5 professionals
Laëtitia, 26 years old. Pain during sexual intercourse.
Laëtitia, 26 years old. Pain during sexual intercourse.
Reviewed by Dr. Alexandre, dermatologist
Related topics
True answer!
Wrong answer!
After tests :
True answer!
Wrong answer!
True answer!
Wrong answer!
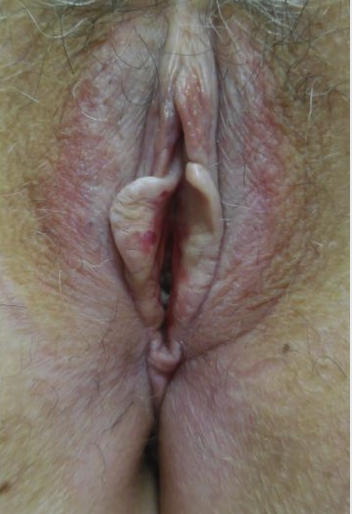
Lichen sclerosus
Following the clinical diagnosis, the diagnosis of inflammatory vestibulitis caused by vaginal dryness of hormonal origin (a type of vulvodynia) was confirmed.
Aim to relax the perineal and pelvic muscles, as pain leads to contraction, which then increases the pain. Such therapy sessions can also include TENS (gentle electrostimulation for pain relief; devices may be recommended for self-treatment in severe forms or cases that have been chronic for more than 3 months).
Innovative therapies such as radiofrequency or biophotomodulation can also be used to improve dryness (action on the Skene and Bartholin glands and the vaginal mucosa).

Piriformis stretching: pain reduction
By stretching your piriformis muscle, you’ll reduce literally all pain, especially sciatica and lower-back pain. It also helps to reduce stiffness in the back of the legs, buttocks, hamstrings, and potentially the calf muscles.

The butterfly:
Butterfly stretching helps to open up the hips and thigh, and improves flexibility. This stretch targets the groin, relaxing and lengthening the thigh muscles (adductor). The adductors are often neglected during training sessions, but they play an essential role in your stability and balance.
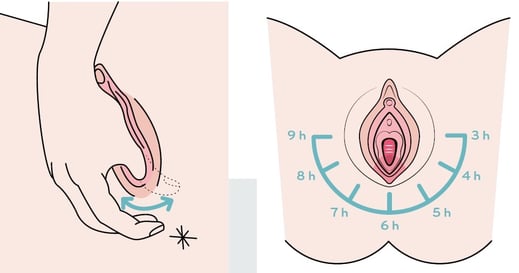
Self-massage during application of moisturizing/soothing creams:
Two fingers, making small circles with as little pressure as possible around the vulva.
Gentle pressure from the edge of the vulva outwards in a star shape from 3 o’clock to 9 o’clock.
To reduce over-stimulation of the sympathetic nervous system linked to stress and pain, and reactivate the parasympathetic nervous system:
Vulvodynia cannot be prevented because its cause is unknown, but it is sometimes possible to prevent the associated pain.

Antifungal medications should not be prescribed repeatedly, particularly in the event of a recurrence.
Non-medicinal treatment guidelines are of crucial importance regardless of the care given based on aetiology: external cleansing with intimate cleanser, no excessive cleansing (in particular, no intra-vaginal cleansing), no complete hair.

Clinical diagnosis using the cotton swab test.
Make treatment for vaginal dryness a priority.
Pain should be taken into account and analgesics (local and/or systemic) and additional treatment adapted as soon as possible; after 3 months, the pain will become chronic and its management even longer and more complicated.

Not every unpleasant sensation in the vulva is a fungal infection.
When symptoms recur, an examination is essential.
Beware of prescribing antifungal suppositories or of self-medication without a diagnosis.
The vaginal flora must be preserved.

Not all vulvodynia is caused by fungal!
Create easily your professional account
I create my accountGet access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations