2 professionals
CILAD 2024 Bioderma Congress Reports
CILAD 2024 Bioderma Congress Reports
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Dr. Maria Alejandra Piegari Feliu (dermatologist, Argentina) and Dr. Ricardo Limongi Fernandes (dermatologist, Brazil)
Related topics
Coordinators: Dr Maria de Fatima Agüero De Zaputovich, Dr Angélica María Domínguez Duarte
Speakers: Dr Maria de Fatima Agüero De Zaputovich, Dr Denise Steiner, Dr Javier Ruiz Ávila, Dr Angélica María Domínguez Duarte, Dr Natalia Jiménez, Dr Ingrid López Gehrke.
Speaker: Dr Denise Steiner
Dr Steiner highlighted the importance of the periocular region as one of the main focuses of facial ageing due to its specific characteristics, such as thin skin, dilated vessels, accentuated pigmentation, sagging and expression lines. Furthermore, the presence of fat bags and dark circles under the eyes make this area even more challenging for reversing ageing.
It is applied to deep layers with cannulas to avoid only reaching the surface and to ensure a natural appearance. Slow movements and small amounts are essential to avoid irregularities.
Bioregenerator: PDRN (polydeoxyribonucleotide from salmon sperm)
Result: deep renewal of the periocular skin, with a more even texture and reduction of marked wrinkles
The combined techniques presented by Dr Steiner are highly effective in the periocular region, providing visible and long-lasting rejuvenation.
The holistic approach, with combinations of personalised techniques, reflects an evolution in aesthetic treatment, prioritising natural and safe patient results.
Speaker: Dr Javier Ruiz Ávila
The presentation highlighted the latest innovations in aesthetic treatments to address visible signs of ageing in the perioral area, as well as the importance of combining techniques and technologies to provide comprehensive results.
4 units on the upper and lower lip, distributed in multiple points.
It is indicated for treating sun spots, vascular lesions and improving overall skin tone.
Used to apply exosomes, peptides and other regenerative molecules into deep layers of the skin
Conclusion: The presentation provided a holistic perspective on managing ageing in the perioral area, highlighting the importance of personalising treatments and using innovative techniques. The combination of biostimulators, peptides, botulinum toxin, and laser and IPL technologies guarantees satisfactory and natural patient results, promoting patient well-being and confidence.
Speaker: Dr Angélica María Domínguez Duarte
The conference addressed ageing in the neck and jawline, which are key areas for comprehensive facial rejuvenation. She emphasised that, although the face may be well cared for, a neglected neck can give away age. This process involves sagging, loss of bone support, fat accumulation and skin deterioration, factors that require a personalised, multidimensional approach.
1. Collagen stimulators
2. Lipolysis and tightening technology
3. Lipolytic enzymes
4. Botulinum toxin
5. Dermal fillers
6. Eliminate skin lesions associated with the ageing process
With this holistic approach, patients can be provided with visible and satisfying results, improving their appearance and their confidence.
Speaker: Dr Natalia Jiménez Gómez
The presentation highlighted the exponential growth of non-surgical rejuvenation procedures worldwide, according to recent ISAPS data. From 2019 to 2023, a 40% increase in treatments such as botulinum toxin, dermal fillers and tighteners has been found. However, this attention to the face has created a stark contrast to other areas of the body, such as the neckline, which tend to be neglected despite significant sun exposure.
The main objective is to holistically address the different needs of the neckline, from blemishes to sagging. This approach combines treatments for:
Focused energies:
Images of real cases were presented showing:
This presentation highlighted the crucial role of dermatologists in assessing and treating neglected areas such as the neckline, highlighting current innovations in non-invasive techniques and focused energies.
Speaker: Dr Ingrid López Gehrke
This presentation highlighted the importance of holistic aesthetic treatments, not limited to the face, but also in often neglected areas such as the neck, neckline and especially the hands. The dermatologist’s mission to inform patients about their overall skin care, including areas that are less visible but equally vulnerable to ageing and sun damage, was highlighted.
Visual results
Final considerations
The presentation underlined the relevance of a holistic approach to aesthetic treatments, prioritising safety and customisation according to individual needs. The combination of innovative techniques and products was promoted as the key to achieving effective, natural results. In addition, the importance of including hand care in rejuvenation plans was emphasised. The hands are an area that, although often overlooked, are essential for a harmonious and rejuvenated appearance.
Coordinators: Dr Elda Giansante, Dr Denise Steiner
Speakers: Dr Gabriela Lydia Ortega Gutierrez, Dr Elda Giansante, Dr Denise Steiner, Dr Felipe Ribeiro da Silva.
Speaker: Dr Gabriela Lydia Ortega Gutierrez
Dr Gabriela Lydia Ortega Gutiérrez stressed that her objective was to help attendees better understand how to perform chemical peels effectively and avoid complications.
Main points of the presentation:
Dr Ortega Gutiérrez explained that there are more than 100 types of chemical peels, of which professionals should master at least 10. She mentioned the classification according to:
Dr Ortega highlighted several key points:
Case 1: Moderate acne with perioral dermatitis:
Case 2: Severe acne with scarring:
Case 3: Patient with mutilated acne:
Case 4: Patient with severe acne and serious psychological history:
Case 5: Superficial peel with intense desquamation:
Conclusion: Dr Gabriela Lydia Ortega Gutiérrez emphasised that chemical peels are safe and effective tools as long as they are performed with knowledge, preparation and appropriate protocols. Their use not only improves the skin, but can also transform lives by restoring patients’ confidence.
Speaker: Dr Elda Giansante
Melasma is a chronic, recurrent and manageable dermatological condition that significantly affects patients’ quality of life. Its treatment is a therapeutic challenge due to factors such as previous treatments, duration and the therapeutic method applied (monotherapy or combination therapy).
Treatment objectives: Reduce the intensity of pigmentation, reduce the extent of affected areas, prevent recurrences and improve the patient’s quality of life. Therapeutic proposal
Melasma treatment is divided into four main lines:
Chemical peels as a therapeutic tool:
Chemical peels consist of applying caustic agents to yield controlled exfoliation of the skin, classified according to the depth reached: very superficial or superficial (epidermis), medium (papillary dermis) or deep (reticular dermis).
Factors to consider in peels:
Common exfoliating agents in melasma:
Application protocol
Initial assessment: medical history, photograph and informed consent
Prior preparation (2–4 weeks): use of topical depigmentation agents such as hydroquinone or glycolic acid
The Jessner peel is one of the most widely used, very practical and safe peels. Higher number of passes, greater depth (4–6), frosting occurs, burning lasts 5–6 minutes, relief with cold air. Increases TCA penetration. Precautions: Not for large areas due to allergy or toxicity to resorcinol and salicylic acid, instability with exposure to light.
Another peel for melasma is retinoic acid (tretinoin), at a concentration of 1–10% in propylene glycol or make-up base. It acts at the cellular level, stimulating collagen synthesis. It stays on for 4–12 hours, produces xerosis and erythema. Exfoliation occurs from the second day onwards. It persists for 2 to 5 days.
The 15–30% salicylic acid peel is very safe in patients with skin type I–VI. As a lipophilic beta-hydroxy acid, it collects in the pilosebaceous unit, and is excellent for acne patients. The crystallisation of the acid on the skin simulates frosting. After application, the skin remains whitish until the acid is removed after 30 to 120 minutes.
The 30–50% mandelic acid peel is also used for melasma. It is an alpha hydroxy acid derived from the hydrolysis of bitter almond extract, and is less irritating than glycolic acid. Gentle application with brush or swab. After 5–15 minutes, erythema, mild pruritus and burning. Remove with water.
The glycolic acid peel is highly erythematous and results in a non-uniform response to application and can lead to necrotic ulcerations. It is not one of the preferred ones, according to this doctor. Neutralisation is mandatory. Pyruvic acid also requires neutralisation. It is an alpha-keto acid, which is also not a favourite, but it gives very good results in ageing. It works very well on stretch marks.
The 10–50% trichloroacetic acid (TCA) peel is stable and inexpensive; no neutralisation is required. The depth corresponds to frosting intensity. It can be used for superficial, medium and deep peels. Avoid on IV–VI skin due to the risk of post-exfoliation hyperpigmentation.
Clinical outcomes: noticeable improvements in pigmentation after several chemical peel sessions
Conclusion: Chemical peels are a safe, affordable and effective technique to treat melasma and other dermatological pathologies. Their success depends on the practitioner’s training and appropriately selecting agents and protocols.
“Learning to doubt is learning to think” - Octavio Paz
Speaker: Dr Denise Steiner
Mechanisms and results:
Composition and formulas:
Application technique:
Conclusion: Phenol peels with croton oil are a powerful technique, but they require rigorous preparation, technical skill and post-operative care. Long-lasting results can be achieved, especially in cases of severe photoageing and melasma.
Speaker: Dr Felipe Ribeiro da Silva
Dr Ribeiro da Silva emphasised that the topic is extremely complicated. You must be very careful when performing chemical peels, because they can actually cause complications. The good news is that all complications are preventable. You can foresee the complication a little before it occurs. It usually gives warning signs.
He published two books together with Dr Denise Steiner: one on chemical peels and the other on complications in cosmetic dermatology, covering more than just chemical peels. All of these complications have already been described in the literature, so there is always some study or evidence to help in the treatment of these complications.
Regarding the large groups of complications, dyschromia, scars, infections and multifactorial complications are noteworthy. The presentation focused on dyschromia and infections.
The most common (and most easily treatable) dyschromia is post-inflammatory hyperpigmentation (PIH). Doctors, and especially resident dermatologists, fear this complication a great deal. However, it is not a real complication. It can occur as a “natural progression” in up to 76% of patients who undergo deep chemical peels. It is a preventable and treatable condition. Periocular and perioral areas are most commonly involved.
In early hyperpigmentation cases accompanied by erythema, he recommended 0.05% clobetasol propionate cream to reduce inflammation. For late hyperpigmentation (after 15–30 days), the choice depends on the sensitivity of the patient’s skin. For sensitive or erythematous skin, the option is 4% hydroquinone; for non-sensitive skin, Kligman’s formula, adjusting as necessary, considering that tretinoin causes irritation.
Hypopigmentation may also occur, more frequently in patients with phototype IV or greater and patients with frontal fibrosing alopecia, and is common after deep peels such as phenol ones. Some treatment techniques include narrowband UVB phototherapy, fractional laser, latanoprost, bimatoprost and melanogenesis stimulants.
The most common infections are viral (mainly herpes simplex and rarely Epstein-Barr). Pain is an important sign of infection (there are no blisters/vesicles) after peels. Pain is uncommon, even in the deepest peels. These infections can be serious and cause permanent scarring if not treated quickly. Prophylaxis with antivirals (valaciclovir with the most relevant posology) is recommended for all patients undergoing medium or deep peels. Bacterial and fungal infections are rarer but can occur, especially in patients who use antibiotics inappropriately or keep the area occluded. Consider Candida infection in the event of perifollicular lesions.
Dr Ribeiro da Silva concluded by inviting everyone to become a member of the International Peeling Society.
Coordinators Dr Ely Cristina Cortes Peralta, Dr Boris Fernando Sánchez Polanía, Dr Denise Steiner.
Speakers: Dr César Fernando González Ardila, Dr Denise Steiner, Dr Priscilla Zepeda Lopez, Dr Ely Cristina Cortes Peralta, Dr Angélica María Domínguez Duarte, Dr Boris Fernando Sánchez Polanía.
Speaker: Dr César Fernando González Ardila
Dr César Fernando González Ardila began by pointing out that melasma is a chronic, multifactorial inflammatory disease that has a significant physical and emotional impact on patients. He cited a recent study conducted at his clinic, which showed that the quality of life of patients with melasma is profoundly affected. He also mentioned the correlation between the severity and duration of melasma and quality of life, stressing that it is a chronic problem with frequent relapses, which requires a comprehensive therapeutic approach.
Dr González emphasised that although Kligman’s trio (developed in 1975) is still useful, it cannot be the only treatment for melasma. Patients expect more effective and sustainable results, especially in view of increasing competition from the treatments and results found on social media.
He stressed the importance of incorporating innovation and technology to exceed patients’ expectations.
A detailed analysis of the pathophysiology of melasma was presented, with an emphasis on...
Dr González presented evidence on the benefits of biostimulators in improving skin quality and luminosity in melasma patients. Studies have shown that biostimulators that are not combined with topical treatments or laser technologies can:
Dr González shared results of a pilot study conducted at his clinic, investigating the efficacy of polydioxanone (PDO) threads in melasma treatment.
Study methods:
Results:
Dr González concluded that for a long time it was believed that melanocytes were the only ones involved in melasma, but fibroblasts have been shown to play a crucial role.
Dr González emphasised the importance of thinking innovatively and creatively to achieve better results in melasma treatment. He also invited attendees to participate in the second edition of the Latin American Congress on Melasma and Pigmentary Disorders, to be held in Bogotá from 15–17 August, highlighting the resounding success of the first edition.
Speaker: Dr Priscilla Zepeda Lopez
Dr Priscilla Zepeda addressed skin ageing and how it impacts mainly on facial aesthetics, specifically in the lip area. Dr Zepeda mentioned that although ageing is inevitable, preventive care throughout life and appropriate treatments can significantly improve its impact.
Dr Zepeda explained that ageing is due to several factors, including environmental factors, diet, lifestyle and genetics. However, she stressed that the way we take care of ourselves over the years is crucial to mitigate the visible effects of ageing. One of the most important aspects of ageing is skin changes, which results in skin thinning, decreased fibroblasts and reduced collagen and elastin production, directly affecting skin turgor and volume. In addition, she mentioned decreased vascularisation, which contributes to a more haggard and aged appearance of the skin.
With regard to the lips, Dr Zepeda noted that perioral ageing is particularly evident. As we age, the lips lose volume and the upper lip tends to flatten. The Cupid’s bow, characteristic of youth, becomes less defined, and vertical wrinkles (barcodes) start to become more noticeable. In addition, the lower lip tends to invert towards the region of the lower labial commissure, giving the patient a more aged appearance. These changes are compounded by inversion of the labial commissures and loss of vascularity, resulting in pale, lifeless lips.
Dr Zepeda pointed out that ageing does not only affect the skin, but is an interactive process that starts from the deepest tissues. She pointed out that bone atrophy and bone and muscle resorption are key factors contributing to facial ageing. This process particularly affects the lower part of the face, where the nasolabial folds and cosmetic units are more pronounced, which can lead to a “tired face” or “grumpy face” appearance.
She mentioned the most popular and effective treatments, highlighting dermal fillers, peels, lasers, radiofrequency and other high-end technologies. In addition, she mentioned that many plastic surgeons have started using less invasive techniques, especially when facial rejuvenation is sought in delicate areas such as the perioral area.
Dr Zepeda shared her personal approach to lip beautification using the Nd:YAG laser. This technique has proven to be effective in treating skin changes in the perioral area, improving lip texture, vascularisation and, of course, volume and definition. Dr Zepeda noted that this technology has helped achieve natural, less invasive results in perioral rejuvenation, without the risks of more aggressive procedures.
Dr Zepeda concluded her talk by mentioning that ageing is an inevitable process, but with proper care and the use of advanced technologies, improving the appearance of and maintaining healthy, youthful skin is possible. She emphasised the importance of prevention and early treatment to ensure that patients age with dignity, while also prioritising their well-being and aesthetics.
The presentation was a useful introduction for healthcare professionals interested in perioral rejuvenation techniques, showing a balanced approach between science and aesthetics in the treatment of facial ageing.
Speaker: Dr Ely Cristina Cortes Peralta
Dr Ely presented the main types of complications with CaHA:
How to manage them?
By far the most common is nodule formation. In this case, minimal intervention involves creating a hyperdilution in the nodule with saline solution, sterile water or hyaluronidase, vigorous post-injection massage and repeating if necessary. Pharmacological (collagenase) or laser (Erbium/CO2) procedures are less frequently used.
For arterial occlusion, the use of acetylsalicylic acid 300 mg, hyaluronidase, prednisolone, sildenafil 50 mg/day for 3 days, subcutaneous heparin for 7 days, doxycycline, aciclovir and hyperbaric chamber may be considered. During follow-up, in the event of poor circulation, she recommends repeating the hyaluronidase injection, continuing acetylsalicylic acid, hyaluronidase and prednisone daily or evaluating other therapeutic options.
Speaker: Dr Angélica María Domínguez Duarte
Dr Angélica María Domínguez Duarte presented a technical presentation focused on non-invasive and minimally invasive aesthetic treatments to beautify the lips and perioral area. She stressed the importance of understanding facial anatomy, selecting personalised techniques and maintaining naturalness and dynamism in results.
Endnote: Dr Domínguez invited the professionals to continue perfecting their technical skills, keep up to date with facial anatomy and always prioritise patient safety in every aesthetic procedure.
Speaker: Dr Boris Fernando Sánchez Polania
Introduction: Dr Boris Fernando Sánchez Polanía began his talk by emphasising how skin quality not only influences patients’ self-perception, but also their emotional health, quality of life and social interactions. However, despite its importance, the concept of skin quality has been underestimated in rigorous clinical studies, and the terminology used to describe it varies considerably from one professional to the next.
Definition of skin quality: Dr Sánchez explained that skin quality can be assessed through 16 key attributes, including:
These attributes serve as an objective guide for doctors in assessing skin condition and establishing a common language to describe it.
The role of the extracellular matrix in skin ageing: According to Dr Sánchez, skin ageing is related to structural changes in all skin layers, with special emphasis on the extracellular matrix (ECM). This structure provides biochemical and cellular dermal support and is essential for maintaining healthy skin.
Fibroblasts have been highlighted as playing an important role in the synthesis of ECM components, including collagen and elastin fibres. With ageing, these fibres fragment due to the action of enzymes such as metalloproteinases, resulting in dermal collagen fragmentation -> ECM degradation -> fibroblast collapse.
This collapse reduces collagen and elastin production, contributing to sagging, loss of elasticity and other signs of ageing.
Procedures to improve skin quality: Dr Sánchez highlighted three main approaches supported by scientific evidence to intervene in skin quality:
Clinical evidence and outcomes: Studies were presented showing how combination treatments can significantly transform skin quality:
Dr Sánchez shared case reports where combination therapies were used, highlighting:
Combination techniques: The suggested protocol includes:
Results:
Conclusions: Dr Sánchez ended by emphasising that treating skin quality goes beyond combating the superficial signs of ageing. It involves a holistic approach that combines science, technique and art to address the specific needs of each patient. This approach not only improves appearance, but also enhances patient confidence and emotional well-being. “We cannot stop ageing, but we can accompany our patients in this process, helping them to age at their best”.
Coordinators: Dr Daniel Alcala Perez
Speakers: Dr Daniel Alcala Perez, Dr Angélica María Domínguez Duarte, Dr Rosa Olivera, Dr Javier Ruiz Ávila, Dr Judith Montiel.
Speaker: Dr Daniel Alcala Perez
Dr Daniel Alcala Perez examined the innovative features and evolving applications of botulinum toxins, highlighting the latest developments in serotypes, liquid formulations and alternative uses in fields such as neurology, dermatology and advanced aesthetics.
Dr Alcala detailed the historical and scientific progression of botulinum toxins from their earliest versions to current formulations. He mentioned:
Dr Alcala emphasised the following innovative uses of botulinum toxin:
Dr Alcala stressed the importance of being familiar with the specific anatomy of each patient to achieve optimal results. Some advances include:
Dr Alcala mentioned the occurrence of unusual allergic reactions, such as erythema and pruritus at the application site, even with well-known toxin brands. Areas of inconclusive research were also addressed, such as the use of the toxin for:
Emerging techniques were discussed such as “Barbie Botox”, used to make the neck slimmer and longer through 6 injection points (5 units per point) in the bilateral trapezius muscle. This trend has become popular thanks to being promoted on social media.
Dr Alcala concluded by stressing the importance of natural results and the ongoing progress in botulinum toxin research. He stressed the need to personalise every treatment and to keep up to date with the latest scientific findings to ensure safety and effectiveness when applying treatment.
Speaker: Dr Angélica María Domínguez Duarte
Dr Angélica María Domínguez Duarte discussed advanced botulinum toxin application techniques to treat various facial muscles. Her presentation focused on functional anatomy and TIPS on how to optimise natural aesthetic results while avoiding undesirable effects:
Dr Domínguez emphasised the importance of understanding facial anatomy and muscle dynamics to ensure safe, effective and natural results in botulinum toxin use. She concluded by thanking attendees and stressing the importance of a careful, personalised and evidence-based application.
Speaker: Dr Rosa Olivera
Dr Rosa Olivera began her talk by focusing on botulinum toxin treatments for hyperhidrosis, highlighting her experience with the botulinum toxin brand and the development of international guidelines for its application. The presentation included practical advice on how to treat various areas of the body, starting with the underarms, the use of appropriate units and the importance of using 100 or 500 unit vials, depending on the case.
Key points:
Dr Rosa Olivera concluded that the key to success in hyperhidrosis treatment with botulinum toxin lies in personalising the treatment and selecting the appropriate doses and application techniques according to patient needs, ensuring long-lasting and natural results.
Speaker: Dr Javier Ruiz Ávila
During his lecture, Dr Javier Ruiz Ávila addressed the most important aspects of botulinum toxin use in perioral therapy, emphasising the importance of applying appropriate and personalised doses for each patient. He mentioned that although botulinum toxin is a recurrent and well-known topic in aesthetics, it is still a topical issue due to its effectiveness and the constant development of new techniques.
In summary, Dr Javier Ruiz Ávila’s lecture provided valuable insights into modern techniques and the appropriate use of botulinum toxin, while highlighting the importance of personalising treatments for every patient and maintaining realistic expectations in aesthetics. He also emphasised the use of innovative technologies and treatments, such as liquid threads and biostimulants, to provide optimal results without compromising the naturalness of facial expressions.
Parte inferior do formulário
Speaker: Dr Luz Helena Pabón Ospina
Dr Luz gave an example of the case of a 52-year-old patient who used 44 units of onabotulinum toxin plus a booster of 7 units of botulinum toxin with satisfactory results, but returned 5 weeks after the application complaining of loss of toxin effect. On the same day this patient was treated, her mother and sister were treated with the same brand and batch of toxin and had an excellent response, with no need for boosters.
Botulinum toxin therapeutic failures have been a topic of discussion since 1988. She explained that this failure can be classified into...
Those who do not respond to the first application and subsequently with new applications
Reasons for therapeutic failure include: doses are too low, injection into the incorrect muscle and muscle contractures, prior botulism, previous vaccination, improper storage/degradation of BoNT.
Those who stop responding after a period of effectiveness
Reasons for therapeutic failure include: presence of neutralising antibodies (53.5%), insufficient doses, mislocalisation, change in muscle activity patterns or disease progression, aggressive reconstitution, inadequate storage, genetic factors–HLA, autoimmune diseases
- High doses per session, high cumulative doses (Dr Pabón stressed that cumulative doses of botulinum toxin should not exceed 400 units in a three-month period. Furthermore, she stressed that doses for cosmetic purposes are considerably lower than those for medical or neurological uses)
- Use of RimabotulinumtoxinB
- Short intervals/booster 1–2 weeks after initial session
- Injection near lymph nodes (neck)
- Autoimmune diseases.
A study by José et al. reviewed by Dr Pabón in 2021 showed promising results in patients who received type A toxin at week 12, with significant improvements at week 14. This suggests that immunological and neurological factors play an important role in therapeutic failure.
Appropriate dilution and correct dosage, correct storage and avoid the use of open vials for longer than a certain period of time, appropriate time period between applications (a minimum of 12 weeks, coordinate application times with other speciality treatments to optimise results). Consider using incobotulinumtoxinA in the event of secondary failure.
In the event of secondary therapeutic failure, Dr Pabón suggested that a break from the toxin may be necessary (a 1- to 2-year holiday), and some research has also suggested considering the use of zinc (although this is a controversial topic).
Coordinators: Dr Paula Peter Brayne, Dr Yadira Diaz.
Speakers: Dr Paula Peter Brayne, Dr Martha Miniño Brea, Dr Jennifer Frías, Dr Elda Giansante, Dr Susana Misticone Moreno, Dr Yadira Diaz.
Speaker: Dr Paula Familia Peter Brayne
The conference focused on the relationship between autoimmune diseases and cosmetic procedures, examining the differences between the innate and adaptive immune systems, factors affecting immunity in the skin, and the precautions needed when treating patients with autoimmune pathologies.
The conference highlighted the need for the holistic and personalised treatment of patients with autoimmune diseases seeking cosmetic procedures, always prioritising their safety and well-being.
Speaker: Dr Martha Miniño Brea
Dr Miniño Brea takes a holistic approach to treating patients with autoimmune diseases. She stressed the need for a change of attitude towards life, modifying behavioural patterns, lifestyles and ways of thinking that can cause inflammation. Her presentation examined contraindications, factors that perpetuate inflammation and the care to be considered in these patients, including cosmetic aspects.
Final message: Treatment adherence and a multidisciplinary approach are key to ensuring a better quality of life for patients with autoimmune diseases.
Speaker: Dr Jennifer Antonia Frías Mendez
Dr her presentation, Dr Jennifer Frías addressed the application of aesthetic procedures in patients with autoimmune diseases, specifically systemic lupus erythematosus (SLE) and other connective tissue diseases. She highlighted the delicate balance between the functional and aesthetic benefits and the risk of disease reactivation. In addition, she presented relevant case reports and literature reviews that support current practices.
Strict criteria prior to procedures:
Speaker: Dr Susana Misticone Moreno
Dr Susana Misticone Moreno began her talk by addressing the positive impact that laser technologies have on dermatology and how they have evolved to become indispensable tools for treating various conditions, including collagenopathies. These diseases, although complex, should not prevent patients from receiving aesthetic and therapeutic benefits from lasers. During the conference, Dr Misticone examined case studies, scientific evidence-based recommendations and her personal experience in applying lighting technologies in this type of pathology.
The dermatologist explained that the use of lasers in patients with collagenopathies has been controversial in the past due to fears of autoimmune disease exacerbation. However, recent studies and clinical experience have shown that these technologies can be safely applied to patients with diseases such as lupus erythematosus, scleroderma and morphoea, provided that appropriate protocols are followed.
Dr Misticone emphasised that light technologies have both aesthetic and functional applications, significantly improving patients’ quality of life. The main advantages include:
The dermatologist shared strategies to maximise laser effectiveness and safety in these patients:
Dr Misticone shared a list of principles for the safe and effective treatment of patients with collagenopathies:
Dr Misticone concluded her presentation by stressing that lasers are indeed safe and effective tools for patients with collagenopathies when used properly. You must know the parameters to correctly treat patients. Always use the lowest possible fluences; avoid when there is activity. She invited dermatologists to lose their fear and adopt these technologies, always emphasising well-defined protocols, constant monitoring and being an INTELLIGENT operator.
Speaker: Dr Yadira Diaz
Dr Yadira began her talk by suggesting that we need to take a very careful look at patients with autoimmune disease. There is a limit on aesthetic procedures in these patients.
Botulinum toxin is NOT contraindicated in autoimmune diseases. Unfortunately from a scientific point of view there is still no answer because there are very few scientific studies and evidence. A study in over 500 patients concluded that as long as the disease is controlled, Botox appears to be safe. The disease must be controlled for at least 3 to 6 months, the patient must not be on corticosteroids and must have no complications from previous applications.
Fillers, biostimulators and threads can act as a foreign body, despite being biocompatible, and can cause intentional immune reactions. If inflammatory response is excessive or becomes chronic, an adverse effect will occur. PLLA and HA non-permanent fillers are recommended for LE patients.
She presented the case of a 64-year-old patient using filler (HA) and BoNT in 2016, who developed oedema and hyperpigmentation after eyelid hydration for injection, and reinforced that “when nothing is safe, anything is possible”.
Coordinator: Dr Carlos Quiroz
Speakers: Dr Maria Paulina Estrada Fernandez, Dr Carlos Quiroz, Dr Maria Rosario Peralta, Dr Nathalie Quiroz Valencia, Dr Carlos De La Roche, Dr Mario Gastón Toledo Lelevier.
Speaker: Dr Maria Paulina Estrada Fernandez
HOW TO GET STARTED?
She suggested starting with five basic points:
Defining the brand’s DNA is essential to be clear about the principles, values and objectives that will guide the path forward and remain consistent over time. In addition, a solid management structure from the outset, aligned with objectives, is the key to success. However, to achieve these goals, you must surround yourself with experts to help with unfamiliar administrative processes, while remaining in control and being actively involved at every stage.
Planning is crucial to maintain order and guide important decisions, such as staff recruitment, defining services and acquiring equipment. This should always occur through a process of ongoing learning. Objectives should follow the SMART rules: they should be specific, measurable, achievable, relevant and time-bound. These larger objectives are often broken down into smaller goals, where the whole team must be involved to ensure coherence and collaboration. Strategic consistency is vital, setting short-term (such as digital strategy), medium-term (time management and reducing waiting times) and long-term (expansion with new staff) objectives.
In order to define an action plan, you must analyse the current status and develop strategies to achieve your final objectives. This involves identifying indicators of success, concrete actions, responsible parties, necessary (financial and human) resources and defined deadlines.
There are useful tools to facilitate this process: the SWOT matrix for macro strategies, resource analysis with budgets and timelines (such as Google), and time management through agendas and deadlines (tools such as Trello).
She described the SWOT technique, a strategic analysis tool used to assess the status of an organisation, project or specific situation. SWOT is an acronym that stands for:
The clinic’s strengths include the dermatologist’s experience and expertise, advanced diagnostic and treatment technology, a good relationship with patients, a strategic location and a good reputation. Opportunities include growth in treatment demand, potential alliances with other clinics and professionals, increased interest in skin health, digital marketing and the use of telemedicine. However, there are weaknesses such as dependence on a single professional, limited capacity for care, lack of online visibility, high equipment and technology costs, and limited administrative resources. Finally, threats include regulatory changes, economic crises and changes in consumer behaviour.
However, in the end evaluating and adjusting is always necessary, analysing the achieved vs planned results and making adjustments according to actual results.
As an example, she mentioned the high-budget advertising campaign that she paid for at the start which did not produce the expected results. From that moment on, she took campaign courses to be able to do it herself and to be able to approach it according to her objectives.
She ended her presentation by concluding that strategic planning provides a clear focus and vision, ensuring that objectives are aligned with your brand DNA; an appropriate management structure; and continuous evaluation as key elements for success.
Speaker: Dr Carlos Quiroz
Because a dermatologist must understand their own business model, he again mentioned the SWOT method to understand which business model is most appropriate for every individual.
Threats include high complexity, multiple patient options in the medical market, and high expectations, while the main challenges are growth, resource management and maximising profitability.
With all the difficulties and threats, there are also positive pressures that force us to distinguish ourselves not only as regards dermatological expertise, but also in the way we deliver services.
He argued that we need to become familiar with profitability, which will ultimately be the most important resource to provide a better service to patients.
He therefore suggested that the strengths to take advantage of all these opportunities can be found in a well-constituted and implemented business model.
Business models or strengths enable strategic decision-making, optimising resources, identifying opportunities, adapting to market changes, improving patient experience and controlling costs and expenses, while differentiation through medical growth and service quality represents a key opportunity.
What is a business model?
It is the set of strategies, processes and practices that a company uses in order to deliver and calculate value.
The concept of value does not only refer to money, but the concept of value varies according to the market. In the case of doctors, the main value is in patients. So in medicine, the value of the business is often in the way you gain, treat and retain patients.
There are thus different components to the business model, but he stressed that the patient must always be at the centre.
Business model components:
Conclusion: properly building your business model does not guarantee that you will achieve what many have achieved, but it does help you to follow what you have set out to do.
Speaker: Dr Mario Gastón Toledo Lelevier
He based his talk on how to create social media content, in order to enhance your medical practice, without losing sight of your objective.
Social media, although not essential, are a free and valuable tool to reach more patients and make your work known. It is key to avoid direct sales. Instead, provide useful content, such as information that adds value. When creating videos, the essential thing is to generate emotions in and be useful to the consumer. An example is to tell a sequential story. First, show a “before and after” image to get them excited, followed by information that explains the case and adds value. Personal promotions should not be included; these may be exclusive to the clinic.
He explained 5 keys to real growth in social media as a doctor:
Some more tips for making videos:
Speaker: Dr Nathalie Quiroz Valencia.
She explained the keys to a good working team.
A good team is essential to improve efficiency in medical care, ensuring a fast and personalised service, as well as optimising time and reducing errors, which has a direct impact on clinic profitability. Staff selection should be based on searching for qualified individuals with technical and social skills, aligned with the clinic’s values. It is important to involve the current team in the process, conduct in-depth interviews and provide ongoing training to encourage personal and professional development. In addition, setting clear and achievable goals motivates the team, while recognising achievements strengthens the sense of belonging and reinforces positive behaviours.
Leadership plays a key role, as you must be exemplary, show enthusiasm and be willing to listen to your team. In addition, regular follow-up through periodic meetings and opportunities for promotion contribute to maintaining a positive working environment, where collaboration, respect and trust are valued. A well-trained team not only improves patient care, but also increases job satisfaction and the profitability of the practice, which promotes the growth and success of the clinic.
Speaker: Dr Mario Gastón Toledo Lelevier
An effective marketing strategy, based on digital and traditional content, should focus on brand positioning and credibility, preserving the doctor’s reputation, attracting new patients, and fostering patient retention and loyalty.
It is important to use the same material on all social media, as the audience of each is different.
However, it all comes together on Instagram where it is important to have a Linktree so that patients can access appointments, products, etc.
On Instagram, the first story should generate excitement or interaction (such as a “before and after” image or a question box) to increase your reach throughout the day. It is important to post content daily, with a maximum of 8 stories, all uploaded at the same time to take advantage of the algorithm. Stories should follow a sequence, alternate backgrounds every two or three posts and measure audience interaction to adjust future content.
TikTok is an ideal platform to make content viral, especially with daily live streams. Content should be consumed for inspiration and to maintain message congruence.
Podcasts are an opportunity to share high-quality information with patients, create relationships through guests and position yourself in the health area, reaching a different audience profile.
In WhatsApp Business, using quick responses, personalising them according to patient needs and having an updated catalogue of services are key.
For videos, he suggested following the anatomy of a reel: a clear introduction, a body with useful content and a call to action at the end. It is key that the videos are short, with no pauses, with varied backgrounds and focused on your speciality. Use them to segment your market. For example, if you work with lasers, create content about melasma and hyperpigmentation. Avoid mentioning specific brands or products.
Value your service: how to price your services appropriately
Speaker: Dr Carlos Quiroz
Aspects to be taken into account in price allocation: He suggested that the main thing is to be clear on what the expenses and profit margins are and then to be able to assess the following points.
He suggested starting by making a list of the tasks necessary to be able to allocate prices.
He gave an example considering that the hourly office cost is $100 and you want to have a profitability of 30%, for example (He clarified that the cost of profitability is up to each individual).
He suggested the following calculation to determine the sales price:
Sales price = (total cost)/(1-margin) = &00/(1-0,3) = 100/0,7 = 142
Considering the example above, in order to have a 30% return, if the cost price is 100, the sales price should be 142.
Conclusion: Taking into account the total expenses adjusted for the time to perform the work is the starting point to initiate a proper pricing strategy.
Speaker: Dr Carlos De La Roche
The main goals in creating a company are to recover the initial investment, generate passive income, improve quality of life, ensure company sustainability, foster employment and build a replicable organisational culture.
Coordinators: Dr Esperanza Melendez Ramirez and Dr Mariela Tavera Zafra
Speakers: Dr Diego Mendez Villanueva, Dr Verónica Rose Marie Rotela Fisch, Dr Marius Anton Ionescu, Dr Ramon Pigem Gasos.
Speaker: Dr Diego Mendez Villanueva
He first reminded us of some concepts and then focused on his presentation.
Demodex spp. is a commensal ectoparasite found in 23–100% of healthy adults. However, this mite has been found to be more prevalent in patients with rosacea. However, the literature is discordant on this percentage.
The objective of the presentation is to compare the sensitivity of standardised skin surface biopsy (SSSB) and direct microscopic examination (DME) in patients with rosacea and, secondarily, to determine the prevalence of Demodex spp. infestation in patients with rosacea.
Both are considered positive when mite density is greater than 5/cm².
The author presented a cross-sectional research study in patients with rosacea in 2 dermatological departments that lasted 8 months. The study enrolled sixty-one patients with erythematotelangiectatic and papulopustular rosacea, aged 18 years and over. Dermoscopy was compatible.
Exclusion criteria: Ocular or phymatous rosacea, other dermatological diseases, recent treatment (less than 3 months)
Each patient underwent both techniques in clinically significant areas. Demodex count, delay time for each technique and associated pain were assessed.
Results: Infestation of up to 62% was detected in patients with standardised skin biopsy compared to 28% with DME. Mite density for the standardised skin biopsy was 30.08 mites per square centimetre compared to the direct microscopic examination with 5.56 mites per square centimetre.
Associated pain was measured via visual analogue scale with 2.7 points for standardised skin biopsy and 2.02 points for DME. No significant differences were detected
He explained that these differences could be due to the fact that cyanoacrylate adheres to the mite and removes it completely, as opposed to the other technique where it is removed rather fragmented.
In conclusion, standardised skin biopsy is a more reliable method. Up to 64% of rosacea patients are infested with Demodex spp.
DME underestimates mite density.
These findings led SSSB to be considered the standard technique at the participating sites.
Speaker: Dr Verónica Rose Marie Rotela Fisch
Dr Verónica Rotela presented a descriptive study on the use of botulinum toxin in mesotherapy (mesotoxin) as an alternative treatment for rosacea. This study was conducted in 2023 in a medical centre in Asunción, Paraguay.
The objective of the study was to determine the efficacy of botulinum toxin mesotherapy in the treatment of rosacea by identifying the clinical and biological characteristics of patients, assessing the specific components of improvement, and analysing how the decrease in erythema and flushing could be related to the blockade of neurotransmitters involved in vasodilation and the regulation of vascular endothelial growth factor.
An observational, descriptive and retrospective study was conducted. Thirty patients with rosacea treated with botulinum toxin mesotherapy in 2023 were included.
Assessment was carried out using conventional photographs, Reveal camera photographs (vascular and pigment structure), applying a modified scale and assessing changes in the different rosacea components.
The technique used was injections in uniform micropapules, 0.05 ml of solution at 1 cm intervals in grids, intradermally, with 10 IU per cheek (100 IU diluted in 5 cc of normal saline).
The following characteristics were present:
The results concur with previous studies in Colombia, Peru, the United States and Korea, which highlight the efficacy of botulinum toxin in reducing erythema and other associated symptoms.
Botulinum toxin mesotherapy was shown to be effective in all of the rosacea subtypes included, highlighting its potential off-label use.
It is proposed in theories to refer to decreased erythema and flushing, taking into account neurotransmitter blockade and even vascular endothelial growth factor regulation.
In conclusion: subjective and objective clinical improvement was found in all patients, with a predominance of female patients, age under 40 years, phototype III and erythematotelangiectatic rosacea. There was a significant decrease in erythema, telangiectasias, papules and pustules in the objective component of rosacea, which identifies less noticeable structures, so clinical improvement is not necessarily similar.
It is important to conduct further studies that assess the duration of effects, include validated tools (RosaQoL) and have larger patient samples. Mesotoxin may be considered to be a promising alternative for rosacea treatment.
Speaker: Dr Marius Anton Ionescu
He mentioned “interactomes”, which involve interactions between microbes, host cells, pathogenic bacteria and saprophytes.
The term microbiome is used when the microbiota is accurately determined by metagenomic analysis. This difference has been widely highlighted in recent years. Microbiota: A set of commensal, pathogenic and symbiotic microorganisms that inhabit the human body. Microbiome: It includes these microorganisms as well as genes and metabolites arising from interaction with the environment and host.
The pathophysiology of acne is more complex than hyperseborrhoea and hyperkeratinisation. Factors such as Toll-like receptors, lack of antimicrobial peptides and changes in the microbiome contribute to the problem. A notable change in the microbiome is the dominance of Cutibacterium acnes (C. acnes) ribotypes RT4 and RT5 (more anaerobic), which are pro-inflammatory and more virulent due to the production of biofilms that perpetuate inflammation and generate antibiotic resistance.
Staphylococcus epidermidis competes with the C. acnes ribotypes RT4 and RT5, inhibiting their proliferation. Recent studies investigate the use of topical S. epidermidis applications as a new strategy in acne treatment.
In addition to conventional treatments, new approaches are being explored including:
A clinical study was conducted in acne patients using a cosmeceutical emulsion formulated with 2 patents, TLR2-REGUL and MPA-REGUL, twice daily for two months. The following was found:
In addition, metagenomic analyses were performed with 16S ribosomal DNA sequencing, identifying 10 known C. acnes ribotypes and 36 S. epidermidis subtypes.
In conclusion, a correlation was found between clinical improvement and restoration of skin microbiome balance. These findings are available in an open access article in PubMed and were presented at the American Academy of Dermatology (AAD) last March.
Ionescu, M.-A.; Tatu, A.L.; Busila, C.; Axente, E.R.; Badalato, N.; Feuilloley, M.G.J.; Asquier, E.; Martínez, J.D.; Lefeuvre, L. Microbiome Modulation in Acne Patients and Clinical Correlations. Life 2024, 14, 688. https://doi.org/10.3390/life14060688
Speaker: Dr Ramon Pigem Gasos
He presented a case series on the use of peels and masks in monotherapy and as adjuvant therapy in patients with rosacea and acne.
He had a conflict of interests with the pharmaceutical company Mesoestetic.
The main points are detailed below:
Final message: Peels and masks are useful therapeutic tools in dermatology, both in monotherapy and in combination therapy, offering tangible benefits in rosacea and acne.
Speaker: Dr Eduardo Rivera Perdomo
He reminded us that erythematotelangiectatic rosacea, characterised by persistent facial erythema, telangiectasias and symptoms such as burning and pruritus, has a profound emotional and social impact on patients. This study aimed to evaluate the safety and efficacy of pulsed dye laser, botulinum toxin and their combination as novel therapies in cases refractory to conventional treatments.
Pulsed dye laser (PDL): its chromophore is oxyhaemoglobin, its energy is dissipated in the form of heat to generate vascular lesions, generating immediate purpura. It has anti-angiogenic and anti-inflammatory effects.
Botulinum toxin: It inhibits the release of inflammatory mediators such as substance P, calcitonin gene-related peptide and vasoactive intestinal peptide, and it reduces cathelicidin LL-37-induced erythema, mast cell degranulation and mRNA expression, thus having an anti-inflammatory effect in the skin.
Clinical characteristics (presence of telangiectasias, facial involvement, extrafacial involvement, flushing and pruritus) were assessed. Quality of life using the SKINDEX-29 scale; adverse events (pain, erythema, purpura, facial asymmetry, hypopigmented macules); degree of satisfaction; and post-procedure recommendation of treatments were also assessed.
This study demonstrates that both laser dye and botulinum toxin, in monotherapy or in combination, are effective and safe treatment options for erythematotelangiectatic rosacea. In addition to improving clinical signs, these therapies had a positive impact on patients’ quality of life and emotional well-being, with a low incidence of adverse effects. This opens up new possibilities for refractory cases.
They concluded their presentation with illustrative case studies showing “before and afters” for procedures, highlighting both the clinical and emotional transformation in treated patients.
Coordinators: Dr Esperanza Melendez Ramirez and Dr Mariela Tavera Zafra
Speakers: Dr Michelle Alcocer-Salas, Dr Jeyson Montero Castaño.
Speaker: Dr Michelle Alcocer Salas.
She presented a case of erosive pustular dermatosis of the scalp in a 94-year-old female patient with a history of actinic keratosis previously treated with 5-fluorouracil. The patient went in with a lesion that initially presented as a small papulopustule on her forehead, which increased in size and progressed into an erythematous plaque with eroded areas, yellowish scabs and well-defined borders on the scalp. Dermoscopy revealed the absence of follicular openings, reddish areas, oily exudate and yellowish scabs, so a biopsy of the lesions was taken. The following were put forward as differential diagnoses: pemphigus, seborrhoeic dermatosis and tinea.
Histopathological analysis showed atrophic epidermis, subcorneal pustules and an inflammatory infiltrate composed of neutrophils, lymphocytes and histiocytes, with skin atrophy and solar elastosis. Mycological cultures were negative, confirming the diagnosis of erosive pustular dermatosis of the scalp.
She then gave a brief description.
It was first described in 1979 by Burton and primarily affects older adults, mostly women. It is important to mention that the pathogenesis of the disease is not fully understood, but it is associated with androgenic alopecia, chronic actinic damage and trauma. In addition, topical medicinal products (e.g. 5-fluorouracil), infections and surgical procedures may be involved in its development, although no definitive relationship has been established.
Clinically, it mainly affects the vertex and frontal region, is asymptomatic and manifests with pustules, erosions, yellowish scabs and, in some cases, scarring alopecia due to chronic inflammation. Dermoscopy shows absence of follicular openings, superficial blood vessels and, in some cases, atrophy revealing hair bulbs. Histopathology is not specific but is crucial to differentiate it from other diagnoses such as squamous cell or basal cell carcinoma and other neutrophilic dermatoses.
The recommended treatment depends on whether or not the patient has severe atrophy. Topical calcineurin inhibitors are indicated in the event of atrophy. In the absence of atrophy, topical corticosteroids can be used.
In the cases presented from the Instituto Dermatológico de Jalisco, three patients (all women, mean age 80 years) were treated with topical corticosteroids, with significant improvement in their skin condition.
Early diagnosis of this disease is essential to avoid sequelae and improve patients’ quality of life. Early detection facilitates timely treatment and prevents the progression of chronic inflammation. This type of dermatosis is rare and in many cases underdiagnosed, so it is important to keep clinical suspicion high for its diagnosis.
Speaker: Dr Jeyson Montero Castaño
Telogen effluvium is a common cause of hair loss characterised by increased hair loss due to hair growth cycle disturbances. It usually occurs after stressful events and can be classified as acute (less than 6 months) and chronic (more than 6 months).
The speaker named the pathophysiological mechanisms proposed by Dr Rebora:
- Premature teloptosis: accelerated hair release due to proteolysis of cadherins and telogen hair release, and high TNF-alpha levels. It can be triggered by endogenous factors (such as seborrhoeic dermatitis) or exogenous factors (such as exposure to UV radiation or medicinal products).
- Collective teloptosis: synchronisation of hair cycles resulting in massive hair loss, common in newborn hair loss, the postpartum period or with the chronic use of oral contraceptives
- Premature entry into the telogen phase: caused by cytostatic drugs, nutritional deficiencies (iron deficiency anaemia, vitamin D deficiency) or autoimmune diseases such as Hashimoto’s thyroiditis. Common symptom: trichodynia.
He mentioned trichodynia (painful or uncomfortable sensation in the scalp) as a symptom. It may be related to vitamin B12 deficiency and other autoimmune conditions, so it is essential to identify specific patterns of alopecia and rule out other conditions, such as androgenic alopecia.
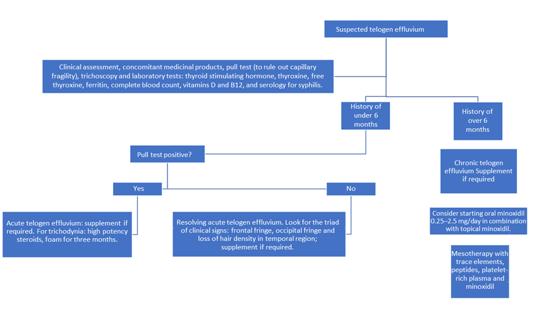
He proposed the following diagnostic algorithm :
As treatment strategies he proposed:
Nutritional support: Correct deficiencies, especially iron and vitamin D, which are common in telogen effluvium.
Pharmacological treatments:
Monitor response to treatment at 3 months. If there is no improvement, consider a scalp biopsy to rule out other conditions.
Coordinators: Dr Esperanza Melendez Ramirez and Dr Mariela Tavera Zafra
Speaker: Dr Claudia Mateo.
Speaker: Dr Claudia Mateo.
The presentation began with an overview of the use of 30% metformin cream as a therapeutic alternative to treat melasma, a chronic skin condition characterised by hyperpigmentation, which primarily affects women in their 30s and 40s. This condition is associated with increased activity in the melano-epidermal unit, especially in sun-exposed areas.
The speaker highlighted the role of melanocytes, cells responsible for pigment production through a complex process known as melanogenesis. Recent research suggests that other cells, such as keratinocytes, fibroblasts and mast cells, also contribute to the condition. Key phenomena include:
She then focused on inappropriate melanocyte activation.
Inappropriate melanocyte activation is mainly triggered by ultraviolet radiation, which causes DNA damage to keratinocytes, increasing the production of proopiomelanocortins that cleave the alpha-melanocyte-stimulating hormone. It activates different signalling pathways by stimulating melanocytic activity. Several intracellular signalling mechanisms are involved, including the following:
Treatment should address photodamage, hyperpigmentation, cellular stress and neovascularisation.
In 2014, the first study on the use of topical metformin was published. Metformin has been studied for its potential in melasma treatment due to its effects on adenosine monophosphate (AMP) signalling pathways. Metformin reduces AMP expression, thereby inhibiting melanogenesis. Studies have shown that metformin is non-toxic to normal cells, including melanocytes and keratinocytes, and can inhibit the proliferation of melanoma cells.
She described the clinical study conducted:
A quasi-experimental study was conducted at Hospital Universitario de Caracas between January and October 2023, in 30 women diagnosed with melasma. A “split-face” design was used to compare the efficacy of metformin cream versus a control group using 4% hydroquinone. The study was divided into three phases, all of which involved photographic recording, Hemi-mMASI and side-effect reporting.
Results
At the end of the study, 88% of patients expressed satisfaction with metformin treatment, while 100% expressed satisfaction with hydroquinone.
The study concluded that topical metformin is an effective and safe treatment for melasma, providing significant improvements in pigmentation and patient quality of life. These findings support the continued study of metformin in dermatological applications beyond its traditional use.
Coordinators: Dr Minerva Gomez Flores, Dr Antonio Massa, Dr Patricia Troielli.
Speakers: Dr Andrea Santos Muñoz, Dr Franz Barnes, Dr Carla Muñoz Olate, Dr Carlos Montealegre Gomez, Dr Jannell Obregon Alzamora, Dr Minerva Gomez Flores, Dr Paulo Jorge Tavares da Silva Lamarão, Dr Vicente Manuel Navarro Lopez and Dr Patricia Troielli.
Speaker: Dr Andrea Santos Muñoz
She began her presentation with a brief introduction.
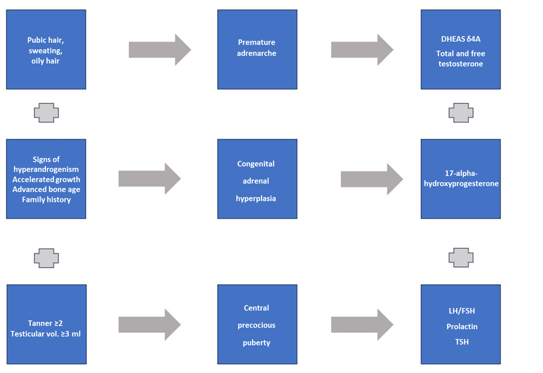
Acne is one of the most common diseases that can occur starting in the first days of life, preceding the first signs of pubertal maturation. It affects 90% of adolescents and about 20% of newborns. The pathogenesis is similar in all age groups, although INFANTILE acne may be a marker for other pathologies, requiring additional clinical studies in some cases.
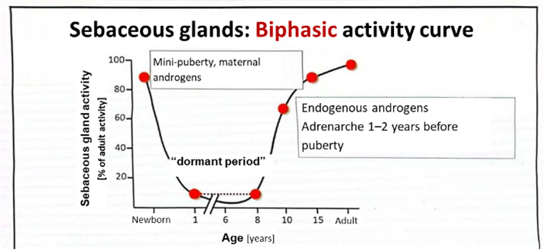
She used the following graph to show how sebaceous gland activity is biphasic, being silent between the age of one year and 8 years, a period in which the onset of lesions should be striking.
Classification of acne in paediatrics:
| TYPE OF ACNE | AGE | MORPHOLOGY | LOCATION | ASSOCIATED SYSTEMIC DISEASE |
| Neonatorum | 0–2 months |
Erythematous papules and papules/pustules Few comedones |
Cheeks, chin, eyelids and forehead | Rare |
| Infantile |
2 months to 1 year |
Papules, pustules, few comedones | Cheeks | Rare |
| Mid-childhood | 1 to 7 years | Comedones, inflammatory papules, pustules and nodules | Forehead, chest, back | YES |
| Pre-adolescent | 7 to 12 years | Comedones, inflammatory papules, pustules, nodules and cysts | Forehead, cheeks, chest and back | Rare |
| Teenage | 12 to 18 years | Open and closed comedones, erythematous papules | Forehead, nose, chest and back | Rare |
In more detail, she then named some of the main characteristics of each.
With regard to treatments, the important thing is that they are safe, simple to carry out and easy for the patient and carer to adhere to. Also explain that most treatments are off-label. It is generally no different from adult treatment except that tetracyclines cannot be used in children under 8 years of age and isotretinoin cannot be used in children under 12 years of age.

It is important to bear in mind that most cases are usually mild and thus dermocosmetics can be a great ally. It is important to protect and restore the skin barrier and microbiome at every stage of treatment.
Speaker: Dr Franz Barnes
He outlined 4 strategies for using social media as allies.
Challenges to overcome:
Speaker: Dr Carla Muñoz Olate
She began her lecture by outlining the WHO definition.
Acne in young people: 10 to 24 years old
Adult acne in people over 24 years of age
She discussed the differences between adolescent and adult acne.
| Characteristics | Teenage acne | Adult acne |
| Age | 10–19 years (a) | >25 years |
| Gender | More common in men | More common in women |
| Severity |
Mild: comedonal type Severe: nodulocystic type |
Generally mild inflammatory-papular type |
| Location | Affects the face: cheeks, trunk | Affects the face: cheeks, chin, mandible, rare trunk involvement |
| Type of lesion | Comedones | Inflammatory papulopustular lesions |
| Comedones | Common | Rare, but more common in smokers |
| Inflammatory papules | Common | Very common |
| Cysts | They may be present, depending on severity | Rare |
| Scars | Depending on severity | Common |
| Sebum production | Increased | Increased |
| Microbial flora | Cutibacterium acnes (C. acnes) | Cutibacterium acnes (C. acnes) |
| Hormonal disturbance | May be present | Very common |
| Response to treatment | Good | Frequently refractory/relapses common |
(a) Acne occurring between the ages of 10 and 24 years should be referred to as “juvenile acne”.
Treatment can follow the Academy’s guidelines recently published this year, although the major therapeutic challenge is not about the algorithm, but about how we achieve adherence to treatment in these patients.
Some tips she recommended to achieve this: give written instructions, avoiding complicated regimens, making use of combined agents to reduce the number of products. Explain proper use (on the entire area, not occasional) and possible adverse effects.
With regard to spironolactone, she reviewed the indications for its use in both adults and female adolescents:
Finally, with regard to acne and BMI, she said there is no consensus, with contradictory results on any relationship. Therefore, focusing on diet is discouraged, as the adolescent population is highly prone to eating disorders. Only suggest healthy habits.
Speaker: Dr Carlos Montealegre Gomez
He began the presentation by summarising the clinical characteristics and discussing its pathophysiology, impact on quality of life and current treatments, with emphasis on the use of isotretinoin.
With regard to acne, he highlighted the following points:
With regard to rosacea, he emphasised the following concepts:
He reminded us of some concepts about isotretinoin.
Indications for low-dose isotretinoin in acne:
Indications for low-dose isotretinoin in rosacea:
Conclusion: In both conditions, low doses of isotretinoin have proven to be an effective and safe strategy with fewer side effects than conventional doses. In acne, low doses are well studied and widely used, showing high efficacy even in severe acne when used in combination with corticosteroids. In rosacea, low doses are a promising alternative for refractory cases, although they are considered second-line treatment, and their implementation depends more on clinical experience than on formal guidelines.
Speaker: Dr Jannell Obregon Alzamora
She began by stating that post-inflammatory hyperpigmentation is often the initial concern in acne patients, and is exacerbated by ethnic, geographic and climatic factors.
Her presentation was based on a summary of topical treatment recommendations from the 2024 AAD guidelines and 2021 NICE guidelines.
First-line treatment because of their effectiveness, low cost and ability to improve adherence. They use multiple mechanisms to maximise effectiveness.
Minimum recommended duration: 12 weeks, assessing results after this period
Useful in specific cases, but less effective than combinations.
Clinical response can be found within 6–8 weeks. Informing patients about this time is essential to manage expectations.
Topical retinoids (including tretinoin, adapalene, tazarotene and trifarotene):
Special considerations: Patients with high phototypes: They require greater care due to the propensity for hyperpigmentation and scarring. Use topical combinations and strict photoprotection.
Pregnant women: No risk: Oral acid, BPO, erythromycin, clindamycin, salicylic acid: safe in small areas and for a short time.
Tips to avoid hyperpigmentation due to acne:
Start treatment early and avoid touching lesions.
Use mild cleansers, moisturisers and broad-spectrum sunscreens.
Conclusion: Topical acne treatment should be personalised, taking into account the severity, skin type and preferences of the patient. Fixed combinations and starting with a low dose are key strategies to improve adherence and clinical outcomes. Photoprotection is essential, especially for high phototypes.
Speaker: Dr Minerca Gomez Flores
She reminded us of the approved treatments for rosacea.
Encapsulated benzoyl peroxide (new 5% formulation) approved in 2022.
Evidence on benzoyl peroxide in rosacea:
Although encapsulated benzoyl peroxide is an emerging option with promising results, it is not yet widely adopted in mainstream guidelines. Its use is recommended in selected cases, particularly when other treatments fail to clear lesions, while taking into account its adverse effects.
Speaker: Dr Paulo Jorge Tavares da Silva Lamarão
He recalled by way of introduction:
Speaker: Dr Vicente Manuel Navarro Lopez
He began his presentation with a brief introduction.
He went on to outline his research group’s studies with different strains that could have a beneficial effect on acne.
Probiotics (Lacticaseibacillus rhamnosus CECT 3001) + Spirulina (Arthrospira platensis BEA_IDA 0074B)
Microbiological findings to date according to the various studies published thus far
With regard to rosacea and gut microbiota, based on recent publications, he presented a randomised, double-blind, placebo-controlled clinical trial he is currently conducting with his working group in which Lacticaseibacillus rhamnosus CECT 30579 and Bifidobacterium Longum CECT 30615 are being assessed.
General conclusions on microbiota and skin diseases
Coordinators: Dr Emilia Noemí Cohen Sabban and Dr Jaime Piquero Casals.
Speakers: Dr Emilia Noemí Cohen Sabban, Dr Andrea Santos Muñoz, Dr Adrián Alegre Sánchez, Dr Oscar Jairo Valencia Ocampo, Dr Jaime Piquero Casals, Dr Jose Luis Lopez Estebaranz, Dr Edgar Enrique La-Rotta Higuera, Dr Jaime Alberto Rengifo Palacios.
Speaker: Dr Emilia Noemí Cohen Sabban
Speaker: Dr Jose Luis Lopez Estebaranz
Treatment with oral isotretinoin is considered to be the most effective option for acne treatment, especially in moderate and severe cases. However, there are several issues to consider when using this medicine.
Speaker: Dr Andrea Santos Muñoz
The human microbiome, particularly the skin microbiome, is a complex ecosystem composed of a vast array of microorganisms, including bacteria, fungi, viruses and Archaea. Overall, 30% of the cells in our body are human, while 70% are bacteria, of which there are more than 1,000 species that colonise different areas of the human body.
The microbiome refers to the set of microorganisms, their genes and metabolites that colonise different parts of the human body. This term encompasses not only bacteria, but also fungi, viruses and Archaea. The skin microbiome is therefore a collection of bacterial organisms that inhabit our skin, playing a key role in skin protection, regulation, repair and immune tolerance.
The composition and function of the skin microbiome is influenced by multiple intrinsic and extrinsic factors. Intrinsic factors include genetics, age, gender and disease, while extrinsic factors include environment, hygiene habits and use of cosmetic products. The skin is divided into different areas with their own microbial characteristics: dry, moist and sebaceous areas, each with a bacterial flora adapted to its local conditions.
The microbiome changes throughout life. In newborns, the microbiome is less diverse and unstable, making it more susceptible to disturbances from external factors such as inappropriate use of antibiotics, which can permanently alter bacterial composition. In children and adolescents, the microbiome remains highly dynamic and vulnerable to factors such as environment, diet and interaction with others. In adulthood, the microbiome stabilises and becomes more diverse, contributing to protection against infection. In the elderly, microbial diversity decreases and the microbiological composition of the skin tends to be more homogeneous among individuals.
Microbiome disturbances, especially early in life, can have long-lasting effects and are associated with increased susceptibility to a variety of diseases, including inflammatory skin diseases.
The skin microbiome has multiple functions including protection against pathogenic microorganisms, immune system regulation and repair of the skin barrier. It also plays a crucial role in immune tolerance, helping to maintain the balance between immune responses and preventing exaggerated responses that can lead to inflammatory diseases.
The skin barrier itself is now understood to be a dynamic structure where the microbiome plays a central role. A healthy microbiome, characterised by balanced and stable microbial diversity, is essential for maintaining skin integrity. Any disturbance in this balance can lead to dysbiosis, which in turn predisposes individuals to inflammatory skin diseases.
In the past, acne was associated with increased Cutibacterium acnes proliferation. However, more recent research suggests that it is not simply an increase in the amount of C. acnes, but a decrease in the skin’s bacterial diversity, with proliferation of more pathogenic C. acnes strains (phylotype IA1-IB), which contributes to the onset of inflammatory lesions.
In addition, though normally considered to be an opportunistic pathogen, Staphylococcus epidermidis actually plays a protective role in the skin. These bacteria produce antimicrobial peptides that inhibit the proliferation of pathogenic C. acnes strains and may actually promote the production of interleukin-10, which modulates immune response in acne.
As regards rosacea, research on the microbiome is less advanced, but some studies suggest that Demodex folliculorum, a mite naturally present on the human skin, plays a crucial role in the pathogenesis of rosacea. Interaction between Demodex and other microorganisms, such as Bacillus oleronius, may aggravate rosacea symptoms, especially in patients with increased skin temperature. Although S. epidermidis is protective in acne, in rosacea it can have an adverse effect under certain conditions, exacerbating skin inflammation.
The gut microbiome also affects the skin, especially in inflammatory diseases such as acne and rosacea. A gut microbiome imbalance, with a decrease in beneficial bacteria such as Firmicutes and an increase in Bacteroidetes, can trigger systemic inflammation which, in turn, affects skin health. Dietary factors, such as a diet rich in refined sugars and saturated fats, can disrupt both the gut and skin microbiomes, exacerbating inflammatory skin conditions.
The treatment of dermatological conditions associated with disturbances in the microbiome should focus on restoring a balanced skin microbiome. In this regard, considering the use of oral probiotics, prebiotics and topical postbiotics was recommended to promote microbial diversity and improve skin health. However, there is still little scientific evidence on the effectiveness of these treatments.
In summary, the skin microbiome is an essential component of dermatological health. Maintaining its diversity and balance is key to preventing and treating acne, rosacea and other chronic inflammatory conditions.
Speaker: Dr Adrían Alegre Sánchez
Truncal acne affects a large proportion of acne patients, as more than 50% of patients with facial acne also have lesions on their trunks. Many do not see a doctor for these lesions because they consider them less important, believe they are untreatable or confuse them with other conditions. This type of acne may influence the choice of treatment for facial acne, as the severity of lesions on the trunk is often greater than on the face, requiring a more intensive treatment approach.
Although there are few studies on the impact on the quality of life of patients with truncal acne, these patients, who are mostly adolescents and young adults, have been found to experience a significant impact at certain times of the year, such as in the summer. In a study in nearly 1,000 patients, 92% were found to have facial acne, 61% back lesions and 45% anterior trunk lesions. This shows that the most affected areas in truncal acne are the back, followed by the chest and shoulders. Furthermore, less than 5% of truncal acne cases are confined to this area, suggesting that the condition almost always coexists with facial acne.
Truncal acne tends to be more common in men and its onset is later than facial acne. A relationship has been found with high testosterone levels, which favour the appearance of acne in this area.
A differential diagnosis is crucial, as truncal acne can be confused with fungal folliculitis, acneiform eruptions, miliaria, or even with hidradenitis suppurativa or acne conglobata in some cases.
The aetiopathogenesis of truncal acne is similar to that of facial acne, with impaired follicular keratinisation and an exacerbated immune response (overexpression of TLR4, IL-2 and IL-10, and decreased MMP9). However, unlike facial acne, hyperseborrhoea is not always found, which means that treatment may differ. In addition, patients with truncal acne have a higher predisposition to develop scarring, especially in dark phototypes, and to develop post-inflammatory pigmentation.
The treatment of truncal acne is challenging due to the extent of the lesions and the difficulty in applying topical treatments over large areas. Topical retinoids such as trifarotene are effective, but their use may cause irritation, so intermittent application is recommended. Other topical treatments may include 7.5% dapsone gel or 10–20% azelaic foaming solution.
Oral treatments, such as isotretinoin, are effective, but due to the lesser relationship with sebaceous secretion, their action is slower, requiring higher doses. Tetracyclines are effective for severe inflammation and spironolactone for adult female acne. Finally, adalimumab is useful for acne fulminans or conglobata.
In addition, it is important to address external factors such as hyperhidrosis, which can contribute to acne exacerbation, or the use of protein supplements or testosterone.
As for cosmetic treatments, the doctor recommended using exfoliating products and body sprays with salicylic acid.
Zinc gluconate, at a dose of 30 mg daily for 3 months, has also proven effective in some cases.
Laser treatments can be helpful, especially vascular lasers for inflammation and remodelling devices for scars. In some cases, photoepilation is recommended to prevent and treat scarring in areas where acne is more severe.
Speaker: Dr Oscar Jairo Valencia Ocampo
Acne in adult women has become a growing concern in dermatology, as it has a high prevalence in this cohort, even reaching 15% in menopausal women.
Acne treatment in adult women requires a thorough assessment of various factors influencing the pathogenesis of the disease. Some of the most relevant factors are the use of irritating cosmetics, diet, stress and sleep deprivation. Therefore, an empathetic and holistic approach, including the emotional assessment of the patient, is essential for effective treatment.
Acne in adult women is often related to hyperandrogenism, especially in cases of polycystic ovary syndrome (PCOS). Typical signs include seborrhoea, hirsutism and androgenic alopecia.
It is important to remember that combined oral contraceptives are still a key treatment option in these patients. In addition, spironolactone has been shown to be superior to clindamycin in the treatment of acne in adult women, especially in women with signs of hyperandrogenism. Spironolactone acts as an anti-androgen, blocking the effects of androgens on the sebaceous glands. A total of 80% of patients have been found to respond positively to this treatment. Hyperkalaemia, one of the feared adverse effects of spironolactone, is rare in women under 45 years of age.
It is also frequently associated with metabolic comorbidities, such as insulin resistance, especially in patients with polycystic ovary syndrome. Obesity, accompanied by acanthosis nigricans, is also a common finding. In these cases, insulin sensitisers such as metformin have proven beneficial, especially in women with body mass indexes (BMIs) over 25. In addition, inositol, known for its beneficial effects in the treatment of PCOS, is increasingly being used as a complementary treatment option.
It is essential for dermatologists to recognise that many adult women with acne also have sensitive skin, with impaired ceramide production and decreased mitochondrial function. Skin irritation from retinoid use is a common problem, as up to 50% of women may experience adverse reactions due to skin hypersensitivity. The use of retinoids with lower irritant potential, such as retinaldehyde, and the use of intermittent treatments or low concentrations are recommended to minimise irritation. In addition, skin barrier care with emollients is key to improving tolerance to treatment.
Acne scarring is a common complication, especially in women with dark skin phototypes who are at increased risk of developing hypertrophic scarring and post-inflammatory pigmentation. Scar treatments should be aggressive to prevent the formation of hypertrophic scars, using effective topical therapy, such as those combined with benzoyl peroxide, which has shown good results. In women with dark phototypes, special caution should be exercised to avoid hyperpigmentation, as these patients are more susceptible due to increased skin inflammation.
Acne excoriée is common in women with psychological disorders. Up to 4% of patients have been found to suffer from this disorder. Intervention should be interdisciplinary, involving both dermatological and psychological treatment, as poor adherence to treatment is a major challenge. In these cases, it is essential to treat the underlying cause, such as anxiety or obsessive-compulsive disorder, which often leads to repetitive behaviours.
During pregnancy, acne affects up to 43% of women, and special care is needed in the treatment of these patients. Azelaic acid is a safe and effective option at all stages of pregnancy, as it poses no risk to the foetus. This active substance has anti-inflammatory properties and has been shown to be effective both in the treatment of acne and pigmentation disorders, such as melasma. In addition, azelaic acid is useful as long-term treatment in women with acne who do not respond to other conventional treatments.
Both topical and oral probiotics have been mentioned in some studies as a complementary therapeutic option for the treatment of acne. Although the efficacy of probiotics in acne has not yet been proven, it has been suggested that they may have a synergistic effect with oral antibiotics. Zinc gluconate has also been shown to be useful due to its anti-inflammatory properties and has been used successfully in the treatment of acne. A daily dose of 30 mg elemental zinc is recommended to reduce acne-related inflammation.
Holistic acne treatment should be the approach in adult women, considering hormonal as well as emotional and environmental factors. Finally, treatments should be tailored to the individual needs of each patient, with a focus on improving quality of life and adherence to treatment.
Speaker: Dr Jaime Piquero Casals.
The concept of “cosmeceutical” refers to products that offer both cosmetic and medicinal benefits.
The doctor’s main message was that cosmetics and medicinal products are not enemies.
Via their synergistic action, cosmeceuticals can improve treatment results and reduce side effects such as dryness or irritation.
The use of cosmeceuticals also improves adherence to medical treatment. These products can complement medicinal products and also act as a bridge between treatment phases to prevent rebound acne or reduce the adverse effects of more aggressive treatments, such as isotretinoin.
Examples of cosmeceuticals:
Cosmeceutical “all-rounder” acne, melasma, photoageing:
Glycolic acid (alpha hydroxy acid, small molecule that penetrates the skin very easily)
Other cosmeceuticals useful in acne are:
He also gave examples of formulations with synergistic cosmeceuticals for use on oily, acne-prone skin:
Retinoids (retinol and retinaldehyde) are used because they promote keratinocyte differentiation, normalise disordered keratinisation in sebaceous follicles, help to control lipid synthesis, strengthen barrier function, have a tone-unifying action and reduce inflammation.
Photoprotection is also fundamental in the treatment of skin conditions. The importance of sunscreens was emphasised, as they not only protect against UV radiation, but can also have anti-inflammatory and soothing effects, which are crucial in patients with conditions such as acne and rosacea. In rosacea, some sun creams contain anti-inflammatory active substances that improve skin appearance without causing irritation, which is especially useful in patients who want to avoid wearing make-up.
He named niacinamide, azelaic acid and glycine, among others, as cosmeceuticals used in rosacea.
Finally, the central message was that cosmeceuticals should be considered to be a comprehensive tool in dermatological practice. It is important for dermatologists to inform themselves about the properties of these products in order to appropriately include them in treatments, improving the quality of life of patients.
Speaker: Dr Jaime Alberto Rengifo Palacios
He described the pathophysiology and possible treatments for rosacea elucidated thus far, arguing that rosacea is a complex condition. He affirmed that its treatment is still a challenge, despite over 100 years of knowledge.
Some key points:
One of the key factors is the microbiota, particularly the density of Demodex spp. which can trigger an inflammatory cascade. This process is amplified by some bacteria, such as Bacillus oleronius, which increase inflammation. In this context, TLRs and calcium channels are key in the activation of inflammatory and vascular responses.
Another relevant finding is LL-37, a peptide involved in inflammation as well as angiogenesis, which also contributes to the pathogenesis of rosacea.
Neurovascular mechanisms are key in rosacea. Burning sensations and transient receptor potential (TRP) receptor activation are mediated by factors such as capsaicin and other calcium channels, leading to vasodilation which is reflected in symptoms.
Several approaches are involved in the treatment of rosacea.
In the innate immunity area, medicinal products such as isotretinoin and tetracyclines stand out. In addition, the use of ivermectin and metronidazole shows good results as anti-inflammatory agents. Topical treatment may include protease inhibitors, which are under investigation, and medicinal products such as oxymetazoline for vasodilation.
Promising treatments are being developed.
In the long term, patient awareness of the importance of avoiding triggers is crucial. Dietary habits, such as avoiding seasoned and processed foods, are still recommended.
In terms of prognosis, treatment response depends largely on the underlying factors in each patient, making rosacea treatment complex but not impossible. The key is to personalise treatments according to aetiology and the patient’s specific characteristics, highlighting the importance of a holistic and well-informed approach to the management of this condition.
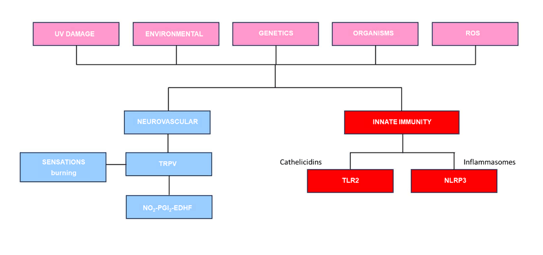
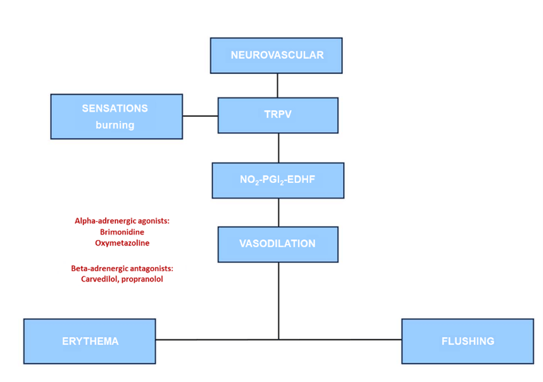
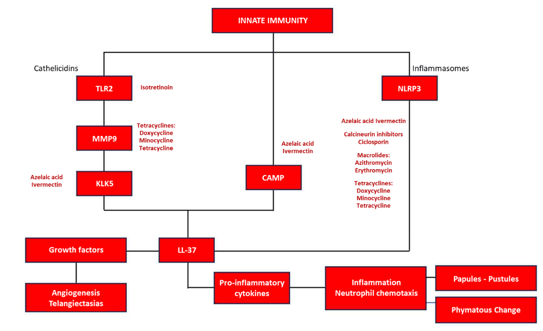
Below are the ORIGINAL charts the doctor presented in his lecture, which summarise both pathogenesis and the proposed treatment.
Geng, R. S. Q., Bourkas, A. N., Mufti, A., & Sibbald, R. G. (2024). Rosacea: Pathogenesis and Therapeutic Correlates. *Journal of Cutaneous Medicine and Surgery, 28(2), 178-189. https://doi.org/10.1177/12034754241229365.
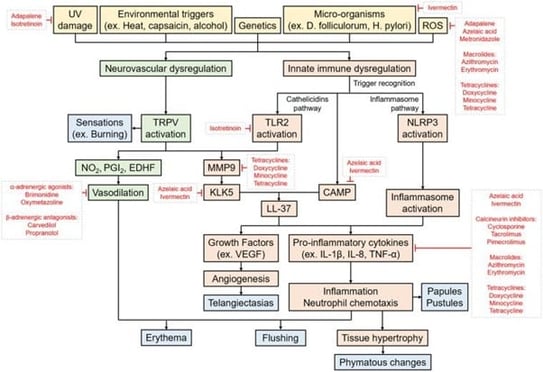
Schema of the risk factors, triggers, and pathogenesis pathways of rosacea. The pathogenesis of rosacea likely involves a complex interplay between several factors and pathways, including neurovascular dysregulation and innate immune system dysregulation involving cathelicidins and inflammasomes. These processes then give rise to the symptoms and clinical features of rosacea, depicted in blue. Known targets of medications currently used in treating rosacea are indicated.

(A) Proposed cathelicidins pathway believed to be implicated in the pathogenesis of rosacea. Production of LL-37 leads to several physiological effects including angiogenesis, vasodilation, inflammation, and matrix degradation. (i) High densities of Demodex folliculorum upregulates the expression of TLR2 in sebocytes. Enhanced TLR2 activity leads to increased KLK5 activity and production of LL-37. (ii) CagA+ and VacA+ Helicobacter pylori strains stimulate mast cell activation and subsequent increase in histamines and prostaglandins, promoting inflammation. (iii) Through MMP2 upregulation and TLR2 signalling, ROS promote matrix degeneration and increase LL-37 production. promote matrix degeneration and increase LL-37 production. (iv) UV promotes expression of CAMP in keratinocytes via vitamin D-dependent and ER stress-induced pathways. CAMP can then be cleaved into the bioactive LL-37 fragments.
(B) Proposed inflammasome pathway believed to be implicated in the pathogenesis of rosacea. Inflammasome activation results in several physiological effects including chemotaxis of neutrophils, angiogenesis, and inflammation. The cathelicidins and inflammasome pathways are intricately linked. TLR2, toll-like receptor 2; KLK5, kallikrein-5; CagA+, cytotoxin-associated gene A positive; VacA+, vacuolating cytotoxin A positive; MMP2, matrix metalloprotease 2; ROS, reactive oxygen species; UV, ultraviolet; CAMP, cathelicidin antimicrobial peptide; ER, endoplasmic reticulum.
Coordinators: Dr Cesar Fernando Gonzalez Ardila and Dr Maria Ivonne Arellano Mendoza
Speakers: Dr Jose Luis Lopez Estebaranz, Dr Thierry Passeron, Dr Lourdes Rita Bárbara Vazquez, Dr Ana Cláudia Espósito, Dr Maria Ivonne Arellano Mendoza and Dr Katherine Perez.
Speaker: Dr Jose Luis Lopez Estebaranz
He began his lecture by showing iconographies of patients with vitiligo and several differential diagnoses. He then highlighted that patients with vitiligo may have autoimmune comorbidities such as thyroid disease and rheumatoid arthritis, among others, as well as psychological comorbidities, such as anxiety and depression.
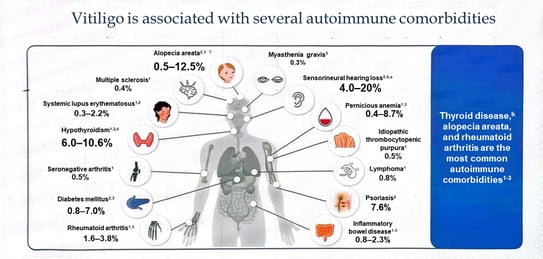
The association with thyroid disorders and neurosensory disorders such as hearing disorders is noteworthy.
He also reviewed the classification into segmental and non-segmental vitiligo, the latter being the most common. He highlighted some clinical variants such as follicular, inflammatory, hypomelanotic and trichrome vitiligo as well as vitiligo ponctué; or special locations such as genitalia and mucosa.
He also reminded us that 50% of all vitiligo cases begin before the age of 20, and that early treatment is important.
He also highlighted the importance of using Wood’s lamp to assess the extent of vitiligo and identify lesions that may not be visible under normal light.
He also mentioned the signs of active vitiligo such as confetti-like lesions, Koebner’s sign or the trichrome sign which indicate that the disease is active and requires urgent treatment to prevent progression.
For the rest of his presentation, he showed clinical images and some differential diagnoses for them.
In conclusion: Vitiligo is a complex condition with varied clinical presentations and associated comorbidities. Early diagnosis and treatment are essential in order not to miss the therapeutic window of opportunity.
Speaker: Dr Thierry Passeron
He began his presentation by outlining three objectives in vitiligo treatment:
Before starting treatment, it is essential to determine whether vitiligo is active (Koebner, confetti-like depigmentation, hypochromic borders) and, if detected, treatment should be urgently initiated and the combination of NB-UVB with oral mini-pulse steroids (e.g. methylprednisolone) is recommended.
Then, to induce pigmentation, it has been shown that the best strategy is the combination of NB-UVB phototherapy or sun exposure with topical treatments, such as topical calcineurin inhibitors or high-potency corticosteroids.
As a prophylactic strategy for relapse he recommended:
New therapeutic agents:
Other approaches:
Speaker: Dr Almudena Nuño Gonzalez
Hyperpigmentation, like melasma and lentigines, arises from a complex interaction of factors, including sun exposure, genetics and hormonal influences. A key factor is oxidative stress, which leads to increased pigment deposition. This occurs because of an imbalance between the production of free radicals (from mitochondrial respiration and external agents) and the body’s antioxidant defences (enzymes such as superoxide dismutase and catalase, and non-enzymatic antioxidants such as glutathione and vitamins C and E). Oxidative stress activates tyrosinase, increasing pigmentation. In addition, DNA damage and advanced glycation end products (AGEs) also contribute to melanogenesis and pigment accumulation.
Although topical antioxidants are commonly used, there are multiple studies with mixed results for oral antioxidants and supraphysiological doses may disrupt the redox balance and promote pro-oxidative states.
She summarised the antioxidants that can be found in foods, including polyphenols; carotenoids; vitamins C, D and E; melatonin; and Polypodium leucotomos.
Polyphenols, which act as ROS scavengers, act synergistically with other antioxidant vitamins. They are mainly present in red fruits, chocolate, cocoa and wine. Studies show that extracts such as maritime pine bark and ellagic acid (in pomegranates and berries) can reduce pigmentation and are useful in the treatment of melasma and solar lentigines.
Carotenoids such as lutein (in green vegetables) and zeaxanthin (in yellow-orange vegetables) have antioxidant properties and are high-energy light filters. They are present in spinach, kale and peppers, among others.
Vitamins C and E are potent antioxidants found in a variety of food sources.
With regard to vitamin D, she suggested supplementation in the event of deficiency.
She mentioned glutathione as the main cellular antioxidant that also inhibits melanin synthesis. It is a copper chelator that disrupts tyrosine activity, interferes with tyrosinase transfer to premelanosomes and increases cysteine levels, which promote pheomelanin synthesis at the expense of eumelanin. It is not only obtained from several foods, but can also be synthesised through exercise, sleep or physical activity. According to clinical trials, the appropriate dose would be 500 mg/day.
Melatonin (a serotonin derivative), a potent antioxidant, regulates circadian rhythm and may improve pigmentation. It can be used topically or orally, although the latter has poor bioavailability and should therefore be used in high doses and at night.
Finally, AGEs can induce melanogenesis and lead to increased oxidative stress. To reduce AGE production, it is important to avoid fried foods, refined carbohydrates and red meat and to opt for vegetables, fruit and cooking methods such as steaming.
Polypodium leucotomos is highly anti-inflammatory and is used in patients with both melasma and vitiligo.
The gut microbiota also plays an important role, with multiple studies analysing the microbiota of patients with and without melasma. Collinsella spp. were found to be abundant in patients with melasma and they are thought to play an important role in impairing oestrogen metabolism, although further studies are needed.
Ultimately, a holistic approach that focuses on healthy diet, exercise, adequate sleep and stress management is most effective. Supplements can play a complementary role, but should not replace lifestyle changes.
Speaker: Dr Ana Claudia Esposito
The treatment of melasma is based on four pillars: photoprotection, systemic treatment, procedures and topical treatment. Although the standard combination is sunscreen plus triple formula, not all patients tolerate the latter due to possible adverse effects, such as ochronosis. Therefore, new evidence-based molecules and treatments have been explored.
Topical metformin:
30% metformin reduces the transcription of melanogenic proteins, such as tyrosinase. In studies, it has been shown to be as effective as the triple formula after eight weeks of use, with good tolerance and promising results.
Melasyl
Melasyl is a melanogenesis inhibitor that acts on precursors such as DOPA, DHICA and DHI, but does not inhibit tyrosinase. MelaB3 combines Melasyl with 10% niacinamide. In studies, its efficacy is comparable to 4% hydroquinone after 80 days, with the advantage of being a cosmetic rather than a medicinal product.
Thiamidol:
A resorcinol derivative, it is a human tyrosinase inhibitor with no cytotoxic effects. When applied 4 times a day, it is as effective as 4% hydroquinone. A new formulation combines thiamidol with (0.1%) retinoic acid and (0.1%) dexamethasone acetate, showing similar results to the traditional triple formulation.
Methimazole:
This antithyroid agent inhibits peroxidase and tyrosinase, with no systemic effects. In studies, 5% methimazole was more effective than 2% hydroquinone, but less effective than 4% hydroquinone.
New products in Brazil:
A combination of hexapeptides, lactoferrin, phosphatidylserine and tranexamic acid showed marked improvement after 12 weeks in comparative studies with 4% hydroquinone.
In conclusion, with an increasing range of options, it is essential to select treatment based on evidence in order to prescribe effective and safe options.
Speaker: Dr Maria Ivonne Arellano Mendoza.
To start her presentation, the doctor reminded us of the concept of the exposome, all those factors to which an individual is exposed and which determine their state of health or disease, such as pollution, tobacco, temperature, nutrition, stress, quality of sleep and solar radiation.
There are multiple molecular mechanisms of photodamage. Some of them include the generation of free radicals (ROS and RNS), generation of harmful metabolites involved in immunosuppression through their effects on Langerhans cells and mast cells (trans-UCA photoisomerisation and photodecomposition), inflammation mediated by nitric oxide and prostaglandins, and both nuclear and mitochondrial DNA disturbances.
Of these, inflammation, abnormal mast cell degranulation and melanogenesis disturbances are the main factors involved in melasma.
She also mentioned opsins, melanocyte membrane proteins, which are sensitive to blue light and capable of inducing melanogenesis.
In order to prevent the onset and recurrence of melasma and other pigmentation disorders, she recommended the use of a broad-spectrum photoprotector with dyes such as iron oxide and that contains antioxidants. Some marketed formulations have different active substances (depigmenting agents or photolyase) that increase their effectiveness.
She reminded us of the main ingredients of topical sunscreens:
She emphasised that there are multiple pigmentation disorders and summarised them in the following algorithm, bearing in mind that each disorder has its own indication for photoprotection and that the photoprotector must be adapted to each patient in order to achieve the best possible adherence.
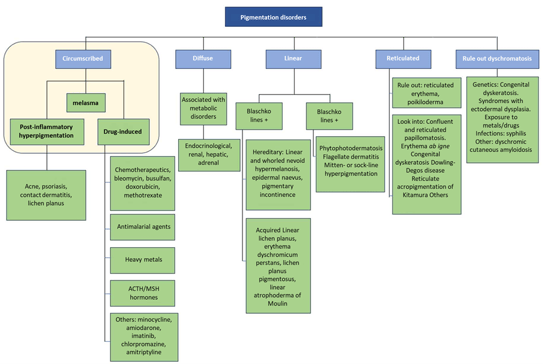
Speaker: Dr Katherine Perez
There are several challenges in melasma treatment in Latin America due to its complex pathophysiology, which involves overactive melanocytes, keratinocytes, fibroblasts, mast cells, endothelial cells and sebocytes, all contributing to inflammation and pigmentation.
She recommended an accurate diagnosis prior to treatment.
She suggested a melasma protocol in which lasers are a therapeutic tool that should be accompanied by other measures:
For melasma with a high pigmentary component, Q-switched laser/Pico laser (4 sessions at 21-day intervals) is preferable.
She also recommended some topical products as a complement to laser treatment, and stressed that she generally does not like to use hydroquinone or corticosteroids. She thus recommended:
She continued her presentation by recommending different lasers for different pigmentation disorders, saying they should always be accompanied by home treatment and photoprotection:
In conclusion: successful melasma treatment depends on an accurate diagnosis, proper selection of tools such as lasers and an individualised approach to avoid adverse effects. The reduction of the vascular component is key in melasma with these characteristics, achieving satisfactory and safe aesthetic patient results.
Speakers: Dr Jose Luis Lopez Estebaranz and Dr Omar Lupi Da Rosa Santos
The first scientific document on photoprotection written by Latin American dermatologists addressing the Latin American population with its specificities was presented. The aim was to share it with dermatologists, doctors from other specialities, other healthcare professionals, and governmental and educational organisations.
A total of 27 dermatologists from 13 countries (9 authors and 18 co-authors) contributed to the consensus.
The modified DELPHI methodology was used. Proposals with less than 80% agreement were rewritten and a new round of questionnaires was carried out until all obtained agreement of 80% or more from experts.
Main messages:
Coordinators: Dr Manuel Del Solar, Dr Sofía López Cordero, Dr Elda Giansante.
Speakers: Dr Ricardo Perez Alfonzo, Dr Juan Carlos Diez De Medina Duran, Dr Sofía López Cordero, Dr Enrique Uraga Pazmiño, Dr Emilia Noemi Cohen Sabban
Speaker: Dr Enrique Uraga Pazmiño
Colchicine is an anti-inflammatory and antimitotic medicinal product that has been used for decades to treat various diseases, such as gout, familial Mediterranean fever and pericarditis. In recent years, its use has expanded to skin diseases and other conditions such as psoriasis and some types of vasculitis.
In terms of absorption, it is administered orally and has a bioavailability of 45%, reaching its peak concentration 2–4 hours after ingestion. Its anti-inflammatory effect is most evident 24–48 hours after administration.
Its mechanism of action has been shown to inhibit microtubule polymerisation by binding to tubulin, so colchicine is effective as an antimitotic. It also disrupts neutrophil L-selectin expression and E-selectin distribution, resulting in an anti-inflammatory effect. It is also antifibrotic and immunosuppressive.
Although the list of dermatological conditions for which colchicine is indicated is extensive, only three have level 1 evidence: palmoplantar pustulosis, recurrent aphthous ulcers and actinic keratoses, the latter in topical form.
It is usually administered at doses of 0.5 to 2 mg, the optimal dose being 1 mg per day in most cases. It is available in topical form (creams and ointments) and, in more severe cases, can be administered intravenously, although the latter option carries higher risks of systemic toxicity.
It has drug-drug interactions with a number of medicinal products, including antibiotics (clarithromycin and erythromycin), antifungals, immunosuppressants and statins, which may increase its concentration and cause serious adverse effects. Moreover, its use should be avoided in renal and/or hepatic dysfunction.
Common side effects include diarrhoea, nausea and vomiting. In rare cases, it may cause liver toxicity or alopecia. Cases of colchicine overdose can cause severe symptoms, including multi-organ failure and death.
Contraindications: - hypersensitivity
- pregnancy
- renal or hepatic failure
- gastrointestinal disorders
- cardiac disorders
- haematological disorders such as blood dyscrasias
- 14 days post use of cytochrome P450 inhibitors and/or P-glycoprotein
The following are case reports in which colchicine was indicated as a treatment with favourable results: generalised granuloma annulare, facial granuloma annulare, generalised pustular psoriasis in combination with biologic therapy, chronic spontaneous urticaria refractory to other treatments, erythema nodosum, lichen planus pigmentosus, AGEP and acne fulminans. In summary, colchicine is an effective medicinal product for various inflammatory conditions, but its use must be carefully monitored due to the risks of side effects and toxicity.
Speaker: Dr Ricardo Perez Alfonzo.
Antimalarial agents (chloroquine, hydroxychloroquine and quinacrine) have immunomodulatory, anti-inflammatory, antiproliferative, photoprotective, antithrombotic, lipid-lowering and hypoglycaemic effects, without causing significant immunosuppression.
Indications: treatment and prophylaxis of malaria and several autoimmune diseases
Antimalarial agents may be indicated for many dermatological pathologies: porphyria cutanea tarda, dermatomyositis, sarcoidosis, generalised granuloma annulare, foreign body granuloma and even rosacea.
Hydroxychloroquine has a delayed therapeutic effect, possibly requiring a month to show results. It accumulates in melanin-containing tissues, such as the skin and retina, and is excreted in the urine. Although it crosses the placenta and is excreted in milk, its teratogenic risk is low.
It is effective on specific CCLE, ACLE, SCLE and LET lesions; improves systemic manifestations of SLE; and acts on non-specific lesions (oral ulcers, photosensitivity and calcinosis).
He explained that there is a latency period for the onset of action so he specified that he starts systemic corticosteroids and antimalarial agents, and then after one month discontinues corticosteroids, progressively reducing them.
He strongly suggested following the indications in the table below.
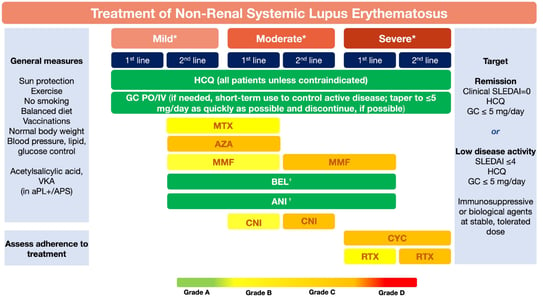
He highlighted some points:
The dose should be titrated according to the patient’s weight and liver or kidney function. Administration requires regular ophthalmological monitoring as, although ocular effects are rare, they may include irreversible retinopathy if the medicinal product is used for more than 5 years or at high doses. Recommend that patients wear dark glasses and stop smoking.
It is also important to request G6PD testing prior to administration to avoid haematological toxicity. Other common adverse effects include nausea, vomiting, diarrhoea and skin pigmentation, although these are usually reversible. It is important not to stop treatment without medical supervision, as stopping treatment increases the risk of disease recurrence.
Contraindications include retinopathy, renal or hepatic failure, glucose-6-phosphate dehydrogenase deficiency and some psychiatric diseases. Although it crosses the placental barrier, its use in pregnancy is not contraindicated, as it has not been associated with congenital malformations.
Speaker: Dr Emilia Noemi Cohen Sabban
Doxycycline is a semi-synthetic antibiotic derived from adritetracyclines. It is broad-spectrum, and is effective against gram-positive, gram-negative and intracellular bacteria such as Chlamydia and Mycoplasma. It is currently used in the treatment of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) infections.
Pharmacological characteristics
Mechanisms of action and resistance
Clinical indications
Adverse effects
Absolute contraindications: use in children <8 years, pregnancy/lactation
Conclusion: Doxycycline is a versatile medicinal product with broad indications in dermatology, most notably in the treatment of acne, rosacea and some STDs. However, its use must be rational to minimise bacterial resistance and adverse effects.
Speaker: Dr Juan Carlos Diez de Medina
N-acetyl cysteine (NAC) is considered to be one of the best antioxidant medicinal products, has been used since 1960 and was approved by the FDA as an expectorant. Despite prolonged use, there are no significant reports of poisoning, and side effects are minimal. The drug, which acts as a precursor of L-cysteine and promotes glutathione production, has a positive impact on the central nervous system, especially on dopamine regulation. This makes it useful in anxiety, depression, schizophrenia and bipolar disorders.
In dermatology, NAC is primarily used as an adjuvant in the treatment of various skin pathologies, including trichotillomania, psychogenic excoriations and acne. Although studies are limited, anecdotal evidence suggests that NAC has positive effects, especially in conditions associated with anxiety. Treatment is generally administered in 600 mg doses every 12 hours in adults, and 300–600 mg in children, depending on age (it can be used from the age of 2).
He presented cases in which significant improvements were observed in patients with skin lesions induced by compulsive behaviour. For example, one patient with psychogenic excoriations experienced a marked reduction in anxiety symptoms and lesions after 45 days of treatment. Other cases of dermal lesions in anxious patients also considerably improved with the use of NAC.
Although clinical studies are still insufficient, NAC appears to be a safe and effective therapeutic option in the treatment of dermatological disorders related to anxiety and compulsive behaviours in both adults and children. Further research into its use is recommended, but thus far its safety profile is remarkably favourable.
Conclusion: NAC is a safe and promising medicinal product in dermatology, with positive results in the treatment of various anxiety-related conditions, although more studies are needed to confirm its efficacy on a large scale.
Speaker: Dr Sofía Cordero
This lecture focused on the use of low-dose methotrexate as a therapeutic alternative in autoimmune and inflammatory diseases, highlighting its applicability in a context where patients do not always have access to modern biologic treatments.
Mechanism of action and properties: Low-dose methotrexate acts as an immunomodulator, inhibiting adenosine degradation and blocking certain enzymes. This increases anti-inflammatory mediators, such as interleukin-10, and decreases pro-inflammatory ones, such as TNF-alpha.
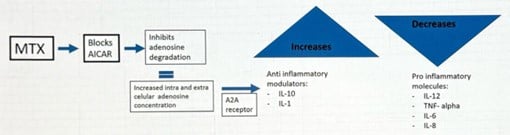

BIODERMA Congress Reports CILAD 2022



EADV 2024 Bioderma Congress Reports