-inflammatory mediators. Another noteworthy approval is Tapinarof 1% cream, indicated for the treatment of plaque psoriasis in adults. Tapinarof is also in development for atopic dermatitis, showing promise as an innovative treatment for both conditions. Tapinarof is a small molecule topical therapeutic classified as an aryl hydrocarbon receptor (AhR) modulating agent (TAMA). Its proposed mechanism of action involves activation of the AhR pathway, which helps to regulate skin immune responses and reduce inflammation. By modulating this receptor, Tapinarof promotes the production of anti-inflammatory proteins while suppressing pro-inflammatory cytokines, aiding in the restoration of skin barrier function. This mechanism is believed to contribute to its effectiveness in treating inflammatory skin conditions such as plaque psoriasis and, in the future, atopic dermatitis. In the Tapinarof Extension Trial, patients who entered the study with a Physician Global Assessment (PGA) score of 0 (clear skin) experienced a remittive effect lasting an average of 115 days. One of the most commonly reported side effects was folliculitis, occurring in 22.7% of patients. However, it was noted that these were more often hyperkeratotic follicular papules, rather than the typical presentation of folliculitis.
Recent advancements in biologics for dermatological conditions include several notable approvals:
These approvals represent significant progress in expanding treatment options for inflammatory dermatoses, improving patient care and outcomes.
Cheryl Burgess, MD, FAAD
Dr. Cheryl Burgess discussed the unique differences and important considerations in evaluating and treating patients with skin of color (SOC). Key physiological differences in SOC include multi-nucleated and larger fibroblasts, lower skin pH, increased melanosomal dispersion, larger mast cell granules, variable blood vessel reactivity, facial pore size differences, and distinct elastic recovery and extensibility of the skin.
Cultural differences also play a significant role in the aesthetic expectations of patients:
Across SOC groups, common concerns include uneven skin tone, infraorbital dark circles, and skin laxity. Regarding pigmentation, Dr. Burgess highlighted the usefulness of a Woods lamp to determine pigmentation depth, noting that epidermal pigmentation is easier to treat than dermal or mixed pigmentation. She also mentioned that pigment production involves 14 steps, with 3 occurring inside the melanocyte and 11 outside, noting that 10 of these steps can be influenced by topical agents.
Dermatosis Papulosa Nigra can be safely treated using a hyfercator (monopolar low mode set at 4.5 watts). For hyperpigmentation and hair removal, the safest laser for SOC patients is Nd:YAG 1064nm, but it is important to always perform a test area first. IPL should be avoided in SOC.
For treating ice pick scars, multiple punctures with a needle can be an effective alternative to more expensive procedures, with good results in collagen production. Radiofrequency is also safe for all skin types but should be applied carefully and slowly in SOC patients for safety.
Dr. Burgess emphasized the importance of understanding both the biological and cultural considerations to provide effective, safe, and culturally sensitive care for SOC patients.
Speaker: Susan Taylor
Dr. Susan Taylor discussed recent advances in atopic dermatitis (AD) and hyperpigmentation in patients with skin of color (SOC). She emphasized the challenges of diagnosing AD in SOC due to clinical variations, particularly the difficulty in identifying erythema. In SOC, the absence of visible redness can mislead clinicians into thinking the disease is controlled when it remains active. To assist in diagnosis, she suggested checking for itching and whether lesions are raised to the touch. Furthermore, the distribution of AD lesions may differ in SOC patients, with follicular, psoriasiform, and lichenoid presentations being more common.
A significant concern in SOC patients with AD is pigmentary sequelae, which often result from the inflammatory process. While genetic factors have been linked to a higher prevalence of AD in SOC, social determinants of health significantly contribute to the disease's severity and burden. Environmental factors, such as air pollution (with Black populations often living closer to highways), and lower socioeconomic status are associated with more severe and persistent AD. Additionally, Black children are less likely to see a dermatologist for AD but are three times more likely to receive an AD diagnosis during those visits, reflecting poor access to and utilization of healthcare among SOC patients.
Regarding AD pathophysiology in SOC, recent research indicates that loss of filaggrin is not necessarily a primary factor in AD for these patients. Instead, it is thought that T-helper 1 and T-helper 22 inflammatory cytokines dominate the disease process. Additionally, ceramide levels have been found to be lower in African American skin compared to White or East Asian skin, with reduced ceramide/cholesterol ratios in African skin as well. In all cases of AD, maintaining microbial diversity on the skin is also crucial.
Treatment of AD in SOC patients remains largely similar to other skin types, though special attention must be given to counselling and moisturizing skincare alongside prescription medications. An ideal moisturizer should include a combination of emollients, occlusives, and humectants to support the skin barrier. Over-the-counter treatments for itch, such as colloidal oatmeal, pramoxine, and menthol, can also be helpful adjuncts to manage symptoms. To prevent post inflammatory pigmentation in AD wearing a sunscreen is of utmost importance.
Understanding hyperpigmentation in skin of color (SOC) begins with accurately identifying its cause. Epidermal pigmentation includes conditions such as ephelids (freckles), lentigos (including ink spot lentigos), café-au-lait macules, and pigmentary demarcation lines. In contrast, dermal pigmentation examples include idiopathic eruptive macular pigmentation, lichen planus pigmentosus (LPP), erythema dyschromicum perstans (EDP), pigmentary contact dermatitis (also known as Riehl's melanosis), and dermal melanocytosis. Conditions that involve mixed epidermal and dermal hyperpigmentation include post-inflammatory hyperpigmentation (PIH), melasma, drug-induced hyperpigmentation, LPP, and EDP.
As a general approach:
The best results are achieved through a combination of topical agents, oral therapies**, and procedures.
Topical agents commonly used for hyperpigmentation include:
Procedures that can enhance treatment include:
Newer OTC ingredients for treating hyperpigmentation include:
Dr. Taylor emphasized the critical role of photoprotection when addressing hyperpigmentation. It is essential to use a broad-spectrum, mineral-based sunscreen with at least SPF 30 that includes iron oxide (3%) to block visible light. Additional sun protection strategies, such as wearing protective clothing and limiting sun exposure, are also important.
Including an antioxidant in the regimen, such as polypodium leucotomos (the best-studied option), is mandatory, as reactive oxygen species (ROS) contribute to long-standing pigmentation. Dr. Taylor stressed that makeup with sunscreen is insufficient, and applying both a makeup sunscreen and a regular sunscreen does not provide a cumulative SPF effect.
Speakers: Candrice R. Heath, and Brandi M. Kenner-Bell
Drs. Candrice Heath and Brandi Kenner-Bell presented a discussion on challenging pediatric cases
The first case focussed on hair-pulling disorder, formerly known as Trichotillomania. Children engage in plucking, pulling, twisting, and rubbing their hair, with the scalp being the most commonly affected area, followed by eyelashes and eyebrows. The condition affects children from preschool age to adolescents. It is often an unconscious action, occurring during activities such as falling asleep, watching TV, reading, or doing homework. In younger children, hair-pulling may be linked to thumb-sucking, while older children may exhibit compulsive behaviors such as nail-biting or skin-picking. In more severe cases trichophagia may complicate the condition, when it involves ingesting hair, which may lead to the formation of trichobezoars (hairballs).
Suspect this when you see short, broken hairs of different lengths on a normal scalp (not red or scaly). The patch is often an irregularly shaped, single area on front ½ of scalp - never completely bald. It is usually not painful and may give a sense of pleasure.
Referral for a patient with hair-pulling disorder (trichotillomania) is not always necessary. It depends on the severity of the case and the patient’s response to initial interventions. Referral might or might not be needed: if the condition is generally self-limited (especially in younger children), mild cases with episodic hair-pulling that respond well to emotional support and behavioral modification techniques, combined with mild psychological changes (50-75% of cases), and these are manageable without specialized intervention, and cases where there is some evidence of improvement with N-acetylcysteine. Referral should be considered however when severe psychological disturbances are observed (particularly in tweens/teens (~5% of cases), and behavioral interventions alone are insufficient, when there is a need for more advanced treatments such as Cognitive Behavioral Therapy (CBT), if pharmacological interventions (such as tricyclic antidepressants (TCA) like clomipramine or SSRIs) are required due to significant psychiatric comorbidities.
The next case was a boy with tinea capitis. They mentioned that T capitis have been reported in newborns and infants! Trichophyton tonsurans accounts for over 90% of cases in the USA, and it is typically transmitted from humans. Another common pathogen, Microsporum canis, is usually transmitted by cats (more often) and dogs. Asymptomatic carriers are considered a major reservoir for these fungal infections. It is important to screen family members and close contacts, as they may carry and spread the infection without showing any symptoms themselves.
Oral therapy is essential for treating T capitis as the medication needs to penetrate the hair follicle to be effective. Griseofulvin is a common choice, with the dosage depending on the formulation (Microsize: 20-25 mg/kg/day for 6-12 weeks; Ultramicrosize: 10-15 mg/kg/day). Absorption is variable and is improved with a fatty meal, but the long duration of treatment often leads to poor adherence. Griseofulvin is more effective for infections caused by M canis. Terbinafine treatment is only for 2-4 weeks which encourages adherence. More effective for T tonsurans (less effective for M canis). Fluconazole is an alternative oral antifungal for T capitis. Treatment is also for 6 weeks. It is the only oral antifungal approved for children under 2 years old. It has better cure rates compared to griseofulvin some cases. Potential medication interactions but still considered very safe for use in children. Itraconazole is not first line treatment. Can use in pulse dosage regime *as per toenail T unguium (ie; 3 pulses).
The third case was a girl with Central Centrifugal Cicatricial Alopecia (CCCA) – yes it happens in pediatric and adolescent patients! Other scarring alopecias can also occur in children. Breakage of the hair is an early sign. Ask the child/teen about symptoms such and pain, tenderness or itching of the scalp. Treat similarly as adults. With time it will progress to permanent loss of hair follicles so treat aggressively. There is no FDA approved treatment specifically for CCCA. Treatment includes topical and intralesional corticosteroids, oral doxycycline (not under the age 8yrs) and minoxidil (low dose – 2.5mg/day or less – is safe in children). In a patient with chronic scalp pruritus without dandruff think of CCCA. Looking at mom’s scalp may help with an early diagnosis.
During the case presentation, a little boy was shown with an asymptomatic hyperpigmented plaque consisting of follicular hyperkeratotic papules on his cheek. The diagnosis was Follicular Keratosis, also known as traumatic anserine folliculosis, keratotic papular lesions of the chin, or pressure-induced facial follicular papules.
This condition typically affects the chin, jawline, cheeks, or upper lip, mostly in children and young adolescents with brown or black skin. It is believed to be caused by friction or pressure, with cases even reported due to cell phone use.
Treatment options include:
A case of periorificial dermatitis was described. Common in children and young women. Common in children using spacers for inhalation corticosteroids. Blepharitis, conjunctivitis, chalazion, and hordeolum frequently seen with this acneform eruption (no comedones). There is uncertainty of the role of demodex mites. Note: extrafacial involvement of other periorificial sites is possible. Treatment as with adults. (may need prolonged courses of antibiotics – even up to 6 months).
Rosacea can occur in children.
Ended off with some salient points on pediatric chronic skin disorders and stigma. Make sure to get the child’s input on the impact on his/her quality of life and not only the caregiver’s. This was discussed by looking at the impact of vitiligo in particular, but can also be applied to severe acne vulgaris, atopic dermatitis or other chronic skin conditions. In a cohort of 30 vitiligo patients (8-18yr-olds) 90% of the vitiligo group had at least 1 psychiatric diagnosis vs. 20% in healthy controls. There was a statistically significant difference in anxiety in the vitiligo group vs. healthy controls and rates of ADHD (36.6%) was significantly higher than that seen in the normal population (11.3% for ages 5-17 years in United States). (Clin Exp Dermatol 2021; 64(3):519-515). Remember the long-term impact of the skin disease so do not undertreat.
Speakers: Susan C. Taylor, and Amy McMichael
Susan C. Taylor, MD, FAAD
Central Centrifugal Cicatricial Alopecia (CCCA): Two-thirds of cases present with the classical pattern of initially central alopecia that expands centrifugally. However, some typical variants involve not only the central scalp but also frontal, temporal, parietal, and/or occipital areas.
In about one-third of patients, the condition presents atypically, with the most common atypical presentation being patchy hair loss. Other atypical variants include occipital, parietal, frontal, temporal hair loss, and trichorrhexis. These atypical presentations often lead to misdiagnosis or delayed diagnosis, which results in inadequate treatment, contributing to scarring and a significant psychosocial burden.
While CCCA primarily affects women, it also occurs in men and children.
Common dermoscopic features of CCCA include:
Hair shaft variability
Additionally, the top four comorbidities associated with CCCA are:
Lichen Planopilaris: Typically one has 3 variants: classic LPP, Frontal fibrosing alopecia and Lasseur Graham-Little Piccardi syndrome. The clinical course is highly variable (insidious or fulminant). Remember to examine the rest of the body for other features of LP (pre, during or post LPP). Dermoscopic features include perifollicular hyperkeratosis and erythema.
(A tip: CCCA more tender and itching; LPP more burning sensation)
Diagnostic clues for FFA:
Atypical patterns of hair loss with FFA:
Frontal fibrosing alopecia (FFA) can present in a non-inflammatory manner in various locations such as the sideburns, eyebrows, trunk, and even limbs. Lonely hair sign has been reported on the lower limbs. In some cases, FFA may be strictly confined to the eyebrows, with eyebrow loss often being the first clinical sign. In men, loss of sideburns can be the only presenting feature of FFA, making diagnosis challenging when inflammation is not obvious. Compared to White patients Black patients experience more facial pigmentation and more itching, more frontal recession and develop the condition at a younger age. FFA tends to be less scaly in Black patients vs White patients.
Frontal alopecia after botulinum toxin may be confused with FFA although perifollicular scaling and erythema is absent. The features are more comparable with androgenetic alopecia.
Traction alopecia (TA) can affect any part of the scalp but is more common in temporal and frontal hair margins. Get comprehensive styling history. Fringe sign is sensitive and specific for TA (ie: differentiate from FFA). TA has also been described in Sikh male patients and women wearing hijabs. TA may be associated with pain but may also be asymptomatic. Dermoscopy at later stage shows peripilar casts that indicates continued traction. Broken hairs and black dots, as well as the ‘Flambeau sign’ (white tracks resembling a torch in the direction of the hair pull) are also typical. Recommending discontinuation is culturally insensitive. Modification may be more beneficial to the doctor-patient-relationship.
Amy McMichael, MD, FAAD
Dr Amy McMichael presented the talk on the management of scarring alopecias.
First-line treatment for FFA includes topical calcineurin inhibitors (CNI)(they have tacrolimus in oil in US) and JAK inhibitors. Intralesional steroids administered every 4-8 weeks are used to address symptoms, and mid-potency topical steroids, which can be increased to ultrapotent steroids in severe cases, are also recommended.
Systemic treatment options include:
Additionally, switching to physical-blocking sunscreens is advised to minimize irritation, although there is no concrete evidence in the literature.
Second-line treatments include Methotrexate and Nd:YAG laser therapy.
Third-line options include Oral corticosteroids, Ciclosporin, and Pioglitazone.
Combination therapies are strongly recommended to enhance efficacy in managing FFA.
CCCA is often accompanied by TA, and predates chemical relaxers.
Goals of Treatment for Central Centrifugal Cicatricial Alopecia (CCCA) is to halt symptoms (pruritus and pain), to explain the inflammatory and progressive nature of the disease to patients and to minimize traumatic behaviours. Furthermore, recruiting remaining hairs back to health, improving the appearance of hair density and maintaining long-term improvement, focusing on disease stabilization and preventing further progression.
Discuss genetic predisposition, decrease traumatic procedures and refer to support groups (Scarring Alopecia Foundation (S.A.F.) – scarringalopecia.org and Skin of Color Society short film (www.skinofcolorsociety.org).
Check whole scalp: if have features elsewhere on scalp then systemic treatment is a better option. During the inflammatory stage moisturizing anti-dandruff shampoos week as well as topical and intralesional corticosteroids is a reasonable place to start. Goal is to be symptom free.
Post-Inflammatory Treatment for CCCA include firstly long-term topical steroids – to reduce ongoing inflammation. Topical and oral minoxidil is added to prolong the anagen phase and promote hair regrowth. Surgical restoration is an option for patients with stable disease who have minimal hair loss. 5-alpha reductase inhibitors may be beneficial, particularly in addressing underlying pattern hair loss.
Emerging Therapies include Platelet-Rich Plasma (but need to continue standard disease otherwise recurs), Low-level laser light therapy and Nutritional supplementation.
Amy McMichael, MD, FAAD
Dr Amy McMichael continued onto the management of non-scarring alopecias.
Trichorrhexis Nodosa – innate fragility observed in African American patients. May be congenital or acquired. Check for iron and thyroid levels and for nutritional deficiencies. Advise to give the hair a rest; serial trimming of the hair (6-8weeks); use heat protectant products. A moisturizing haircare regimen is advised and includes these steps:
Make sure that the patient is aware of the long wait period.
Androgenetic Alopecia – more than 50% of older men and 15% of postmenopausal women. 2 FDA approved treatments – minoxidil and finasteride.
Treatment: topical minoxidil5%, Low dose oral minoxidil (LDOM); Finasteride 1-5mg/d, PRP, Hair transplantation.
LDOM – much better adherence to treatment. Complications include hypertrichosis vir topical 5% and systemic 15%). Oral minoxidil: 4% had pretibial oedema. Postural hypotension. 3 pericardial effusions described in world literature. Important is to keep in mind that this is a chronic treatment – is like DM medication: if stop it DM will be out of control. So if stop minoxidil hair will fall out again. ‘Minoxidil shedding’ aka ‘dread shed’: happens around 4weeks after commencing minoxidil. Takes around 4-6w to slow down. Doses: Adult female 1,25mg; Adult male 2,5mg; Adolescent female 0,625mg; Adolescent male: 1,25mg.
Alopecia Areata (AA) – SALT score is standardised method for measuring scalp hair loss in AA. Earlier treatment has better outcome. Current approved JAK inhibitors: Ritlecitinib (12yrs+), Baricitinib (adults only; can up titrate and down titrate), Deuruxolitinib (chemically altered form of ritlecitinib; studies only in adults; very recent approval). Differential diagnosis for AA includes CCCA/TA/sarcoidosis/DLE/tinea capitis.
In general, should wash hair at least every 10-14days.
Always consider biopsy to confirm diagnosis.
Speaker: Dr. Andrew Alexis
Dr. Andrew Alexis' presentation on the treatment of acne in patients with skin of colour (SOC) highlighted the unique therapeutic challenges, particularly in managing post-inflammatory hyperpigmentation (PIH) alongside effective acne control. A delicate balance between maximising treatment efficacy and ensuring tolerability is essential. Dr. Alexis emphasised the importance of early initiation and adherence to treatment regimens, with careful attention to the tolerability of active ingredients, vehicle formulations and dosing. He also emphasised the use of appropriate skin care, including pH-balanced, non-irritating cleansers and non-comedogenic moisturisers, to minimise irritation and dryness and ensure optimal outcomes in SOC patients.
He referred to an article he wrote in 2022 in which he collaborated with experts in the field to produce a very useful algorithm for AV management in patients with SOC.
Alexis A, Woolery-Lloyd H, Andriessen A, Kang S, Rodriguez D, Callender V. Racial/Ethnic Variations in Acne: A Practical Algorithm for Treatment and Maintenance, Including Skincare Recommendations for Skin of Color Patients With Acne. J Drugs Dermatol. 1 nov 2022;21(11):s13223‑132214.
He mentioned tazarotene 0.045% and trifarotene (a 4th generation retinoid) as particularly useful (trifarotene with the added benefit of treating PIH).
(In Q&A he mentioned that most topical treatments only need to be on the skin for 2-3 hours to be effective).
He mentioned PAHPI - a validated index for post acne hyperpigmentation (PIH). He also mentioned a new fixed-dose combination of clindamycin phosphate 1.2%/adapalene 0.15%/benzoyl peroxide 3.1% gel showing great promise.
Stein Gold L, Lain E, Del Rosso JQ, Gold M, Draelos ZD, Eichenfield LF, et al. Clindamycin phosphate 1.2%/adapalene 0.15%/benzoyl peroxide 3.1% gel for moderate-to-severe acne: Efficacy and safety results from two randomized phase 3 trials. J Am Acad Dermatol. nov 2023;89(5):927‑35.
Clascoterone cream 1% was also mentioned as a new androgen receptor inhibitor approved for the treatment of acne vulgaris in patients aged 12 years and older. (FDA approved Aug 2020).
Sarecycline is also available in the US and is a narrow-spectrum tetracycline designed specifically for the treatment of acne.
Dr. Andrew Alexis stressed the critical importance of addressing post-inflammatory hyperpigmentation (PIH) from the outset of acne treatment, recommending a combination of adjunctive non-prescription, prescription and physical treatments. He highlighted the promising potential of the latest OTC molecule, 2-MNG, in the treatment of PIH. He also underscored the need for daily sunscreen use as part of a comprehensive treatment approach.
Speaker: Dr. Hilary Baldwin
Dr. Hilary Baldwin discussed the evolving understanding of rosacea in skin of colour (SOC). Traditionally described as a condition affecting women over 40 of Northern European descent, it is now recognised in men, people with SOC and younger populations. The exact incidence and prevalence in these groups remains uncertain. Symptoms such as burning, stinging, itching and skin sensitivity (to products, medications and the sun) are more easily recognised than visible signs. Identifying rosacea in SOC is challenging because erythema is difficult to detect and the index of suspicion is often low. Possible reasons for the lower perceived prevalence include genetic differences (with a calculated genetic contribution of 46%), increased UV protection in SOC, structural and functional differences in the skin barrier, or simply underdiagnosis.
The transition from subtype to phenotype consensus has been highlighted (Tan et al. Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel.
Schaller M, Almeida LMC, Bewley A, Cribier B, Del Rosso J, Dlova NC, et al. Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. Br J Dermatol. mai 2020;182(5):1269‑76.
Don't forget about eye involvement - potential for sight-threatening disease. Other consequences of undetected rosacea include increased morbidity and reduced quality of life, as well as disfiguring flares.
The first step in managing rosacea in patients with skin of colour (SOC) is to actively listen to the patient. It's helpful to give them a mirror and ask them what bothers them most about their skin. Gaining the patient's buy-in is essential as rosacea is a chronic condition that requires long-term management, which can be costly. It's important to manage their expectations and emphasise that results will take time. In addition, care must be taken to avoid drug-induced irritation and post-inflammatory pigmentation, so vehicle selection is critical in treatment planning to maximise both tolerability and efficacy.
Dr. Baldwin highlighted key findings for effective rosacea management in patients with skin of colour, emphasising both efficacy and tolerability. Among topical agents, the best data support the use of ivermectin 1% cream, minoxidil 1.5% foam and microencapsulated benzoyl peroxide 5%, with tolerability improving as rosacea symptoms improve. An important principle is to repair the skin barrier before introducing active treatments.
Dr. Baldwin also advised switching to oral therapies earlier in the treatment process, particularly in moderate to severe cases. Options include subantimicrobial doxycycline, low-dose extended-release minocycline and isotretinoin. As subantimicrobial doxycycline may not be available worldwide, a workaround is to take the drug with food, which reduces absorption by 26%. She also referred to the use of oral ivermectin in highly inflammatory cutaneous and oculocutaneous rosacea, with doses of 3 mg daily for 8 days showing success in managing the condition, based on studies/case reports by Brown et al. (JAMA Dermatol 2014) and Allen et al. (Cutis 2007).
Brown M, Hernández-Martín A, Clement A, Colmenero I, Torrelo A. Severe Demodex folliculorum –Associated Oculocutaneous Rosacea in a Girl Successfully Treated With Ivermectin. JAMA Dermatol. 1 janv 2014;150(1):61.
Allen KJ, Davis CL, Billings SD, Mousdicas N. Recalcitrant papulopustular rosacea in an immunocompetent patient responding to combination therapy with oral ivermectin and topical permethrin. Cutis. 2007;80(2):149–151.
Dr. Baldwin emphasised the importance of proper skin care in the management of rosacea, particularly in patients with skin of colour (SOC), noting that it can improve the condition even without medication. Inadequate skin care can worsen papulopustular rosacea (PPR) and erythematotelangiectatic rosacea (ETR). Good skin care can also improve the tolerability of medical treatments.
For SOC patients with rosacea, Dr. Baldwin recommended a skincare regimen that included
Dr. Baldwin also advised that patients should be taught how to apply make-up properly to avoid irritation. Heavy cosmetics that require scrubbing or harsh make-up removers should be avoided. Patients with background erythema should use foundation with a green tint to neutralise redness. In addition, applying emollients before make-up and choosing products with a matte finish (as shiny ingredients can irritate rosacea) can make a significant difference to the management of the condition.
Speakers: Dr. Andrew Alexis and Dr. George Han
It is now well established that atopic dermatitis (AD) is a heterogeneous disease with variable presentations, particularly in skin of colour (SOC). Unique features in SOC include differences in erythematous manifestations and a higher prevalence of follicular micropapular and papulonodular variants, such as prurigo nodularis-like lesions. In addition, extensor elbow involvement (papules coalescing into plaques; children and adults) is frequently observed in SOC patients with AD. These differences highlight the importance of recognising the different clinical presentations of AD in different skin types.
Quan VL, Erickson T, Daftary K, Chovatiya R. Atopic Dermatitis Across Shades of Skin. Am J Clin Dermatol. sept 2023;24(5):731‑51.
New approval for AD announced by the FDA during the conference: Lebrikizumab (IL13)
The importance of shared decision making was emphasised.
Dr. Han highlighted a remarkable clinical overlap phenotype between psoriasis and atopic dermatitis (AD) in the Asian population. It is believed that these cases are more likely to be psoriasis rather than a co-occurrence of both conditions, which has important therapeutic implications. The recommendation is to prioritise psoriasis-specific biologics over Th2-targeting AD biologics in these scenarios. If targeted therapies prove ineffective, broader-spectrum therapies are recommended to ensure adequate disease control.
They also noted that if patients have elevated liver enzyme levels while on JAK inhibitors, rechallenge may be considered as the elevation doesn't always recur. However, such patients should be monitored more closely during this process.
Speaker: Dr. Amy McMichael
Dr. Amy McMichael presented on psoriasis in skin of colour (SOC), noting a prevalence of 3.7% in the USA. While psoriasis in SOC is generally consistent with typical presentations described in the literature, hypertrophic psoriasis is more commonly observed. Clinical trials involving patients with SOC are currently limited, although efforts are being made to fill this gap, as highlighted in previous discussions.
Key considerations for the management of psoriasis in SOC include:
Speaker: Dr. Ginette Okoye
Dr. Ginette Okoye gave an excellent and practical presentation on the management of hidradenitis suppurativa (HS) in SOC.
She highlighted five key aspects for potential intervention in the management of HS: the hair follicle, the environment, bacteria, inflammation and hormones/metabolism.
Management of episodic flares:
Consider referral to endocrinology. Consider GLP1 agonist.
Refer patients to: www.hs-foundation.org and https://www.hs-foundation.org/educational-videos-for-patients and https://hspatientguide.com/
Speaker: Dr. Ted Rosen
Dr. Ted Rosen discussed an important topic on syphilis, highlighting an alarming increase in all stages of the disease since 2018, particularly in patients with skin of colour (SOC) and congenital cases. In particular, 2-5% of patients with syphilis present with alopecia, and 5% of cases occur in the extragenital area.
He also discussed hypertrophic or vegetative genital herpes (HSV-2), which predominantly affects immunocompromised individuals, especially those with HIV, but can occur with any form of immunosuppression. This presentation may resemble condylomata lata or condylomata acuminata. Diagnosis requires biopsy with immunostaining or viral culture (PCR). These cases may be resistant to standard antiherpetic medications and require a combined treatment approach using acyclovir derivatives together with surgery, cryosurgery or imiquimod.
Speaker: Dr. Ted Rosen
Compared to white patients systemic lupus erythematosus (SLE), dermatomyositis, and scleroderma (PSS) are more prevalent in patients with SOC. In discoid lupus erythematosus, the hypopigmentation often associated with the disease is of particular concern. In scleroderma, the highest rates of renal disease and mortality are seen in black patients. Lichen planus (LP) in SOC has unique features, including a deeper hyperpigmented colour, annular morphology and a higher prevalence of hypertrophic LP. In addition, bullous and erosive LP on the feet is more common in SOC.
Regarding vitiligo, he discussed when and how to consider emergency treatment. Immediate intervention is required when there is rapid progression such as expansion of 1% BSA over 6 weeks, confetti pattern, trichrome vitiligo or Koebner's phenomenon. The treatment protocol includes an oral 'mini-impulse' steroid (dexamethasone 2-4 mg/day, with half the dose for patients under 16) given on two consecutive days per week for 6-8 weeks. Phototherapy also requires time and commitment, with a target of 50 treatments at twice-weekly intervals. Expected improvement can be 25% at 3 months, 50% at 6 months and 75% at 9 months. Best results are expected on the face/neck, with improved results when combined with topical therapy.
Speaker: Dr. Shawn Kwatra
When taking the history of chronic pruritus, key elements to explore include:
Ask about:
During the physical examination, determine whether the pruritus is due to a primary dermatological condition or whether it is pruritus without a primary skin lesion - which would require a systemic investigation and possible screening for malignancy. Remember that skin lesions may be secondary to scratching and not due to an underlying skin condition.
Assess itch intensity at each visit using the Worst Itch Numeric Rating Scale (WI-NRS).
Ruxolitinib, a topical JAK inhibitor, has shown rapid improvement in pruritus, with relief occurring within minutes to hours. In contrast, systemic JAK inhibitors typically provide itch relief within a few days.
Initial screening for JAK inhibitors should include a complete blood count (CBC) with differential, liver and kidney function tests, TB test, hepatitis B and C screening, baseline lipid panel and pregnancy test (if applicable). Follow-up examinations at 1, 3 and 6 months should include a CBC and liver and kidney function tests, with an additional lipid panel at the 3-month mark.
There is some evidence that prurigo nodularis (PN) has a genetic background. In cases where there is no clear association with atopic dermatitis (AD), an 'itch of unknown origin' work-up should be carried out to explore the underlying causes. In addition, PN should be considered in the differential diagnosis of patients presenting with parasitic delusions. In African American patients with PN, the lesional skin often shows greater thickening and tissue fibrosis.
Predictors of response to dupilumab -History of AD and elevated blood eosinophils.
The IL31 blocker nemolizumab, now approved for PN, has a very rapid effect on itch.
Chronic pruritus without identifiable primary skin lesions requires a thorough systemic investigation and malignancy screening. Non-inflamed, non-diseased pruritus may also have neuropathic or psychogenic causes. Basic investigations should include a complete blood count (CBC) with differential, liver and kidney function tests, HbA1c, fasting glucose and thyroid function tests. Further investigations should be guided by specific risk factors and may include testing for HIV, hepatitis B/C, heavy metal levels, vitamin D or B12 deficiency, and stool analysis for ova or parasites.
The most common malignancies associated with chronic pruritus are haematological in nature; therefore, chest x-ray, serum protein electrophoresis (SPEP)/urine protein electrophoresis (UPEP), lactate dehydrogenase (LDH) levels, and lymph node ultrasound may be warranted. Hepatobiliary malignancies require abdominal ultrasound for evaluation. Risk factors indicating a higher likelihood of malignancy include pruritus lasting less than 12 months (with the highest risk seen in those with pruritus lasting less than 3 months), male sex, age over 60 years, history of smoking (current or former), presence of B symptoms and/or liver disease.
In addition, circulating blood eosinophils and immunoglobulin E (IgE) levels may serve as useful adjunctive biomarkers in the assessment of patients with chronic pruritus of unknown origin, and a trial of immunomodulatory treatment may be considered.
Roh YS, Choi J, Sutaria N, Kwatra SG. Itch: Epidemiology, clinical presentation, and diagnostic workup. Journal of the American Academy of Dermatology. janv 2022;86(1):1‑14.
Speaker: Dr. Johanna Harp
Drug reaction with eosinophilia and systemic symptoms (DRESS) or drug-induced hypersensitivity syndrome is a type IV hypersensitivity reaction to drugs. This delayed reaction typically occurs 3 to 6 weeks after starting the offending drug, although it can manifest months later, particularly with allopurinol. DRESS can affect any organ system and although eosinophilia and transaminitis are classic findings, they are not essential for diagnosis. Atypical lymphocytosis may also be present and requires a manual lymphocyte count for accurate identification. Patients may present with hypotension due to eosinophilic myocarditis, along with other symptoms such as a maculopapular rash (resembling a simple drug eruption but usually more pronounced), fever, facial oedema and lymphadenopathy. Corticosteroids remain the mainstay of treatment, usually administered as prednisone at 1 to 2 mg/kg or equivalent. In severe cases, a pulse of Solumedrol (methylprednisolone) 125 to 1000 mg for a few days may be considered. Recent literature has increasingly reported the use of cyclosporine as an adjunctive treatment option.
The duration of treatment for DRESS can vary widely depending on the offending drug and the complexity of the patient's presentation.
Overall, the duration of treatment for DRESS needs to be individualised, with ongoing assessment of organ function and response to therapy. Close monitoring for relapse or flares is essential, as DRESS is a systemic disease that can affect multiple organs over time.
Acute generalised exanthematous pustulosis (AGEP), a type IV hypersensitivity reaction, is characterised by early erythema, particularly in the flexural areas, followed by the rapid development of hundreds to thousands of tiny punctate pustules and ending in a seborrhoeic scale. The rash usually has a rapid onset, appearing within 1 to 2 days of exposure to the offending agent. Common triggers of AGEP include antibiotics, particularly penicillins and cephalosporins, and calcium channel blockers. A notable clinical feature of AGEP is the presence of geographic tongue, although true mucositis is rare. The first-line treatment remains corticosteroids. However, in refractory cases, cyclosporine, TNF-alpha inhibitors and, more recently, anti-IL-17 agents have been reported to be successful. Dr. Harp suggested some clues to aid diagnosis:
SJS/TEN: may be morbilliform early on and tends to be more painful than itchy. It is a type IV hypersensitivity reaction. Typical onset is between 1-3 weeks. Tends to start more centrally on the body with flat atypical targets or vesicles on macules. Less inflammatory on histology; simple epidermal necrosis. Current treatment recommendations (combination of RCTs and Dr. Harp's experience) First line: etanercept or cyclosporine - Dr. Harp tends to favour etanercept from personal experience and based on the RCT by Wang et al - see below ('almost NO side effects that I've seen or reported in the literature'); data suggesting that it may speed time to re-epithelialisation (Typically she gives 2 doses of 50mg 48-72 hours apart. Rarely 3rd dose if still red, new lesions); emerging data for etanercept + steroids or etanercept + IVIG; cyclosporine data cautiously supportive 3-5mg/kg/day; caution in renal disease, hypertension, risk of infection (not IVIG alone; mixed results with high dose steroids alone) Ocular scarring may be more severe in SOC patients. Indication: always ask about pain in mouth, sandpaper or gritty sensation in eyes, burning with urination.
Wang CW, Yang LY, Chen CB, Ho HC, Hung SI, Yang CH, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. Journal of Clinical Investigation. 5 févr 2018;128(3):985‑96.
EMM(ajor): blisters longer than SJS/TEN (extensive disease can be as severe as SJS/TEN) and has a viral>Drugtrigger. Histologically, lesions are more inflammatory than expected in SJS/TEN. More distal distribution - central lesions do not coalesce as in SJS/TEN. Systemic steroids are the mainstay of treatment.
For PIH: high SPF sunscreen (consider tinted version (with 3% iron oxide); consider topical hydroquinone and/or tranexamic acid (topical or oral - ask about blood clot history) and/or azelaic acid topical.
Speaker: Dr. Shawn Kwatra
Seborrhoeic dermatitis affects different age groups, with 60-70% of babies affected (mothers are often concerned about whether their baby will ever have a normal colour - discuss this with parents). Other affected groups include adolescents, young adults and adults over 50. Risk factors include male sex, HIV infection and other forms of immunosuppression, a diet associated with increased levels of Candida in the gut, and conditions such as Parkinson's disease.
Current understanding of the pathogenesis of seborrhoeic dermatitis points to a disrupted lipid bilayer and dysregulation of the skin barrier, increased levels of Malassezia and increased production of pro-inflammatory cytokines.
Seborrheic dermatitis is one of the five most common dermatological conditions in black patients. A common presentation in SOC is hypopigmentation.
Treatment goals include:
The standard of care for seborrhoeic dermatitis prior to 2024 included a variety of treatments aimed at managing symptoms and controlling flare-ups:
A reasonable treatment regimen for a standard case of seborrhoeic dermatitis might include the following steps:
Roflumilast foam 0.3% was approved by the FDA in December 2023 for the treatment of seborrheic dermatitis in patients aged 9 years and older. This approval marks a significant advance in the treatment of this chronic skin condition, particularly with its ease of application to areas such as the scalp.
There are also promising developments in the treatment pipeline, including phase 2 studies for ruxolitinib 1.5% cream (a JAK inhibitor) and another PDE4 inhibitor (PF-07038124 0.02% ointment).
Seborrheic dermatitis remains a complex condition that can have a significant impact on a patient's quality of life. Shared decision making between clinicians and patients is essential. In more resistant cases, clinicians may consider short, repeated courses of systemic antifungals to control symptoms and reduce Malassezia yeast levels, especially when topical treatments are inadequate.
Speaker: Dr. Shari Lipner
Psoriasis is the most common skin disease associated with nail involvement, with 80-90% of patients experiencing nail changes at some point in their lives. In addition, over 80% of patients with psoriatic arthritis also have nail disease. In contrast, only a small percentage (5-10%) of people have isolated nail psoriasis without other skin or joint involvement. It has a significant impact on quality of life. In SOC patients, nail psoriasis tends to be diagnosed at a later stage and is more severe.
She showed a wonderful algorithm for treating nail psoriasis from Rigopoulis D et al.
Rigopoulos D, Baran R, Chiheb S, Daniel CR, Di Chiacchio N, Gregoriou S, et al. Recommendations for the definition, evaluation, and treatment of nail psoriasis in adult patients with no or mild skin psoriasis: A dermatologist and nail expert group consensus. Journal of the American Academy of Dermatology. juill 2019;81(1):228‑40.
Her preferred intralesional steroid solution is 2.5% Kenalog diluted in 1% lidocaine, which she injects with/without a nerve block.
She said that for nail bed psoriasis, lower doses work as well as higher doses and can be injected into the matrix or hyponychium (although more painful). More than 3 nails require systemic therapy combined with intralesional steroid injections. The frequency of injections depends on the patient - give the patient the flexibility to decide.
In nail psoriasis, the response should not be assessed until 12-18 months later.
New studies of biologics for nail psoriasis include brodalumab, tildrakizumab, risankizumab, bimekizumab, deucravacitinib.
Nail lichen planus is a nail emergency - anonychia and pterygium are irreversible. In SOC patients, erythema on the nail plate is difficult to see, onychorrhexis and longitudinal melanonychia (which is of course more physiological) are more common. Nail bed LP may resemble psoriasis.
Speaker: Dr. George Han
When advising an Asian patient, be sensitive to their cultural background.
Speaker: Dr. Jennifer Stein
She made a point to remind the audience that ‘Furrows are fine, but that Ridges are risky’.
In practice ‘ethnic melanosis/mottled hyperpigmentation’ is common in SOC patients. These often have parallel ridge patterns. There is very little in the literature about this and it needs more characterization. As a ‘Take-home message’ she emphasised that a large lesion (larger than 7mm) that is atypical needs attention.
Regarding pigmented lesions on the nail, she agreed that it may be much more challenging. SOC patients often have melanocyte activation, but it tends to be lighter than MM. As special tips she mentioned that a fungus tends to be broader at the periphery but that MM broader proximally (base of triangle at the base). A nevus tends to be narrow, have parallel bands and may have a pseudo-Hutchinson sign. A MM may have multiple, uneven bands and may show pigmentation beyond the nail. If the width of the pigmented band is more than 2/3 of the nail, then be more worried about a MM. A pigmented band less than 1/3 is usually benign (Benati et al, JEADV).
Benati E, Ribero S, Longo C, Piana S, Puig S, Carrera C, et al. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. Acad Dermatol Venereol. avr 2017;31(4):732‑6.
She ended off by advising to look out for one nail that looks different from the rest. She also advised looking at https://dermoscopedia.org to learn more about dermoscopy.
Speaker: Dr. Valerie Harvey
Health inequalities contribute to delayed diagnosis in patients with SOC, leading to increased morbidity and mortality. In this context:
It's also noted that the parallel ridge pattern may be a normal feature in SOC patients.
Dr. Harvey mentioned the following online resources for medical education related to skin of colour:
Speaker: Dr. Maritza Perez
In her presentation, Dr. Perez emphasised a comprehensive approach by targeting different stages of melanin production and transfer. Blocking all the processes has the highest probability of success.
Ingredients with the most evidence of systemic sun protection include polypodium leucotomos and nicotinamide. Sun protection should be topical and systemic, and photosensitising agents (such as HCTZ) should be avoided.
Regarding ageing, she said that SOC patients start ageing 10 years later than white patients.
The pathways & metabolism involved in the production of natural skin antioxidants start to decline from the 20s. In our third decade our mitochondria start to malfunction - replacement with NAD+ and peptides such as Pal-KTTS can address this problem. In our 40s the pathways/metabolism associated with cell senescence begin to increase dramatically. Sun exposure and lifestyle factors such as aerobic exercise and smoking are the main contributors to cellular senescence. In the 50s, pathways and metabolism related to the production of skin barrier building blocks begin to decline. The right emollients and retinoids are important at this stage.
Dr. Perez highlighted the accelerated ageing process after menopause, noting that the rate of ageing increases 6.79 times faster after menopause. This is largely due to the sharp drop in oestrogen levels. Oestrogen depletion has a dramatic effect on the skin:
This significant loss of collagen contributes to noticeable changes in skin texture, elasticity and overall appearance, making the effects of ageing during and after the menopause faster and more visible.
She referred to methylestradiol propanoate (MEP): A New Class of Cosmetic Non-Hormonal Estrogen Receptor Activator (NERA). Unlike oestradiol, MEP is not a hormone with any of the potential risks.
Draelos ZD. A Double-Blind Randomized Pilot Study Evaluating the Safety and Efficacy of Topical MEP in the Facial Appearance Improvement of Estrogen Deficient Females. J Drugs Dermatol. 1 nov 2018;17(11):1186‑9.
Speaker: Dr. Heather Woolery-Loyd
In SOC patients, facial lines are less pronounced due to a thicker and more compact dermis. However, they are more prone to dyspigmentation (uneven pigmentation) due to the difference in concentration of epidermal melanin. Dr. Woolery-Loyd referred to a study showing that skin colour distribution can account for up to 20 years of perceived age.
The main site of UV filtration in Caucasian subjects is the stratum corneum, whereas in black patients it is the stratum basale and stratum spinosum. UVA and visible light (especially blue light) are the major contributors to pigmentation in SOC patients.
All skin types need sunscreen, but for different reasons.
Tanaka et al showed that iron oxide pigments have different efficacy in blocking different types of radiation. Key findings from iron oxide research include:
They concluded that dark iron oxide combinations are particularly effective at blocking UV, visible light and near-infrared radiation, providing a broader spectrum of protection than lighter shades. (Tanaka, Yohei, Richard Parker and Amaryllis Aganahi. "Photoprotective ability of coloured iron oxides in tinted sunscreens against ultraviolet, visible light and near-infrared radiation". Optics and Photonics Journal 2023; 13(8):199-208).
Regazzetti, Claire, et al. Melanocytes sense blue light and regulate pigmentation by opsin-3. Journal of Investigative Dermatology 2018;138(1):171-178. This article has also been cited to show the importance of blue light in the development of pigmentation.
With regard to antioxidant sunscreens, she showed that they provide protection equivalent to tinted mineral sunscreens against UVA1 and visible light. Finally, she referred to the new Australian sunscreen recommendations, which balance the risk of sun exposure with the risk of vitamin D deficiency due to insufficient exposure.
Neale RE, Beedle V, Ebeling PR, Elliott T, Francis D, Girgis CM, et al. Balancing the risks and benefits of sun exposure: A revised position statement for Australian adults. Australian and New Zealand Journal of Public Health. févr 2024;48(1):100117.


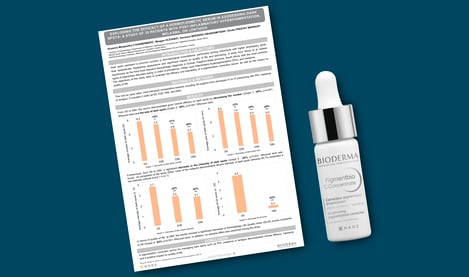
Exploring the efficacy of a dermocosmetic serum in addressing dark spots: a study of 39 patients with post-inflammatory hyperpigmentation, melasma, or lentigos


Bioderma Congress Reports ESPD 2024

Bioderma Congress Reports EWMA 2024