2 professionals
Bioderma Congress Reports IMCAS 2025
Bioderma Congress Reports IMCAS 2025
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Dr. Ana Reymundo (Dermatologist, Spain) and Dr. Lidiya Todorova (Dermatologist, Bulgaria).

Related topics
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Chairs: Dr. Editta Buttura Da Prato (Facial Plastic Surgeon, Italy); Dr. Diala Haykal, MD (France)
The session ended with a discussion of the best aesthetic practices that should be implemented with regard of the generational differences.
Speaker: Dr Diala Haykal (France)
As an introduction to her lecture, Dr Haykal discussed that Generation Z and Alpha have grown up very exposed to the influence of social media. They are the first generations to have had the internet since childhood. This greatly influences standards of beauty, body image and self-perception.
Then Dr. Haykal started discussing the difference in generations and skin care practices that Generation X, Millennials, Generation Z and Generation Alpha are currently applying and specifically how the years they were born impact on the skin care routines and aesthetic procedures they are seeking, as well as the results they are aiming to achieve in terms of their perception of beauty standards.
She cleared out the different beauty standards in beauty in generations as well as generational shifts, pointing out that:
Coining out the term “prejuvenation”: it is a ten-year-old term that is defined as a way to seek active ways to prevent signs of aging in early age in order to preserve natural beauty. This “approach” in aesthetics is mainly influenced by social media (SM) and all the skin care practices that are shown in different SM platforms. However, non-professionals recommending skin care products and procedures may result in the creation of dangerous treatments. Therefore, there is a strong need for education on what truly works and what doesn’t. The goal should be an embrace in diversity and protection from misinformation that is delivered though SM, as well as to bring about body positivity, and the responsibility to make informed decisions.
Time spent on social media can trigger dysmorphophobic disorders and obsessive thoughts related to physical appearance. This has also led to a growing interest in the use of skincare by younger and younger people, and the use of unsuitable treatments can be worrying (see Figure 1.) We should help young people to have the tools to critically evaluate the content they consume on social media in order to avoid social pressures and the use of treatments that are often unnecessary.

Figure 1. This is an advertisement to raise awareness that skincare is not necessary for children
Dr. Haykal emphasized the responsibility of medical practitioners to address the following concerns:
To equip young individuals with critical skills for evaluating social media content and ensuring safety, Dr. Haykal proposed a collaborative effort involving healthcare professionals, parents, policymakers, industry leaders, IT developers, cultural consultants, and educators.
Aesthetic providers should take responsibility for their output on social media, because they have an invaluable expertise and can combat misinformation and offer insights in cosmetic procedures. They can also highlight potential risks. In their hands is to launch awareness campaigns of the safety practices in cosmetic dermatology and necessity of age. A great role in the protection of Generation Alpha would be played by their schools and the information imbedded in the school curricula. The industry’s role in protecting Gen Alpha is to determine how marketing is being done, which impacts the cosmetic trends among the young individuals. For example, currently industry companies are producing campaigns that raise awareness of the harmful trends published out on SM.
Conclusions:
To go further, Dr Haykal suggests referring to the following article: Haykal et al., Educational strategies to combat harmful cosmetic dermatology trends in Generations Alpha and Z, https://doi.org/10.1016/j.clindermatol.2024.05.004
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Khaled Othman (Consultant in dermatology, andrology and aesthetic medicine, UAE)
Dr Khaled starts his presentation by pointing out that prejuvenation is a trend from 2021. Prejuvenation is about preventing the appearance of aging from an early age, using minimally invasive techniques with the prospect of not having to correct the signs of aging later on with more invasive techniques. This trend also affects men and is influenced by social media. A worrying thing is that 85% of the prejuvenation content being consumed comes from non-healthcare professionals.
Studies show that Gen Z is engaging in aesthetic treatments at an earlier age compared to previous generations. Their premature aging is influenced by unhealthy lifestyles, stress, and constant exposure to digital screens. In fact, over the past 5 years there is a 92% increase in dermal fillers and a 236% rise in neurotoxin procedures among millennials and GenZ.
Key Aesthetic Concerns of Gen Z:
The holistic approach combining diet, mental health, exercise, and skincare is now emphasized to enhance overall well-being. Several innovative treatments are revolutionizing the field of prejuvenation for Gen Z:
Dr Khaled also posed on some growing issues in the industry:
Looking ahead, the industry is focusing on safer, more natural approaches, such as:
Men are most concerned about hair loss, but there is also a growing trend in demand for the use of fillers and botulinum toxin, as well as improving skin quality through the use of topical products, peels and lasers. In these groups it is important to get good advice on which treatments are needed, and which are not.
Conclusions:
To go further, Dr Khaled suggests referring to the following articles:
Haykal et al., Prejuvenation: The Global New Anti-Aging Trend, https://doi.org/10.1093/asjof/ojad061
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor David J Goldberg (USA)
Professor Goldberg has made a classification of the different generations to distinguish the concept of prejuvenation, which is more typical of the Alpha and Zeta generations who were born with access to the internet from a young age (Figure 2.). They are characteristically more concerned with how they look in a photo than how they are in reality. Millennials also care about their image and embrace the concept of prejuvenation, but also of using corrective treatments when they are older.

Figure 2. Segmentation of “generations” by age/birth year.
Professor Goldberg also goes back on the definition of prejuvenation, coined by Ken Arndt in 2013: the use of skin care and non-invasive cosmetic treatments to prevent or delay signs of aging. It is a proactive approach that values prevention over correction to maintain or enhance youthful aesthetic features, typically through topical regimen and cosmetic procedures. This trend as previously mentioned is very much influenced by social media. It focuses on the use of wrinkle-preventing skincare, baby botox, skin booster and the use of laser with low downtime.
Traditional rejuvenation is more typical of generation X and baby boomers. They already have damage, and it is a matter of correcting it. Therefore, it is more typical to use ablative lasers such as CO2, fillers or even surgery (Figure 3.).
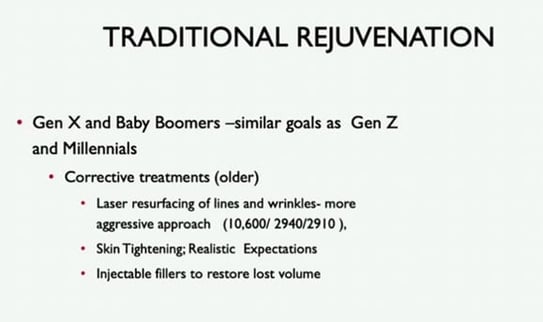
Figure 3. Traditional rejuvenation techniques and target groups.
Prof. Goldberg concludes that some people say both approaches look alike, but they have nothing to do with each other. One is about doing less invasive procedures to prevent ageing, and the other is about correcting ageing when it is already present.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor Maria Jose Pelli (Dermatology, Argentina)
Cosmeticorexia, primarily affecting females aged 8 to 17, is a compulsive obsession with cosmetics and skincare, influenced by social and cultural factors. Although not yet officially recognized as a mental disorder, it presents both dermatological and psychological challenges. The condition has gained attention due to increased screen time during the COVID-19 pandemic, social media influencers, the cosmetic industry, and unrealistic beauty standards. Early diagnosis and intervention by healthcare professionals, along with parental guidance, are crucial in the prevention and management.
What is cosmeticorexia?
It is the compulsive use of cosmetics and/or home-made products as a result of social and cultural influences, which may be a sign of underlying compulsive or dysmorphic disorder. The condition predominantly affects young females between the ages of 8 and 17. Dr. Pelli explained that the condition involves obsession with appearance, excessive skincare regimens, and significant expenditures on cosmetic products. The condition is not yet recognised as a mental disorder.
As an example, Dr. Pelli, shared a case from her practice of a 12-year-old female patient suffering from acne exacerbated by excessive at-home cosmetic treatments. The lesions were irritative and itching. Psychological evaluation revealed compulsive tendencies and anxiety related to beauty. With this case, the speaker underscored the necessity of addressing both dermatological and psychological aspects when treating cosmeticorexia.
Key aspects of cosmeticorexia
Dr. Pelli continued the lecture by identifying the three major aspects of cosmeticorexia:
Patients with cosmeticorexia often suffer from:
Cosmeticorexia may be an early indicator of mental health conditions, including:
Why is cosmeticorexia an emerging issue?
Several factors have contributed to the emergence of cosmeticorexia as a widespread issue:
How can doctors identify cosmeticorexia? How can it be effectively treated and prevented?
Dr. Pelli outlined key indicators for doctors to suspect cosmeticorexia in young patients:
The management of cosmeticorexia requires a dual approach:
Prevention starts at home, with parents playing a crucial role in guiding their children:
If not identified and addressed properly on time, young females suffering from cosmeticorexia will probably become demanding patients, who are never satisfied and ask for more treatments than they need.
In conclusion, with the growing influence of social media, societal pressures, and aggressive cosmetic marketing, young females are increasingly vulnerable to developing obsessive skincare behaviours. Therefore, doctors should be aware of the emerging cosmeticorexia. Early identification, professional intervention and parental guidance are essential in the prevention and management of the condition.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor Raheleh Sarbaziha (USA)
The aim of this talk is to discuss what peptides are, which peptides are available on the market for injections and FDA regulation. Peptides are short chains of amino acids that act as signaling molecules in the body. They are gaining popularity in aesthetic medicine for their ability to stimulate cellular processes for regeneration, repair and antiaging.
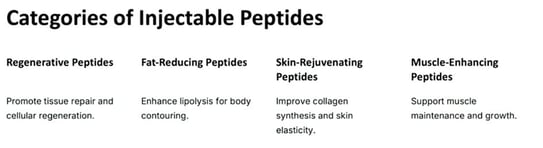
Figure 4. Most famous injectable peptides.
It is important to know which peptides are legal in one’s country of practice and be careful with the protocols to be able to combine them. It is important to educate the patient because many are subcutaneous and will have to be administered at home. Professor Sarbaziha has been using them for 5 years and has never had any problem or analytical alteration.
Here are her key takeaway messages on the topic:
The field of injectable peptides in aesthetic medicine is growing, with ongoing research expanding their therapeutic potential and optimizing formulations for targeted applications.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Franck Bonnier (France)
Dr Bonnier spoke of an ongoing research project to assess ageing with imaging techniques such as ultrasound and OCT. The combination of techniques provides more data.
Key points:
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor Rym Benmously Mlika (Tunisia)
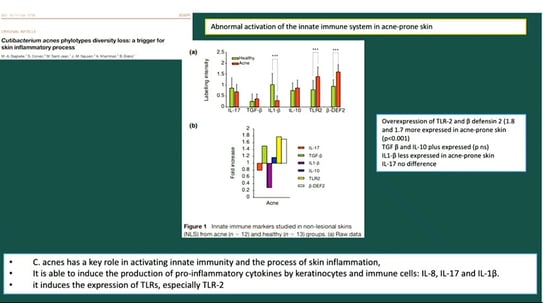
Recent studies have highlighted new factors involved in the pathogenesis of acne such as cutaneous dysbiosis with predominance of Cutinobacterium acnes phylotype IA1 which is a trigger for activation of innate immunity and impairment of barrier function.
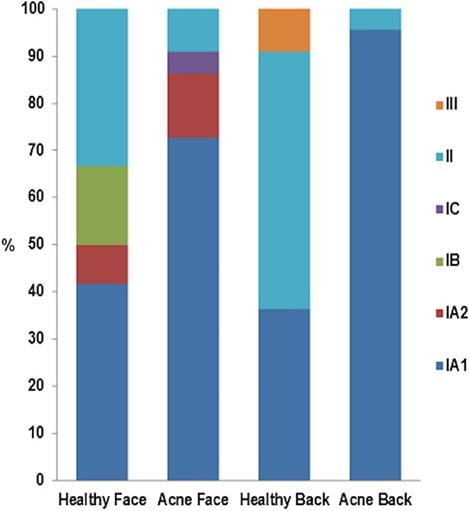
Figure 5. from Dréno et al., The Skin Microbiome: A New Actor in Inflammatory Acne (doi: 10.1007/s40257-020-00531-1). Dysbiosis is related to the loss of diversity of C. acnes phylotypes on the face and back of acne patients [13]. Phylotype IA1 (in dark blue) is abundant in acne skin. Reproduced from [13], with kind authorization from Acta-Dermato-Venerealogica, under the creative commons licence (Attribution-NonCommercial 4.0 International, CC BY-NC 4.0).
Figure 6. From Cutibacterium acnes phylotypes diversity loss: a trigger for skin inflammatory process
She has also highlighted other known factors such as sebaceous hyperfunction and follicular hyperkeratosis.
Speaker: Dr Iñigo de Felipe (Spain)
Dr de Felipe highlighted the role of lasers in the treatment of active acne and their concomitant use with medical treatment.
Classical guidelines do not include lasers in the management of acne, only oral and topical treatment. The most widespread treatment is the use of isotretinoin at high doses. Even so, when treatment is discontinued, 32% of patients have a relapse of acne.
Dr de Felipe has treated patients with isotretinoin and YAP 1340 nm Neodymium laser (4-5 sessions) and in a long-term follow-up (5 years) no relapses have been observed. In their practice, out of 17540 patients treated with low dose isotretinoin and 1340 nm/IPL laser only 6.75% relapsed after 12 months.
Conclusions:
Speaker: Professor Victor Gabriel Glatici (Romania)
Prof. Glatici has highlighted the role of lasers in the treatment of acne. They serve to control Cutibacterium acnes overgrowth, reduce sebum production (by destroying or minimising the number of sebaceous glands), modulation of hair follicle keratinisation, immune and inflammatory response. Combination of lasers with medical therapy offers the best results in the treatment of acne. (Thiboutot D, Gollnick H, Bettoli V et al. New insights into the management of acne: an update from the global alliance to improve outcomes in acne group. J Am Acad Dermatol 2009; 60:51-60).
Laser and light-based acne treatments can be an alternative to medical treatment for non-responders and are associated with minimal adverse effects. These devices also offer an option for those patients who have moderate to severe acne but are concerned about oral medications because of potential adverse effects.
Before doing any treatment, you have to make a good assessment and adjust well the expectations of the patient by telling them the number of expected sessions and the expected results. It is important to study everything that has been published with the device you have in the clinic and to know everything about your patient.
Speaker: Dr Asma Sioud (Tunisia)
This is a fantastic review of the use of lasers for acne with an emphasis on the new 1726 nm lasers with an affinity for the oil gland and those more specific for high phototypes (Goldberg DJ, Andriessen A, Bhatia AC, et al. Treatment of mild to severe acne with 1726 nm laser: A safe alternative to traditional acne therapies. J Cosmet Dermatol. 2023;22(11):3026-3032. doi:10.1111/jocd.15964).
Table 1. Summary of light-based procedures that have been used for inflammatory acne. Extracted from (Goldberg DJ, Andriessen A, Bhatia AC, et al. Treatment of mild to severe acne with 1726 nm laser: A safe alternative to traditional acne therapies. J Cosmet Dermatol. 2023;22(11):3026-3032. doi:10.1111/jocd.15964).
| Device | Mechanism of action | Side effects |
|---|---|---|
| Fractional CO2 laser | Photothermolysis of sebaceous glands | Pain; erythema; bleeding; transient PIH |
| Potassium titanyl phosphate (KTP) laser | Thermal injury to sebaceous glands; reduction of C. acnes | None reported |
| Pulsed dye laser (PDL) | Targets dermal blood vessels; increases growth factor | Pain; erythema; edema; peeling; crusting; blistering; transient PIH |
| 1064 nm Nd:YAG Infrared laser | Destroys sebaceous glands; reduces perifollicular stratum corneum; reduces inflammation | Erythema; dryness; burning; crusting; transient PIH |
| 1450 nm Nd:YAG Infrared laser | Destroys sebaceous glands | Erythema; edema; transient PIH |
| 1540 nm infrared laser | Destroys sebaceous glands | Erythema; edema; heat sensation |
| 1565 nm nonablative fractional laser | Destroys sebocytes; reduces C. acnes | Erythema; edema, crusting; transient PIH |
| 800 nm diode laser with gold microparticles | Selective destruction of pilosebaceous infundibulum and glands with gold-coated silica microparticles with strong absorption at 800 nm | Erythema; overall well-tolerated |
| Blue light 407–420 nm | Photoactivation of bacterial porphyrins; reduces C. acnes; reduces inflammation | Erythema; stinging |
| Red light 620–700 nm | Anti-inflammatory effects | Few side effects by itself; mild to severe discomfort following use of a topical sensitizer |
| Intense pulsed light (IPL) 400–1200 nm | Photothermolysis of sebaceous glands; activation of bacterial porphyrin; reduces C. acnes | Transient PIH; can worsen nodulocystic lesions |
| Photopneumatic therapy (IPL with suction) | Expels comedones with suction; thermal destruction of follicles; reduces C. acnes | Erythema; edema |
| Photodynamic therapy (PDT) after application of topical aminolevulinic acid (ALA) or methylaminolevulinate (MAL) | Destroys sebaceous glands; reduces C. acnes; reduces inflammation | Pain (intolerable with ALA 20%); erythema; edema |
There are many lasers and light treatments that can be used in skin of color. The 1726 nm laser is the best option to treat acne in all phototypes. Because the peak absorption of the sebaceous gland is between 1700 and 1720nm, the 1726 nm laser is really specific for treating the sebaceous gland but is really expensive (Goldberg D, Kothare A, Doucette M, et al. Selective photothermolysis with a novel 1726 nm laser beam: A safe and effective solution for acne vulgaris. J Cosmet Dermatol. 2023;22(2):486-496. doi:10.1111/jocd.15602).
Many others may be used: We must adapt the wavelengths to the skin of color.
Dark skins à IR lasers are safer. Lasers remain absent from recommendations of the 1st and 2nd line acne treatment options.
Further studies should be continued not only for that but also to include the skin color.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor Leonardo Marini (Italy)
We can use laser and energy-based devices to treat scars. Indeed, laser & light can interact with wound healing in different ways and during the various stages of wound healing. The best treatment approach is always a personalized combination strategy since each scar and each patient are unique. The best time to intervene is as soon as possible (Figure 7).
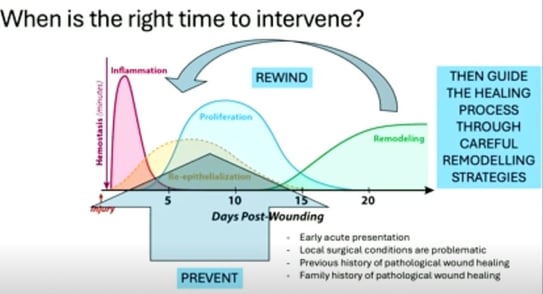
Figure 7. Illustration of when lasers should be best used to improve healing.
In his lecture, Professor Marini described the use of fractional picosecond and nanosecond lasers in the treatment of scars. These are short pulse devices with a fractional lens. They create laser induced optical breakdown (LIOB) in the skin by stimulating the generation of collagen (Figure 8).
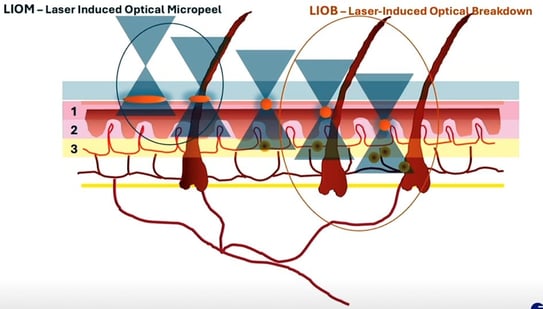
Figure 8. Difference between laser-induced Optical micropeel and breakdown.
In the treatment and prevention of keloids and hypertrophic scars, Prof. Marini combines it with corticosteroids and imiquimod (Figure 9).
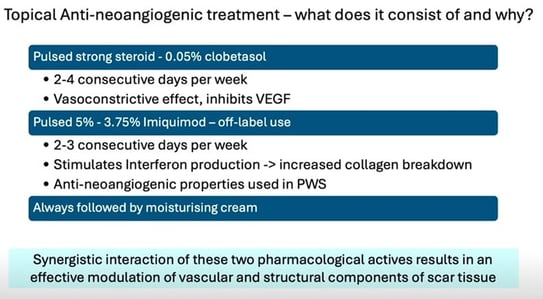
Figure 9. Protocol proposed by Professor Marini
He also combines it with hyper diluted botulinum toxin A (BTX) in order to reduce the tension of the scar at the periphery of it.
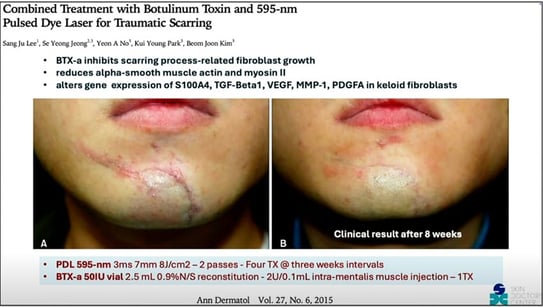
Figure 10. From Lee SJ, Jeong SY, No YA, Park KY, Kim BJ. Combined Treatment with Botulinum Toxin and 595-nm Pulsed Dye Laser for Traumatic Scarring. Ann Dermatol. 2015;27(6):756-758. doi:10.5021/ad.2015.27.6.756
Conclusions:
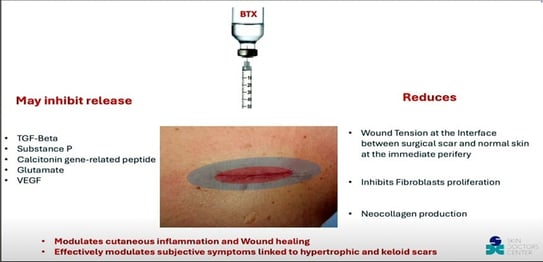
Figure 11. Benefits of BTX in scar management.
Speaker: Dr Brian Hibler (USA)
Dr Hibler’s lecture was about how to treat scars if you don’t have lasers or energy-based devices. The adequate use of sunscreen to prevent hyperpigmentation, proper cleansing of the scar to prevent infection and the use silicon gels are recommendable. In the cases of hypertrophic scars and keloids intralesional drugs such as corticosteroids and 5-FU can be used to control de volume of the scar.
Vitamin E, onion extract or trolamine don’t have enough evidence, just like cryotherapy.
In the case of earlobe keloids, Dr Hibler combines surgery with the topical application of 5% imiquimod cream. This technique has good results, and the combination reduces the risk of relapse.
For acne and atrophic scars, retinoids had demonstrated improvement in the texture and appearance of the scars. He commented on a split face study comparing retinoids with microneedling with similar results (Figure 12).
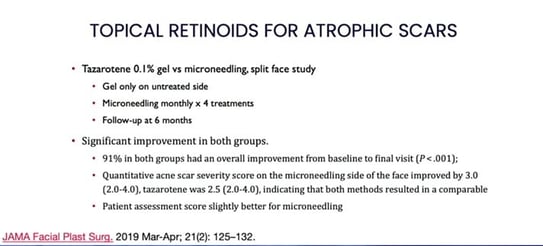
Figure 12. Comparison of retinoids and microneedling for the treatment of atrophic scars
Other useful tools are subcision, the use of chemical peels such as TCA or surgical techniques like punch elevation/excision.
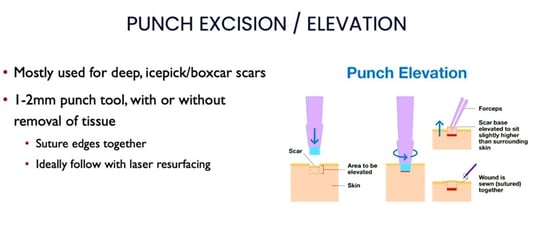
Figure 13. Protocol of punch excision/elevation for atrophic scars.
Conclusions:
Speaker: Dr Fatima Zahra Belgnaoui (Morocco)
In this talk Dr Zahra has stressed the importance of surgery in our field and also the importance of preparing the skin before surgery and performing proper disinfection to avoid infection as much as possible (it seems that chlorhexidine is better than povidone iodine for this). This will help to improve healing, reduce downtime and improve the cosmetic result.
It is also important to use low diameter sutures and surgical techniques to reduce wound tension and improve healing. Once the wound is formed, proper wound care, the use of silicone gels or early laser would improve the outcome.
Speaker: Dr Eugenio Gandolfi (Italy)
Dr Gandolfi described a new pocket-sized laser with dual wavelength 1927 nm/1550 nm. The combination of both improves the scars and its portable and easy to use.
It can be used as well for the treatment of stretch marks, non-ablative resurfacing and can be useful for the management of hyperpigmentation and melasma.
Speaker: Dr Brian Berman (USA)
Dr Berman divided his lecture in 3 sections.
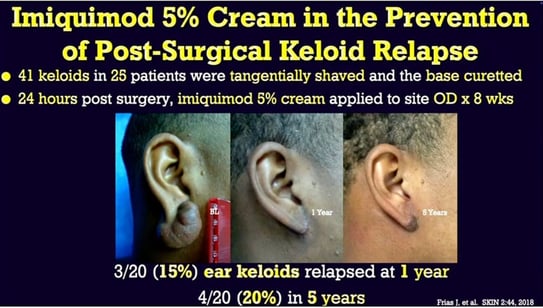
Figure 14. From Stashower ME. Successful treatment of earlobe keloids with imiquimod after tangential shave excision. Dermatol Surg. 2006;32(3):380-386. doi:10.1111/j.1524-4725.2006.32077.x
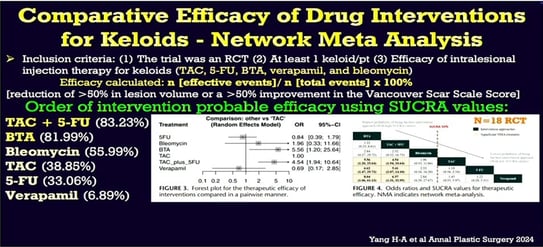
Figure 15. Yang et al. Annal Plastic Surgery 2024.
A single presurgical 1540 nm Erbium glass laser treatment, of a planned incision site is a simple, safe, and painless strategy to significantly improve the final scar appearance (Friedman et al. Laser pretreatment for the attenuation of planned surgical scars: A randomized self-controlled hemi-scar pilot study. J Plast Rec Aesth Surg 2020 ; 73 : 893-898)
Treatment with ablative lasers was more effective than non-ablative lasers, but with greater hyperpigmentation and time to heal
The Global Acne Scarring System score for concurrent isotretinoin and laser treatment was significantly lower than the side treated with isotretinoin and 6 months later laser (Taleb et al. Lasers Surg Med. 2023)
Speaker: Dr Michael H Tirgan (USA)
Dr. Tirgan is an oncologist specialised in the treatment of keloids. He does not recommend surgery as a first treatment of an early keloid. It can make it worse. Laser can be useful but there is insufficient evidence to support it (Leszczynski R et al. Laser therapy for treating hypertrophic and keloid scars. Cochrane Database of systematic reviews. 2022; 9.CD011642)
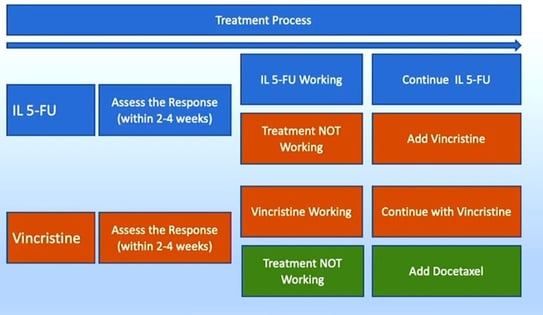
Figure 16. Protocol proposition for intralesional chemotherapy
Speaker: Dr Albert Wolkerstorfer (Netherlands)
The way drugs are injected into keloids is important to avoid skin atrophy. Sometimes this is challenging. Little is known about biodistribution (Yin Q et al. The biodistribution of triamcinolone acetonide injections in severe keloids: an exploratory three-dimensional fluorescent cryomicrotome study. Arch Dermatol Res 2024. 8; 316-368) and there are simple tricks to improve it, such as the use of thin needles and syringes and the concomitant use of contact cryotherapy.
Speaker: Dr Madiha Frikha Mseddi (Tunisia)
Dr Mseddi proposes the use of 40% phenol weekly application for the treatment of keloids. They have been using it since 2010 (Mseddi M et al. Treatment of keloid with phenol: a new therapy. Ann Dermatol Venereol. 2014; 141: 493-499)
Phenolisation is an innovative and promising treatment. Regression of more than 60% of the scar in 85% of cases. Nearly a quarter of the patients achieve the disappearance of the entire scar. It’s generally well tolerated and has a reassuring character.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speakers: Rox Anderson, Jean Carruthers, Sebastian Cotofana
Speaker: Professor Sebastian Cotofana (USA)
Prof. Cotofana’s talk was about the anatomy of the lips and how this area is one of the first we look at. He stressed the importance of the location of the facial artery (Cotofana S et al. Distribution pattern of the superior and inferior labial arteries: Impact for safe upper and lower lip augmentation procedures. Plast Reconstr Surg 2017. 139: 1075-1082, Cotofana S et al. Anatomy of the Superior and Inferior Labial Arteries Revised: An ultrasound investigation and implication for Lip Volumization. Aesth Surg J. 2020; 40: 1327-1335) and its implication in the injection technique (Ghannam S et al. Treating the lips and its anatomical correlate in respect to vascular compromise. Facial Plast Surg 2019; 35: 193-203).
Finally, he talked about a recent study that he published about lip compartments and their potential clinical relevance (Cotofana S. et al. Intralabial Lip Compartments and their potential clinical relevance. Plast Reconstr Surg. 2023). (Figure 17)
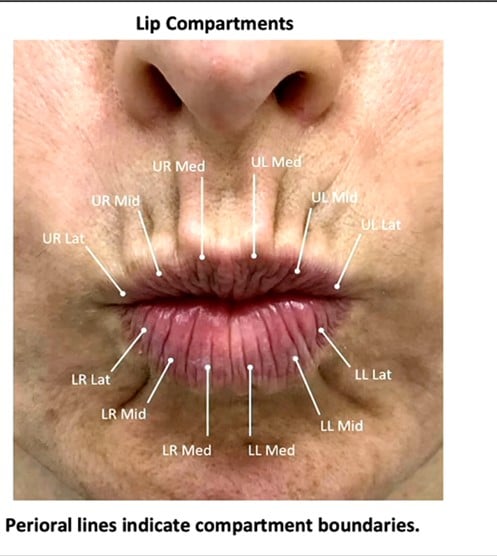
Figure 17. Perioarl lines help locate the various lip compartments
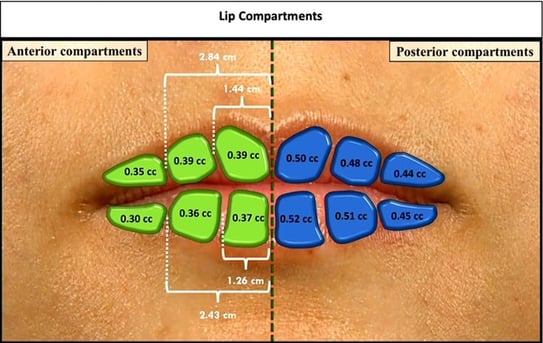
Figure 18. Lip compartments.
He proposes that injections be made in the lips compartment with needle vertical technique to avoid breaking the walls between compartments (Figure 18).
Speaker: Dr Jean Carruthers
In this presentation Dr Carruthers talks about how she and her husband, Dr Carruthers, described the use of botulinum toxin for cosmetic purposes in the treatment of expression wrinkles. At first, they were told that their idea would go nowhere, but in 2022 3,945,282 neuromodulator treatments were performed in the world.
Dr Carruthers proposes that botulinum toxin in combination with other treatments prolongs aesthetics results.
She proposes injecting platysma and oris angle depressor before EBD treatments in the lower third and neck to improve the result.
Speaker: Dr Richard Rox Anderson (USA)
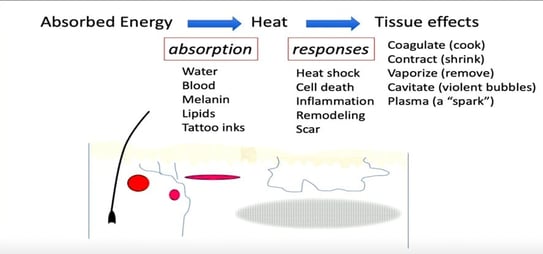
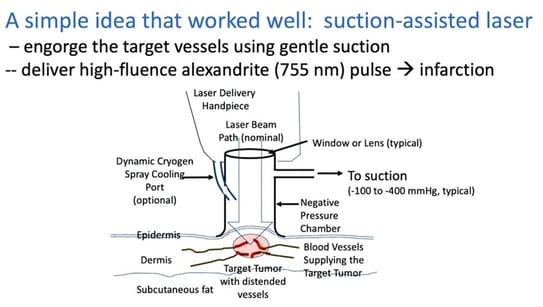
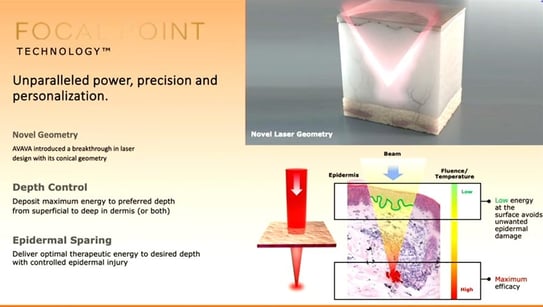
Figure 19. Summary of the main effects on the skin with energy-based devices.
In 1983 Dr Anderson published a groundbreaking paper: “Selective photothermolysis” and people thought he was crazy at first. It is the foundation of all EBDs available today.
What is new?
Speaker: Dr Meryem Ozlem Ozturk (Turkey)
They conducted and studied where they injected renal transplant patients and healthy controls. They use 0,5 ml Hyaluronic acid in the zygomatic arch. No complications were observed in either the renal transplant or the healthy group after 6 months follow up. The frequency of adverse effects was similar. HA injection procedures can be safely applied to these patient groups.
Speaker. Dr Armeela Javaid (Pakistan)
Bimatoprost 0,03% has FDA approbation for lash growth. It has been studied for efficacy and safety. It is a structural analogue of Prostaglandin F2. It is intended to be used topically not as an eye drop. It is a gradual growth with full results in 16 weeks.
Dr Javaid enrolled 45 patients that applied the solution daily for 120 days. 80% of patients had darker and longer lashes. Only 4 patients had slight eye dryness and irritation. The safety profile was good.
Speaker: Dr Maximiliano Maass (Chile)
Dr Maass proposed the use of intralesional steroids (0,1 ml triamcinolone acetonide on the lateral sides at the level of the proximal nail fold) after surgical avulsion to prevent recurrence and adverse events (nail dystrophy, growth abnormalities...) and they conducted a study when they compared total nail avulsion and total nail avulsion plus corticosteroid injection.
Preliminary results suggest that this combined approach may reduce the incidence of post-surgical nail dystrophy. The results must be confirmed in prospective randomized controlled trials with larger sample size.
Speaker: Dr Saud Aleissa (USA)
Jet injection works via active diffusion, forcing a stream of liquid through a precision nozzle. The high speed and pressure of the liquid enables it to penetrate in a web-like distribution. They conducted a study with 15 patients with Basal cell carcinoma and they used jet injection photodynamic therapy (4 PDT + excision and 11 2 sessions of PDT separated 4-6 weeks) with promising results.
Speaker: Dr Maxine Bennek (Germany)
They conducted a split face study. In one side of the face, they injected ona or abobotulinum toxin and in the other side letibotulinum and compared their diffusion capacity. They conclude that differences in the diffusion characteristics should be considered, especially when switching products. LetibotulinumtoxinA is a highly precise and targeted toxin with predictable diffusion.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Professor Pablo Boixeda (Spain)
The most important thing before treating these diseases is an accurate diagnosis. Prof. Boixeda proposes some principles treating skin manifestations in systemic diseases:
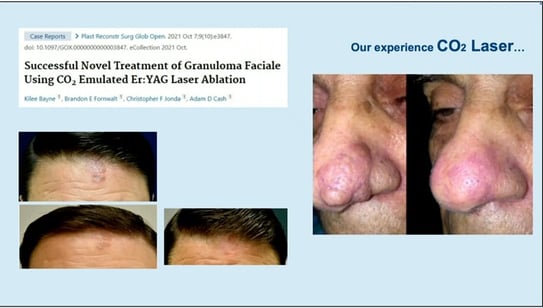
Granuloma faciale: It can be treated with picosecond, ablative lasers and even vascular lasers.
Necrobiosis lipoidica: Pulse dyed laser can be used but using wide spot and long pulses. The endpoint is erythema. It is recommended to use sub purpuric settings in order to avoid ulceration.
Sarcoidosis: Chronic facial lesions can be treated with PDL in combination with CO2

Hidradenitis suppurativa
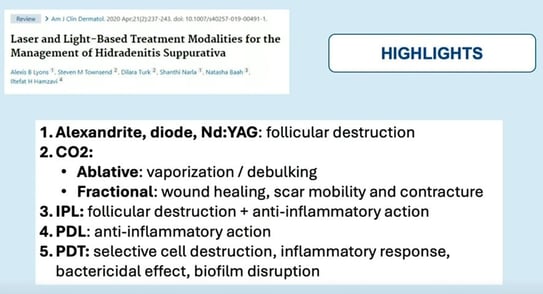
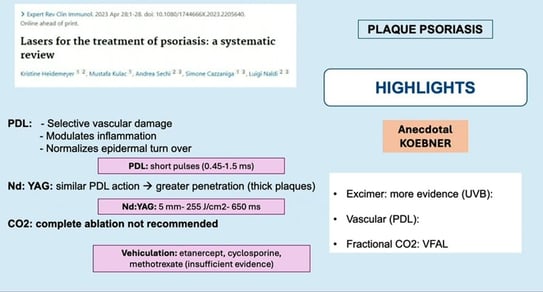
Psoriasis: Its 2nd line treatment but it can be useful for nail psoriasis.
Haley-Haley

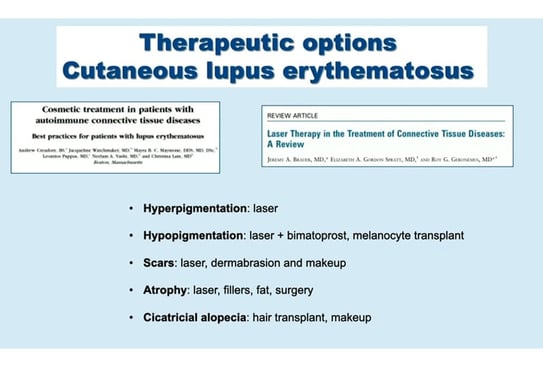
Lupus
Conclusions: Laser should be used with caution especially in higher phototypes.
Most evidence consists of case reports and a small case series. Larger studies are needed to determine the effectiveness of these treatments.
Speaker: Dr Claudio Marasca (Italy)
Pseudotumor is a term encompassing dermatological conditions which are not true proliferations, but either have a clinical resemblance to a known tumor.
Recurrent melanocytic nevus is defined as the proliferation of remaining melanocytes that occurs after the partial removal of a melanocytic nevus, which leads to repigmentation at the site of previous excision.
Exophytic lesions can be treated with ablative lasers while flat lesions can be treated with nano or picolasers. Recurrences can occur in 2% of patients, especially when we treat intradermal nevi.
The occurrence of recurrent nevi was inversely associated with increased patient age, darker phototypes and dermal nevus. The presence of dark brown colour, multiple colours, dots, terminal hair and an annular distributed pigmentation around adnexal structures. But how can we differentiate recurrent nevi of recurrent melanoma? By their characteristic dermoscopic patterns
Congenital nevi: More than 4 years of follow-up is required to evaluate the efficacy of lasers in CMN, and partial excision and laser combination treatment might be an effective treatment option.
Melanocytic nevi after laser hair removal. It can present some dermatoscopic changes such as pigmentary blotches with crust formation, pigmentary blotches with subsequent loss of pigment network, asymmetric pigment network with gray-blue dots and milky red veil, blue-gray areas, loss of pigment network and peppering morphology. The delay or error in diagnosis often occurs because the pathologist does not know that the lesion has undergone some local destructive treatment and, therefore, they diagnose melanoma instead of pseudomelanoma.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Monika Fida (Albania)
The red face is a broad of differential diagnosis and in most cases is a benign disease (rosacea, seborrheic dermatitis or photodermatosis), but we must not forget other causes such as drug reactions, carcinoid syndrome etc.
Differential diagnosis of the most common dermatosis is presented in the table below:
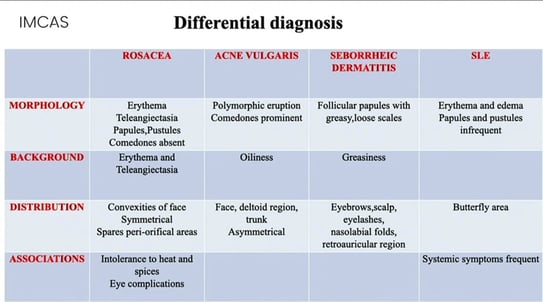
Dr Fida described the most common treatments and her approach for rosacea (antibiotics, topical with azelaic acid, antibiotics and gentle cleanser and lasers), seborrheic dermatitis (low topical corticosteroids, topical antifungal agents, topical calcineurin inhibitors and in resistant cases always test for HIV and oral itraconazole can be an effective treatment), atopic dermatitis (topical corticosteroids, immunosuppressors, antiinterleukin4/13, JAK inhibitors…), psoriasis and lupus.
Take home message
Managing facial erythema can be frustrating for both patients and dermatologist.
The key to success is to make a clear diagnosis and to aid the patient with treatment of compliance.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Yaryna Turkevych (Ukraine)
Dr Turkevych talked about collagen stimulators, and she divided them in two groups:
Conclusions:
There are no direct collagen stimulators that can cause physiological neocollagenogenesis. Using Calcium hydroxyapatite, Polylactic L-acid and energy-based devices it is necessary to combine Polynucleotides and exosomes for more natural and physiological results. We need to investigate and learn a lot in the area of preaging medicine.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Arnaud Lambert (France)
Dr Lambert talked about IPL being the most bought energy-based device in France. In his opinion, it is because of its rentability and versatility (you can target melanin and blood vessels).
In this talked he defends this device because it is affordable and accessible and very polyvalent. Combinations are always a good idea.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Alexandre Filippo (Brazil)
Toning mode with nano and picolaser promotes the decrease in the number of melanocytic dendrites, change in the structure and size of melanosomes and cavitation in the dermis.
Dr Filippo proposes his technique to treat PIH: he combines the toning mode (7 mm fluence 0,6-0,8 J with several slow slides) and fractional mode (6x6 fluence 1,5J) in order to improve the extracellular matrix.
He uses this approach for all the pigmentary disorders.
Conclusions
- Chronic pigment disorders stay challenging
- Patient expectation should be managed and reduced
- Consent form and photographic documentation are very important.
Reports written by Dr. Ana Reymundo (Dermatologist, Spain)
Speaker: Dr Paolo Bonan (Italy)
Microwave technology can be used to treat localized fat, cellulite and skin laxity. It can penetrate deep into the skin by treating fat more selectively and without damaging the epidermis (Bennardo L et al. Microwave Therapy for Cellulite: An effective non-invasive treatment. J Clin Med 2022. 11; 515; Nistico SP et al. A new treatment protocol to treat abdominal subcutaneous fat combining microwaves and flat magnetic stimulation. Bioengineering. 2022; 21:182; Zappia E. et al. An innovative microwave technology for the treatment of submental skin laxity. Lasers Med Sci 2025; 40:28). The heat generated also serves to induce collagen production and improve skin texture.
It can be combined with CO2 and 1540 nm non ablative diode, as well as with fillers (it increases the proliferation of pre adipocytes).
Speaker: Dr Anil Ganjoo (India)
The technique of resurfacing has evolved from conventional ablative to conventional non ablative to fractional ablative and non-ablative to microneedling radiofrequency to subablative RF and now to nano-subablative RF. This evolution happened due to the quest to develop a technique of resurfacing that would be devoid of side effects as far as possible while producing maximum results.
Speaker: Dr Anthony Rossi (USA)
Dr Rossi’s talk was about the possibility of combining different technologies such as botulinum toxin, fillers, and ablative lasers. He has shown different cases in which he performs all 3 procedures in one session. He starts with the toxin in the muscle plane, then topical anesthesia, fillers and finally lasers. As he works on different planes (muscular, subcutaneous, and dermal) there is no problem in performing all 3 procedures at the same time (Dempsey A et al. Practice patterns regarding combination treatments and laser and energy-based devices: A survey of American Society for Laser Medicine and Surgery Members. Lasers Surg Med 2023. 55:16-21).
Speaker: Dr Neeraj Pandey (Singapore)
Over the years with the evolution of technology, the laser has become a fundamental, irreplaceable omnipresent device of modern dermatology practice. At present, new devices have been under development for the therapy of different kinds of diseases.
The lasers, already in use, are evolving to be more effective and useful in many other disorders.
Some unconventional uses of lasers are:
Take home messages
Speaker: Dr Anjali Mahto (UK)
The multimodal approach in the treatment of acne scars is highly recommendable. It provides synergistic effects for superior outcomes (we can treat the textural irregularities, volumetric loss and pigmentation changes).
Dr Mahto’s protocol is to apply polynucleotide with gentle cannula subcision to improve hydration and elasticity 2 sessions 2 weeks apart. And she uses laser to do a resurfacing treatment. Afterwards, she applies topical exosomes to enhance healing and reduce downtime.
Polynucleotides stimulate fibroblast activity and collagen synthesis, enhance hydration and elasticity, and promote extracellular matrix remodelling. They act as a priming to the dermis.
Exosomes are extracellular vesicles rich in growth factors and cytokines that reduce inflammation and erythema and enhance collagen synthesis and dermal repair. Applied post laser, they can accelerate healing and improve scar texture, tone, and recovery times.
Therefore, combining these three technologies can lead to fewer sessions and improved patient outcomes.
Speaker: Dr Sang Ju Lee (Korea)
In this lecture, Dr Lee discussed the different therapeutic options that can be used for the treatment of stretch marks.
Microneedling, non ablative fractional laser, and ablative fractional laser are all effective for stretch marks. Among these three methods, ablative fractional CO2 laser was the most effective.
Applying 30µm sized PLLA after ablative fractional laser was more effective than laser alone.
Speaker: Dr Dianne Quibel (USA)
Dr Quibel talked about combining different lasers and energy-based devices depending on the layer of skin you want to treat. And that in some cases the combination with peelings, botulinum toxin, corticoids, vaporisation can be very useful.

Reports written by Dr. Lidiya Todorova (Dermatology, Bulgaria)
Speakers: Dr Muriel CREUSOT (Dermatologist, Belgium) and Dr Alessio REDAELLI (MD, Italy)
The session was a round table with a focus on skin boosters, where experts gave their scientifically backed opinion and recommendations. Skin boosters are more than just a beauty trend; they are scientifically backed treatments that enhance hydration, stimulate collagen, and improve skin texture. Whether used alone or in combination with other aesthetic procedures, they offer significant benefits without the risk of fibrosis. As research continues, their role in dermatology and regenerative medicine is expected to expand even further.
The session was a round table that included representatives of skin booster brand producers, including Dr Alessio REDAELLI, who introduced the topic, Dr Aude BERNARDIN (Allergan Aesthetics), Dr Natalia SUKMANSKAYA (Fillmed), Xiaoming LIN (Galderma), Dr Mimi Rosealie BORRELLI (Merz Aesthetics), Dr Silvia INNOCENTI (Relife), Dr Jimmy FAIVRE (Teoxane).
After a brief introduction of each one of them, Dr. Redaelli initiated the discussion with a short overview over each presented product (details within the following table):
| Company | Brand Name | Indications | Active Ingredients |
|---|---|---|---|
| Allergan Aesthetics, an AbbVie Company | Juvéderm® VOLITE™ | Fine lines and skin texture | Cross-linked hyaluronic acid (HA), 12mg/ml, with lidocaine (0.3% w/w) |
| Laboratoires FILLMED | NCTF® 135 HA | Intense revitalization and hydration of tired or dull skin, filling of superficial wrinkles, and skin redensification | 60 essential active ingredients chosen for their role in skin metabolism at precise dosage |
| Galderma Laboratories, L.P. Fort Worth | Restylane® Skinboosters™ Vital, Vital Lidocaine, Vital Light Lidocaine | Face and non-facial indications for Restylane® Skinboosters™ | HA manufactured using NASHA (Non-Animal Stabilized Hyaluronic Acid) technology |
| Merz Aesthetics | Belotero Revive® (HA20G; CPM-HA; Belotero Revive®) | Overall skin quality improvement and skin revitalization, hydration, elasticity, and firmness. Smoothing fine and superficial facial lines | Glycerol with a cohesive poly-densified matrix of hyaluronic acid (HA) at a concentration of 20G |
| Teoxanne | RHA®1 | Correction of the superficial of the fine wrinkles of the face and skin quality | 15 mg/g high molecular weight HA (4 MDa) |
| Relife | Definisse™ hydrobooster | Aging, to maintain hydration, to improve tone and elasticity, smile lines | Non-animal sodium hyaluronate with high molecular weight (> 3 million Da), obtained from Streptococcus equl |
The Round table began with a zealous discussion, followed by questions asked online and on-site in the conference room. The initial questions posed were whether skin boosters are myth or reality, how do they work, and how do they truly deliver on their claims? Indeed, for some time, skin boosters have become a key player in aesthetic dermatology, promising improved skin texture, hydration, and collagen stimulation. All the brands’ representatives confirmed not only that these injectables enhance skin texture and hydration by boosting aquaporin 3, but there is also an increased skin elasticity and fibroblast activity that stimulates collagen production and extracellular matrix (ECM). The hydrating qualities of skin boosters can be also explained with the natural ability of hyaluronic acid to attract water. New clinical trials confirm the new collagen formation, while ultrasound examination proves the improved skin texture, hydration, and increased skin thickness. Moreover, skin boosters also improve dermal regulation, skin sensation, and barrier function, and can accelerate wound healing processes. In fact, ex vivo and in vitro studies show that fibroblast migrate towards the hyaluronic acid gels within two weeks and therefore they are able to form new tissue.
The next question concerned collagen stimulation. The ability of skin boosters to stimulate collagen production is a crucial factor in their effectiveness for skin rejuvenation. The brands have explored how their formulations influence collagen synthesis and skin quality, yielding promising results. Skin boosters stimulate the production of pro-collagen, collagen types 1 and 3, and this is without inducing fibrotic tissue. Studies have shown slight inflammation upon injection in animal models and ex vivo conditions. However, there is no significant fibrotic scar tissue surrounding the gel, allowing for natural collagen formation. It was also mentioned that skin boosters stimulate collagen production by occupying space within the dermis. When injected, the first response involves collagen 3 production (associated with wound healing), followed by collagen 1 synthesis.
In terms of volumization, the experts agreed that while primarily acting as biostimulators, skin boosters also exert mechanical action by stretching and volumizing skin defects and can deliver plumping effect through water retention and of course collagen stimulation, which enhances skin density and leads to more tissue formation within the same space.
A discussion followed on the mechanism of action. Skin boosters operate through mechanical transduction signals, increasing water content within the skin. This modification in hydration alters the mechanical properties of fibroblasts, leading to enhanced collagen synthesis.
How about combination treatments? Many of the experts on the round table recommend combining skin boosters with hyaluronic acid fillers for comprehensive aesthetic results. Skin boosters can be applied to the superficial layers of the skin to improve its sheen and luster, while fillers add volume. These treatments can be performed in a single session for optimal effects. Combining skin boosters with NCTF for reduced complications and side effects is also a good option. The combination with lasers has also been suggested, where laser treatments are performed before skin booster injections to prime the skin. Combined treatments enhance overall outcomes and should be specified individually.
Do skin boosters have any effect on the subcutaneous tissue? They do not directly stimulate adipocytes. However, hyaluronic acid stimulates fibroblasts within the fat tissue, which then contributes to skin regeneration and repair.
A very modern and timely question regarding the use of skin boosters in patients undergoing treatment with semaglutide was posed, but it still remains an area of ongoing research. As the anti-diabetic drug is a relatively new medication, no definitive guidelines exist for integrating skin boosters into the treatment regimen. Current advice suggests individual patient assessment to determine the appropriate timing and approach.
In all, the session delivered unmatched information on how skin boosters work, and why they play a vital role in aesthetic medicine by stimulating collagen production, enhancing hydration, and improving skin elasticity. They can be effectively combined with HA fillers, laser treatments, and other regenerative therapies for comprehensive skin rejuvenation. With ongoing research and emerging clinical applications, skin boosters continue to prove their efficacy in enhancing skin quality and overall aesthetic outcomes.
Reports written by Dr. Lidiya Todorova (Dermatology, Bulgaria)
Speaker: Dr Monika Fida (Albania)
Dr. Monika Fida, an esteemed dermatologist from Albania, gave a highly scientific talk on the very contemporary topic on exosomes. She explained that in nature exosomes are a subpopulation of extracellular vesicles (EV), nanosized particles, lipid-bilayer enclosed, naturally secreted from cells after the fusion of intracellular multivesicular bodies with the plasma membrane. The experiments in which EVs were specifically identified as “biological entities carrying enzymatic and functional potential” began in the 80s and the term was coined in this period.
Compared to traditional dermatological therapy, the cell-free exosome therapy offers several advantages: targeted delivery, low toxicity, tissue repair, personalized treatment and multifunctionality, including:
These advantages make exosome-based therapy a promising new and relatively safe method for individual treatment approach to variety of skin conditions [1], [2].
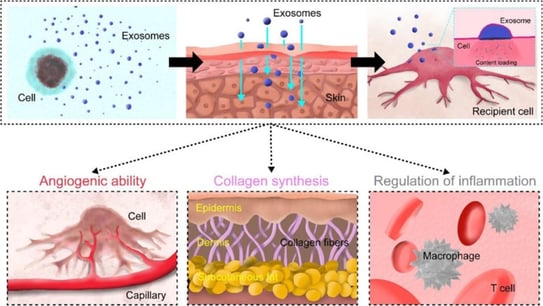
Figure 20. “Schematic representation showing skin regenerative abilities of exosomes” [3]
Currently, exosomes are clinically effective in wound healing and scars, as well as their application as an anti-age treatment, but research on inflammatory and autoimmune skin conditions is still in the preclinical stage.
Studies done confirm their effectiveness in improving skin wrinkles, elasticity, hydration and pigmentation. It is also proven that they potentiate other treatments like fractional CO2 lasers in the treatment of acne scarring.
How exosomes work in different conditions:
Indisputably, exosomes are future in regenerative medicine. But what are the current challenges that surround these treatments?
In conclusion, Dr. Fida highlighted that exosomes promise a future of tissue regeneration, skin rejuvenation and targeted therapies, but further investigations are needed to optimize their efficacy for clinical use.
Articles used by Dr. Fida in her presentation:
Speaker: Dr Atchima Suwanchinda (Thailand)
Lecture summary: Exosomes from young versus old donors: what are their regenerative capacity and clinical implications? Exosomes derived from adipose mesenchymal stem cells (AMSCs) have been explored to determine how donor age affects their molecular profiles. Current research, presented by Dr. Suwanchinda, Vice President of the International Society for Dermatologic Surgery and the Association for Dermatologic Surgery in Thailand, reveals key differences between young and old donor exosomes. Younger exosomes show greater regenerative potential due to higher levels of cytokines and growth factors, while older exosomes still maintain functionality but exhibit a decline in regenerative capacity. These findings may play a key role in the future application of exosomes in terms of personalization and therapeutic indication.
What are the differences between exosomes derived from young and old donors? Do these differences impact their regenerative capacity? These questions have been addressed through recent research presented by Dr. Suwanchinda. Her study explores the quality of AMSCs-derived exosomes in relation to donor age, shedding light on their functional characteristics and potential clinical applications.
The key findings on their structural and functional differences are the following:
The cytokine profile analysis of the explored groups revealed:
When the scientific group led by Dr. Suwanchinda compared the regenerative potential of young- and old-donor exosomes, they found the following interesting observations:
Senescence and aging markers were estimated through the measurement of cytokines such as IL-6, IL-10, and IL-18. They showed no age-dependent differences, therefore their exosomal anti- and pro-inflammatory activity may be maintained across lifetime. When measuring Jagged1 (major NOTCH signalling ligand), responsible for tissue regeneration, wound healing and angiogenesis, the scientists established that it has decreased with age. Therefore, this suggests reducing regenerative potential with aging.
What are the key clinical applications of these findings:
Conclusions:
The final thoughts of Dr. Suwanchinda highlighted that exosome therapy presents exciting possibilities for regenerative medicine, aging, and inflammation control. While younger exosomes display superior regenerative potential, older exosomes still hold significant therapeutic value. Understanding and optimizing exosome compositions will be key to unlocking their full clinical potential.
Reports written by Dr. Lidiya Todorova (Dermatology, Bulgaria)
Chairs: Jeremy Magalon (Pharmacologist, France); Dr Sophie Menkes (MD, Switzerland) ; Dr Hernan Pinto (PhD – Research, Spain)
Speaker: Dr Shadi Kourosh (Dermatology, USA)
Dr. Shadi Kourosh, a renowned U.S. dermatologist, delivered the opening lecture at “PRP innovations” session, providing an overview of platelet-rich plasma (PRP) and the secretome in hair restoration and skin rejuvenation. She analysed recent data, highlighting both advancements and controversies in the protocols used in regenerative aesthetics. Her presentation concluded with expert guidance at future research with the goal of fostering innovation in patient care.
For her lecture, Dr. Kourosh acknowledged the guidance of Prof. Maria Hordinski, dermatologist, recognized for her expertise and research in hair diseases and the peripheral nervous system as it relates to hair follicle biology, and introduced a structured approach to regenerative aesthetics through the "7 S" framework:
She emphasized the regenerative potential of blood, particularly its ability to transmit youthful signals while reducing senescence-associated secretory phenotypes (SASP). Parabiosis, or the shared circulation of two organisms, was discussed as an emerging concept in enhancing regenerative capacity. The goals are to transmit youthful signals to tissue, to decrease senescent signals (SASP) and to increase the regenerative capacity of the organism. The blood includes everything necessary: growth factors (GFs), mRNA, platelets, secretome, exosomes. PRP, a widely used method, remains inconsistent due to variations in its composition, preparation, and application protocols, which are influenced by factors such as:
Dr. Kourosh outlined key challenges in PRP use, including the frequency of treatment, patient selection criteria, stability of growth factors, mode of delivery, and efficacy in non-androgenetic alopecia. She emphasized the need for standardization in PRP preparation and dosing to ensure optimal regenerative outcomes. Current approaches recommend an induction phase of three treatments at monthly intervals, followed by maintenance phase of one treatment every 3-6 months.
Combination therapies are emerging as an effective strategy. PRP combined with hyaluronic acid stabilizes growth factors, enhancing rejuvenation. Additionally, PRP used alongside fractional lasers (1550nm and 1927nm) stimulates follicular stem cells and growth factors and achieve remarkable results in treating androgenetic alopecia and telogen effluvium. Low-level laser therapy (photobiomodulation) presents a low-risk, at-home option for hair restoration, but when combined with PRP the results are remarkable.
Key questions and challenges for the future of regenerative medicine include:
Dr. Kourosh's lecture highlighted the immense potential of PRP in regenerative medicine while emphasizing the pressing need for standardization and optimization. As the field evolves, refining protocols and integrating complementary treatments will be key to achieving consistent, effective results. The future of PRP is to be tailored to individual patient needs, ensuring its role as a main regenerative capacity inductor.
Speaker: Patrick Yam (Dermatology, Canada)
Dr. Patrick Yam is a recognized expert in the field of platelet-rich plasma (PRP) preparation and use. As a featured speaker at IMCAS 2025, he delivered a lecture on how platelet concentration in PRP affects clinical efficacy and how to improve PRP quality using simple visual cues and centrifuge adjustments. The audience gained practical tips for enhancing PRP concentration and clinical results, with optional insights into when and how hematology analysis might be beneficial.
Dr. Yam, the second lecturer in the "PRP Innovations" session, began his lecture by sharing his daily use of a hematology analyzer for a variety of aesthetic and medical PRP treatments. He then referenced Marx's (1998) classic definition of PRP as a high concentration of platelets in plasma, where platelet levels exceed 1 million per microliter, reaching concentrations 4-5 times greater than baseline. The preparation of PRP involves collecting blood in tubes, separating the plasma from red blood cells via centrifugation, and immediately collecting PRP. An optional second spin can be performed for even higher concentration.
However, not all PRP is the same. Dr. Yam cited an article by Prof. Magalon [1], who analyzed 36 PRP systems and found a vast range in platelet dose, from 0.6 to 12.8 billion (a 21-fold difference). The concentration varied from 79 to 2310x10^3 (a 29-fold difference). Less than half of the systems produced high-concentration PRP, and some even yielded platelet-poor plasma, with levels lower than baseline. Only one system consistently produced high-quality, high-concentration PRP. Intrigued by these findings, Dr. Yam conducted his own laboratory analysis, which revealed over 300-fold differences in platelet concentration between the lowest and highest PRP samples tested. Concentrations ranged from as low as 5k/µL (99% below baseline, essentially acellular plasma) to over 4 million/µL (more than an 800-fold difference). His research also identified variations in composition, including red blood cell (RBC) and leukocyte contamination. While lower RBC and leukocyte contamination improved PRP quality, it should not come at the cost of platelet concentration.
PRP quality is crucial, yet estimating growth factors (GFs) is complex and time-consuming. Instead, platelet count serves as a reliable proxy, as it directly correlates with GF levels. Additionally, some visual indicators can assess PRP quality without requiring a hematology analyzer.
How are platelets calculated? Dr. Yam provided a simple formula:
Dose = Concentration x Volume
For example: 1mL x 1 million/µL = 1 billion platelets.
He also presented a table demonstrating that a small tube of blood does not contain enough platelets for most treatments, highlighting that his team typically draws 50 mL per treatment.
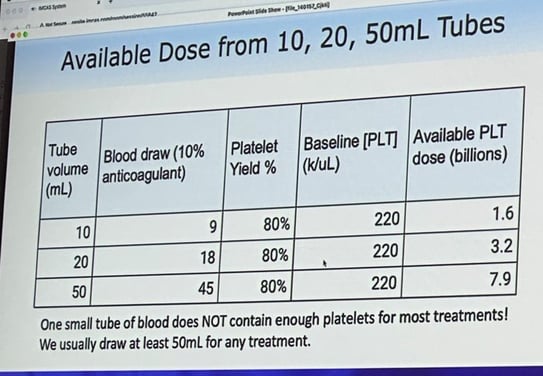
This leads to a critical conclusion: if platelet concentration is lower than baseline, the sample is actually platelet-poor plasma, or "bad PRP." The characteristics of "bad PRP" include:
After analyzing more than 11,000 samples, Dr. Yam’s research team found that "bad PRP" was very common. While hematology analysis remains the gold standard for detecting poor-quality PRP, there is a practical visual test: transparent PRP is always very low concentration. Another simple test involves checking for a visible platelet pellet and the presence of RBCs. PRP prepared in tubes with gels often suffers from overspinning, which traps platelets in the gel, leading to lower concentrations and poor yield.
Dr. Yam then posed the question: What settings should be recommended?
The optimal centrifugation settings depend on factors such as baseline platelet concentration, hematocrit, viscosity, tube size, and temperature. A suggested starting point is 6 minutes at 600g for small tubes.
To maximize PRP’s potential, practitioners should:
In conclusion, Dr. Yam’s findings emphasize the importance of platelet concentration in PRP efficacy. His research shows that poor-quality PRP is prevalent, but with proper techniques, its effectiveness can be significantly improved. By understanding platelet dosage, using correct centrifuge settings, and avoiding common pitfalls such as overspinning and low-yield tubes, clinicians can optimize PRP treatments for better patient outcomes.
[1] Magalon J et al. Technical and biological review of authorized medical devices for platelets-rich plasma preparation in the field of regenerative medicine. Platelets. 2021 Feb 17;32(2):200-208. doi: 10.1080/09537104.2020.1832653.
Reports written by Dr. Lidiya Todorova (Dermatology, Bulgaria)
Speakers : Prof Andrew F Alexis (Dermatologist, USA); Dr Seemal R Desai (Dermatologist, USA); Dr Albert Wolkerstorfer (Dermatologist, Netherlands)
Speaker: Dr Nicolas BACHOT (France)
Dr. Nicolas Bachot, a renowned French dermatologist specializing in hyperpigmentation and skin aging, delivered an insightful lecture on the management of periorbital hyperpigmentation (POH) using tranexamic acid. He disclosed data about a current clinical study that gives hope in the treatment in this challenging condition.
Periorbital hyperpigmentation (POH) is a widespread concern, with limited scientifically proven treatments offering long-lasting results. POH disproportionately affects melanin-rich skin compared to Caucasian skin and has an estimated prevalence of up to 30% among Indian individuals. Due to its multifactorial etiology and the presence of melanin in both the dermis and epidermis, POH remains challenging to treat. Despite the high demand for effective therapies, few scientifically validated solutions exist.
In the search for resolution, Dr. Bachot was inspired to start conducting a multi-center clinical study to evaluate the safety and efficacy of microneedling (MN) combined with tranexamic acid (TXA) and niacinamide for POH treatment. The audience at the session was the first to hear the preliminary findings.
The Phase 1 trial took place in Japan and Malaysia, involving 46 patients. The study protocol consisted of three MN sessions, each conducted one month apart, followed by a home treatment regimen between and after MN sessions. MN was performed at a depth of 0.5–0.7 mm, and the solution used during the procedure was niacinamide 10% and TXA 5%, both known for their anti-inflammatory and depigmenting properties. The at-home treatment during the first month included a light depigmenting peel (consisting of lactic acid 8.5%, TXA 5%, ferulic acid 2%). From the second to the fifth month, patients were asked to apply a depigmenting concentrate (niacinamide 10% and TXA 5%). The final assessment occurred in the fifth month.
Evaluation methods included:
Dr. Bachot presented preliminary results after only two MN sessions, revealing a significant reduction in POH levels. A 43.3% improvement was recorded compared to the control group, with 65% of patients showing good to excellent improvement. Treatment efficacy increased after the second MN session. Notably, no patients developed post-inflammatory hyperpigmentation, and only one patient experienced high erythema, while two reported slight redness and tightness, which were resolved within weeks. Despite the MN sessions, erythema levels decreased by 20.3%, indicating reduced inflammation under the eye. Overall, 47% of patients exhibited clear to mild erythema after the second MN session, demonstrating an improving trend with ongoing treatment.
The study concluded that:
The continuation of at-home treatment is crucial for confirming the therapy's long-term efficacy across varying POH severity levels. Further research will determine the necessity of ongoing at-home treatment and its role in optimizing results over time.
Reports written by Dr. Lidiya Todorova (Dermatology, Bulgaria)
Speakers: Dr Yolanda Gilaberte Calzada (Dermatologist, Spain); Prof Andy Goren (Dermatologist, Czech Republic); Dr Sergio Vano Galvan (Dermatologist, Spain)
Speaker: Dr Marisa MATHIEU (Dermatology, Belgium)
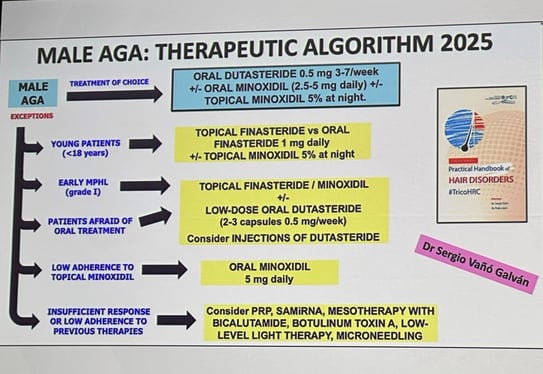
Dr. Marisa Mathieu, a Belgian dermatologist specializing in hair and nail disorders, delivered an insightful lecture on the latest treatments for androgenetic alopecia (AGA). The presentation featured numerous before-and-after images. Dr. Mathieu covered systemic antiandrogens such as bicalutamide and dutasteride, mesotherapy applications, botulinum toxin, and innovative experimental treatments.
Dr. Mathieu introduced oral bicalutamide, a nonsteroidal antiandrogen that blocks androgen receptors. This drug, an analogue of flutamide, offers an improved safety profile and has been shown to enhance hair density, reduce seborrhea, and improve acne and hirsutism. The recommended daily dosage ranges from 10 to 50 mg, though no consensus has been established. Clinical studies confirm its effectiveness in treating female AGA. Adverse effects such as mild increases in transaminases, peripheral oedema, gastrointestinal discomfort, mastalgia, asthenia, myalgia, and reduced libido have been reported. Specialists advise monitoring liver enzymes before treatment, one month after initiation, and then every three to six months. While the risk of severe hepatotoxicity is low, it typically occurs within the first months of therapy. Patients planning pregnancy should discontinue the drug two months prior due to the risk of fetal feminization [1-3].
Another systemic antiandrogen discussed was oral dutasteride, a 5-alpha reductase inhibitor with a long half-life of five weeks. Dutasteride blocks both type 1 and type 2 isoforms of the enzyme responsible for converting testosterone into dihydrotestosterone (DHT), thereby reducing the impact of androgens on hair follicles. The recommended dosage is 0.5 mg per day, with specialists suggesting a reduction to 0.5 mg two to three times per week after 12 to 18 months to improve patient compliance. The maximum treatment effect is typically observed within this timeframe. Biological monitoring is not required, except for prostate-specific antigen (PSA) levels. Dutasteride is not recommended for individuals using hepatotoxic medications, patients under 40 years old with a family history of prostate cancer, African American patients, or those over 50. The ideal candidate is an 18-year-old male with AGA. Dr. Mathieu also recommended combining oral dutasteride with oral or topical minoxidil for optimal results [4-5].
Mesotherapy with dutasteride has shown to be effective and safe in clinical practice when administered at 0.025% every three months [6]. Even better outcomes are observed when injectable dutasteride at 0.01% is combined with oral minoxidil [7]. Due to its long half-life, mesotherapy is recommended quarterly. Potential side effects include local erythema, pain, pruritus, headaches, oedema, hematoma, and folliculitis, though these are transient and typically resolve within 24 hours. Unlike oral dutasteride, mesotherapy is suitable for both men and women, making it an option for patients who decline oral treatments or experience side effects. Combining mesotherapy with oral or topical minoxidil, oral antiandrogens, or platelet-rich plasma enhances its effectiveness.
Mesotherapy with bicalutamide (0.5%) is an emerging option for treating AGA. It is recommended for female pattern hair loss patients and can be used alone or alongside other treatments. Although initial studies show only subtle improvements, the treatment's side effects are similar to those of dutasteride injections [8-9].
The use of botulinum toxin type A for AGA has garnered attention recently. Since alopecic areas suffer from microvascular insufficiency and reduced oxygen levels, this environment encourages testosterone conversion to DHT, which in turn triggers the production of transforming growth factor-beta1, a proapoptotic substance initiating AGA [10]. Although recent studies indicate that botulinum toxin has no significant effect on male AGA, further research continues [11].
Several promising topical antiandrogens are currently being developed, including GT20029 and pyrilutamide. GT20029 degrades androgen receptors by recruiting them for degradation, while pyrilutamide inhibits the binding of androgens to androgen receptors in hair follicles and sebaceous glands. Small interfering RNA (siRNA) technology is also being explored as a means of silencing specific genes by degrading their messenger RNA (mRNA). In AGA, siRNA inhibits androgen receptor mRNA, reducing its expression and blocking androgen signaling. Another related development, SAMiRNA, targets androgen receptors using self-assembled micelle inhibitory RNA, preventing protein synthesis and decreasing androgen receptor presence in dermal papilla cells [12].
CosmeRNA, a cosmetic product with EU certification, is designed to be applied biweekly to inhibit androgen receptor synthesis via inhibitory RNA. Exosome therapy, which utilizes extracellular vesicles containing proteins, lipids, mRNA, and miRNA, is also emerging as a potential treatment. Exosomes promote hair follicle regeneration, enhance cell proliferation, and facilitate angiogenesis. They also possess anti-inflammatory properties, counteracting follicular miniaturization, and deliver key growth factors such as VEGF, IGF-1, and FGF, which support follicular health.
Dr. Mathieu concluded her lecture with an overview of the anticipated treatment algorithm for male AGA in 2025, reflecting the advancements in the field and the promising future of combination therapies for optimal hair restoration:
Articles used in the presentation of the lecturer:



Bioderma Congress Reports IMCAS 2024