1 professionals
Toxidermia: Clinic, diagnosis and treatment
Toxidermia: Clinic, diagnosis and treatment
Medical review by Dr Pierre Schneider, Dermatologist, Saint-Louis Hospital, France
Related topics
Immunological toxidermia can be mediated by two different mechanisms1 :
The most frequent forms1,2:
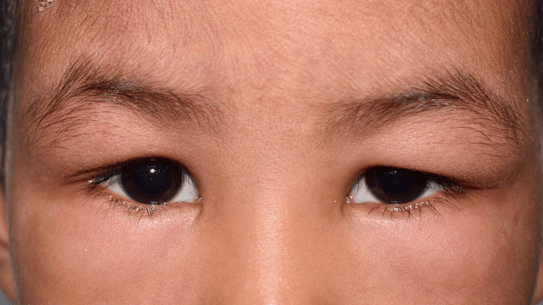
Fig: Fixed erythema pigmentosum

Rare. Recognized by several criteria:
Fig 1,2,3: DRESS Syndrome


Among the drugs implicated in DRESS, the most frequently suspected are:
Fig 1: Stevens-Johson Syndrome; Fig 2: Lyell-TEN Syndrome


The mortality risk for this toxidermia is high: 4.8% for SJS, 19.4% for SJS-TEN overlap and 14.8% for TEN6. Re-epidermalization occurs within 10 to 30 days, with frequent sequelae: pigmentation disorders and mucosal scars, especially in the eyes (synechiae).
Epidemiological case-control studies conducted in Europe by EuroSCAR2 have identified the drugs responsible for Stevens-Johnson syndrome and toxic epidermal necrolysis, namely antibacterial sulfonamides, allopurinol, carbamazepine, phenobarbital, phenytoin, non-steroidal anti-inflammatory drugs of the oxicam family and, to a lesser extent, nevirapine, lamotrigine, sertraline, pantoprazole and tramadol6.
Fig 1,2: Acute urticaria
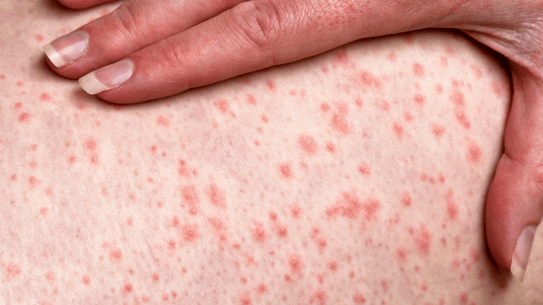

Superficial and/or deep urticaria may, in rare cases, be associated with an episode of anaphylaxis.
Rash occurring within hours of exposure to the sun. Localized on the exposed areas: photodistribution.
It depends on two distinct mechanisms:
2. Phototoxicity
It occurs in the hours following sun exposure.
Diagnoses are most often clinical, but additional biological tests may be performed in some cases.
As toxidermia manifests itself in multiple forms depending on the individual and the drug, each reaction has its own differential diagnosis. The main differential diagnoses referenced concern immunoallergic toxidermia.
These rashes can also have an infectious origin: in children, 70 - 80% of exanthemata have an infectious cause.
Generalized pustular psoriasis characterized by a less abrupt onset, more prolonged evolution and the need for a history of psoriasis.
Must be differentiated from other pathologies such as:
These three elements make it possible to determine the therapies involved and to proceed to their immediate interruption. These drugs are contraindicated for use by this patient.
Hospitalization in a specialized care center for specific treatment.
Antihistamines, local corticosteroids and sometimes general corticosteroid therapy (erythroderma and DRESS).
More than 90% of toxidermia is benign. Only 1/10,000 to 1,000,000 are life-threatening.
Can toxidermia affect the pregnancy? Can it have an impact on the delivery or the child?
Should I contact the doctor?
Does toxidermia occur every time I take medication?
Is an appointment with an allergist necessary?
Can a simple toxidermia reveal a higher risk of developing severe toxidermia?
Is toxidermia usually triggered by the first dose or by the 2nd or 3rd?


Contact dermatitis: Clinic, diagnosis and treatment
Create easily your professional account
I create my accountGet access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations