0 professionals
Psoriasis From Gene to Clinic 2024 Bioderma Congress Reports
Psoriasis From Gene to Clinic 2024 Bioderma Congress Reports
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Report written by Dr. Sophia Paget (Dermatologist, United Kingdom)
Related topics
The opening day of the Psoriasis Gene to Clinic conference 2024 truly lived up to its name, blending groundbreaking lab-based research with practical clinical insights. This dynamic combination sparked as many new questions as it answered.
Several key themes emerged throughout today's presentations.
An exciting topic was potential biomarkers to help us to identify super responders and those likely to progress to more severe forms of psoriasis for whom early intervention with highly effective immunomodulatory treatments may improve overall outcomes and potentially lead to disease modification and long-term remission.
There was exploration of differences in genetic expression of immune pathways in psoriasis types and how this information may help to guide treatment choice
A proposed redefinition of the classification of psoriasis severity was presented, which incorporates factors important to patients. Data outcomes were shared indicating that ignoring these factors results in dermatologists under treating psoriasis. As part of this there was a push for future trials to include particularly high impact site psoriasis (such as genital, scalp and nail psoriasis) irrespective of PASI or body surface area.
Novel potential pathways of treatment were presented such as mesenchymal stromal cells for extremely treatment resistant severe plaque psoriasis. Further potential treatments were explored using evidence from other specialties particularly rheumatology who shared experience with CAR – T cell treatment in autoimmune conditions. Whilst experience from the world of ankylosing spondylitis unveiled the effective use of specific clonal TCR targeting treatments to deplete disease specific CD8 cells. Both experiences raised the question whether these treatments may present new options for highly treatment resistant forms of psoriasis in the future.
Let’s explore some of these themes in more detail.
Speaker: Dr. Khusru Asadullah
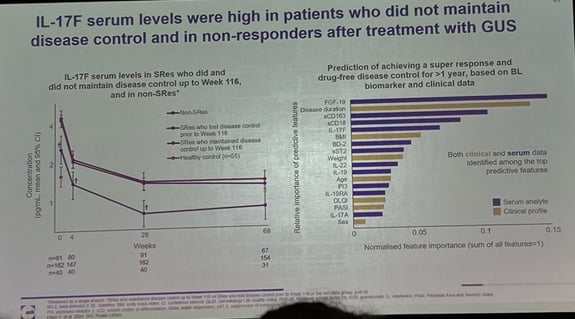
Dr. Khusru Asadullah, Berlin Germany, presented data from the phase 3a GUIDE trial. This looks at psoriasis patients with short duration disease (</=2 years) and long duration disease (>2years) treated with guselkumab. They defined a super-responder as those who had a PASI 0 at week 20 and week 28. Even after stopping treatment, there was sustained control of disease. So how can these super responders be identified? The authors discovered that the super responder group had elevated IL 10 producing T cell population at baseline, which was sustained throughout treatment. Could this be a potential biomarker? We will wait and see. Discussion points from this presentation also uncovered that ultra short disease duration patients (<=15 months) had even greater response supporting the hypothesis of early intervention leading to disease modification and improved outcomes.
Speaker: Dr. Jake Saklatvala
Dr. Jake Saklatvala, London UK, presented work looking at Polygenic risk score PRS identified from 4 bio banks across Europe with blood samples from psoriasis patients. The problem presented is that we currently only treat the severe psoriasis group, but if a PRS could be identified correlating with the severe psoriasis phenotype, perhaps this might help spotlight which patients would progress to severe disease, enabling early intervention where needed. The PRS found had similar bearing to obesity and smoking as risk factors for severe disease and the authors propose that in combination with other known risk factors PRS may provide support to a scoring system to help highlight severe psoriasis cases early in their disease course.
Speaker: Pr. Nick Reynolds
Professor Nick Reynolds, Newcastle UK, presented on behalf of the PSORT – D team who used transcriptomic profiling from skin biopsies of psoriasis patients receiving Biologics and with the help of machine learning tools such as Weighted gene correlation network analysis (wgcna) they have uncovered molecular endotypes of psoriasis phenotypes and signatures of disease severity. This outlined 20 genes associated with psoriasis disease severity. Quite amazingly, using this technique they were able to predict overall PASI score from the molecular endotypes identified from a singular skin biopsy of a psoriasis patient. The next step would be to identify which of these genes is the most relevant and how could this be translated into clinical practice?
Speaker: Pr. Michel Gillet
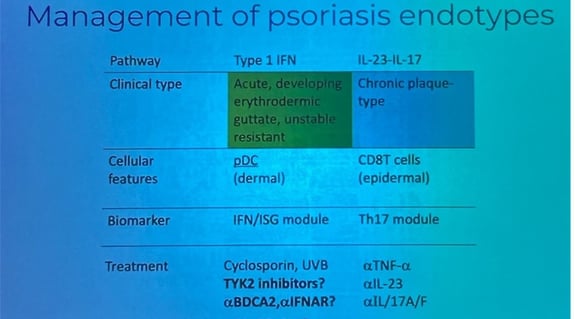
There are varied patterns of genetic expression of immune pathways in different forms of psoriasis. Professor Michel Gillet’s keynote lecture presented a summary of the psoriasis transcriptome and how certain molecular endotypes convey treatment resistance. It seems that Il17 and IL23 resistant psoriasis have a shift towards higher production of IFN1
In the context of other inflammatory skin diseases, it is well established that certain immune pathways predominate for example in Lichen planus the Th1 pathway reigns and the disease pathway can be blocked with JAK1/2 inhibition. Similarly in lupus IFN alpha/beta blockade can be effective. In all forms of psoriasis all there is gene activation related in some way to the IL17 pathway.
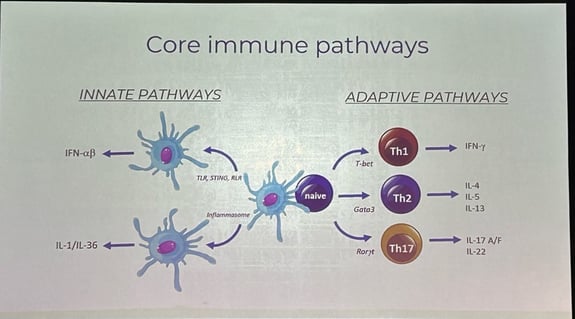
Examining the psoriasis transcriptome can be helpful when there is phenotypic overlap such as psoriatic dermatitis. Gene modelling can be used to see whether Th17 or Th2 gene expression predominate to tailor treatment appropriately. An example of this provided was a case of atopic dermatitis were at baseline genetic modelling outlined predominant Th2 expression. This patient proved to be a non-responder to dupilumab. Gene modelling was repeated which this time demonstrated predominant Th1 gene expression. The patient was switched to a JAK inhibitor and treatment response was observed.
Professor Gillet described 3 immune models in psoriasis:
IFN1comes from all cells but is produced by plasmacytoid dendritic cells (pDCs) more than any other cell type. Early expression of IFN 1 is seen in early psoriatic plaques before Th17 in later more established lesions. Antimicrobial peptides eg LL37 trigger IFN1 production. This occurs when LL37 binds with DNA and enables it to be stabilised, enter and activate pDCs inducing IFN1 production. C1qBP binds LL37-DNA membrane expression by pDCs and C1q, produced most by macrophages, inhibits this binding. Could new treatments targeting these be used to treat IFN1 predominant psoriasis?
Speaker: Pr. Bruce Strober
Professor Bruce Strober delivered a compelling summary of the case to redefine severe psoriasis. He made the case for abandoning the terms mild, moderate and severe due to these terms resulting in rigid thresholds used to define when therapies can be used which unfortunately results in the under treatment of forms of psoriasis which impact quality of life severely but may not involve wide body surface area. He presented the IPC severity reclassification statement which prioritises the following when considering whether psoriasis is severe:
Professor Strober referenced, numerous supportive trials, including the UPLIFT study which looked at over 3800 pts with PSO and or PSA. Of these patients 60% with less than or equal to 3% BSA self-labelled their psoriasis as severe. He noted that this data suggests dermatologists are tending towards under treating disease from a patient perspective.
Professor Strober particularly delved into the patient burden of living with psoriasis affecting high impact areas. He presented evidence showing a history of high impact disease impacts patients more negatively in many areas eg fatigue, itch etc. Clinical Trials conventionally exclude PASI<10 and ¾ of patients categorised as moderate to severe on IPC definition would not qualify for phase 3 trial of drugs. However, there has been a move from industry to include patients with high impact site involvement (IXORA-Q ixekizumab for genital psoriasis, DISCREET apremilast for genital psoriasis, SCALP secukinumab and Psoriatyk scalp deucravacitinib). Results from these placebo control trials indicate promising disease control with biologics for this group of psoriasis patients with notably no increase in adverse events compared with high PASI score patients.
The main takeaway was adhering to BSA and PASI alone leads to under treatment of severe psoriasis.
Speaker: Dr. Su Mar Lwin
Dr. Su Mar Lwin, London England, presented 3 case studies of severely treatment resistant psoriasis in whom mesenchymal stromal cells have been used.
The basis for using MSC treatment stemmed back to observational case reports where bone marrow transplants (BMT) were performed for other reasons in psoriasis patients and psoriasis was cured as a secondary effect. MSCs are multipotent stem cells with low immunogenicity, so there is no need for preconditioning therapy like for CAR-T or BMT. MSCs Down regulate inflammatory pathways.
Dr. Lwin presented 3 females each with a more than 25-year history of psoriasis, all of whom had failed at least 5 Biologics. Umbilical cord MSC were administered in slow boluses (to avoid pulmonary accumulation overload risks). Adjuvant etancercept was continued for 1 case and MSCs were administered alone for the other 2 cases. The treatment was well tolerated by all 3 candidates with no severe adverse events reported.
Results were as follows:
From a cytokine perspective patients 1&3 were more IL17 dominant; patient 2 was more IFN1 dominant. Promising initial results from a novel therapeutic strategy for highly treatment resistant psoriasis.
Speaker: Pr. Matt Brown
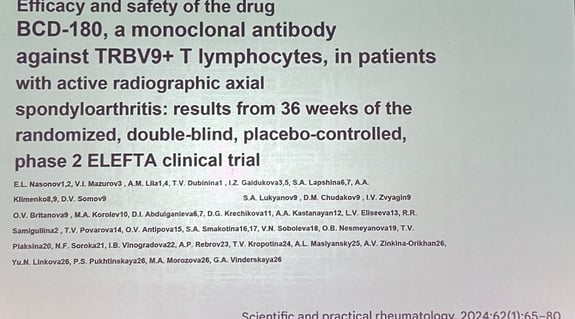
Professor Matt Brown, London, UK, shared experience from rheumatology using highly targeted monoclonal antibodies to target specific TCR subsets of CD8 cells in patients with ankylosing spondylitis (AS). Nearly all HLA – B 27 positive cases of AS and no healthy HLA – B 27 positive nor negative controls have CD8 lymphocytes with a very similar group of TCRs which are T effector memory cells. Monoclonal antibodies used to deplete these CD8 lymphocytes are effective at treating ankylosing spondylitis. Could something similar be targeted for psoriasis?
Professor Brown explained the ERAP1 association with HLA-cw6 seen in psoriasis gene to gene interaction. ERAPs help make peptides just the right length for presentation on HLA molecules. ERAP1 cuts to 9amino acids; ERAP 2 degrades into smaller parts.
Every human has around a billion different T cells, TCR rearrangement options are 1011.
He shared a case example of resistant AS, where Biologics and even autologous stem cell transplant had been ineffective. Monoclonal antibody directed Trbv9 T cell depletion however, worked very well.
He shared a paper from a Russian randomised controlled trial using monoclonal antibody targeting trbv9 T cells, which showed this treatment to be as effective as Biologics. Adverse events with this included high rates of acute infusion fevers, however and high dose prednisolone was required for managing this, although there was no increased infection rates in this group.
Speaker: Pr. Georg Schett
The Keynote lecture from Professor Georg Schett, Erlangen, Germany, provided an overview of the use of CAR-T cells in a myriad of autoimmune rheumatology diseases including severe lupus, dermatomyositis, granulomatous polyangitis and systemic scleroderma. He pointed out the move towards cytokinine focused rather than organ focused disease definitions, and treatments aiming to treat the source of the disease rather than control the effects of the immune response. Ultimately moving the aim from disease suppression to disease remission and possibly even cure.
Schett explain the benefits of CAR – T cell treatment for autoimmune disease diseases including the following:
Using the example of systemic lupus erythematosis (SLE) Schett outlined how although this is an antibody mediated disease unfortunately ritlicitinib, the anti-20 B cell depleting agent, is not effective in controlling disease. Why is this? Although circulating be cells are depleted B cells residing in lymphoid tissues such as the tonsils are protected these are enough to continue perpetuating the disease. In contrast CAR – T cell therapy results in more effective B cell depletion including in the central nervous system which is a benefit for diseases such as SLE.
CD–19 CAR – T cell therapy will eliminate circulating plasma cells but not bone marrow plasma cells. This results in excellent disease control without eliminating old memory such as vaccination history.
It appears that this form of treatment results in a deep immune reset. Schett commented that it seems likely T cells are also probably contributing to the remission being sustained.
Could this be an area for therapeutic methods for severe treatment resistant psoriasis? Questions raised pointed out the need for T cell targeted CAR – T cell treatment to be very cell specific to deplete the correct populations for psoriasis disease control without resulting in severe immunocompromise. Schett also shared that where disease course has been long and resulted in extensive tissue damage he would avoid CAR – T cell treatment in practice as unlikely to be effective.
In vitro CD123 CAR-T cells were presented by Eloise Bôle-Richard as a potential therapy for psoriasis and in vivo studies are planned.
Today’s themes were even more diverse and spanned the gap from bench to bedside in every session. The day began with an exploration of two highly relevant clinical targets for treating psoriasis: IL 17 and IL 23 and how this axis is involved in psoriasis pathogenesis. Later there was data presented around IL 23 inhibition and its effect on non-pustular palmoplantar psoriasis.
They were talks on the microbiome, infections and psoriasis. This included ruling out the long-held theory of streptococcal throat infection leading to molecular mimicry triggering psoriasis onset. There was data presented on the oral microbiome as seen in psoriasis patients and clinical experience was shared about screening for infections prior to biologic treatment raising discussion around outdated testing for Biologics (such TB testing before IL 17/IL 23 inhibitors) and vaccination implications before and during biologics treatment.
Global perspectives of psoriasis and treatment for severe psoriasis were explored. With a Keynote lecture on the challenges in managing psoriasis and lower middle income countries particularly across the Middle East and an update on the current literature available for diagnosing and managing psoriasis in skin of colour.
Technology use for psoriasis care was presented in different ways. An example of Vision transformers used to estimate PASI in psoriasis patients was shared and Professor Justin Ko delivered a tour de force overview of technology in healthcare with a focus on Dermatology from experiences in Stanford.
Generalised pustular psoriasis was shown to be emerging from the disease control abyss with the advent of IL 36 inhibitors. Professor David Burden’s overview lecture from yesterday evening paved the way for further talks today on the changing paradigms of generalised psoriasis along with exploration of cellular cytokine explanation for the female preponderance of pustular psoriasis in women.
Areas of drug safety and Pharmacovigilance were reviewed with some evidence from real world data challenging preconceptions with regards to certain risks, such as cancer risk with TNF inhibitors. Rare adverse effects and how these may be missed in clinical trials and even registries were also discussed and work around identifying paradoxical eczema cases with TNF inhibitors, IL 17 and IL 23 inhibitors was presented.
Finally, newly available potential therapeutic targets were discussed including AHR pathway and the TYK2 pathway.
Let’s take a closer look at the details.
Speaker: Pr. Johann Gudjonsson
Exploring the IL 17 and IL 23 pathway and their role in psoriasis pathogenesis.
Professor Johann E Gudjonsson, Michigan USA, outlined the two sources of IL – 17: IL 23 dependent sources and IL 23 independent. The former coming from the innate immune cells and the latter from activated TH 17 cells. He showed that IL 17 A and IL 17 F are expressed in a similar way across different tissues and then went on to explain the differences between IL 17a and IL 17 F. Firstly IL 17 A is more potent but IL 17 F is more abundant. IL 17 A appears earlier in tissues then later IL 17 F production increases. The switch from IL17A to IL17F is regulated by the STAT5 pathway. N – wasp is an epigenetic regulator of keratinocyte IL 17 production and also other inflammatory cytokines. IL17A and IL17 F synergise with TNF alpha to amplify IL – 23 production.
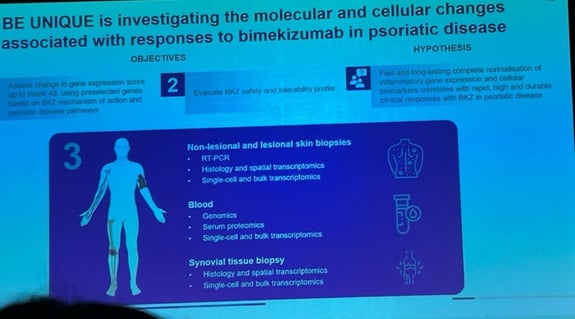
Professor Gudjonsson explained that Bimekizumab, a highly avid IL 17 inhibitor, was shown to normalise psoriatic transcription to a non-lesional skin level in around eight weeks.
He presented data from the BE RADIANT trial where there was a head-to-head comparison of Bimekizumab against secukinumab in a phase 3b trial. Bimekizumab maintained PASI 90 up to 28 weeks, which is longer than Ixekizumab, an alternative IL 17 inhibitor. When compared to the IL 23 inhibitors bimekizumab sits between guselkumab (PASI 90 reduced for around 20 weeks) and risankizumab (PASI 90 reduced around 40 weeks). The longer efficacy seen with bimekizumab compared with Ixekizumab was postulated to relate to bimekizumab’s ability to reduce tissue resident memory (TRM) T cell signature in tissue samples.
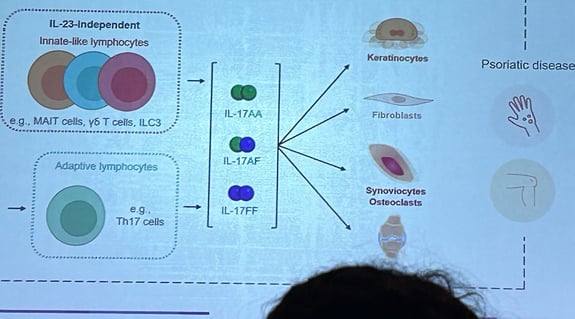
TRM T cells are CD8 cluster cells with a similar TCR. There is a hypothesis that their presence may be the link between skin psoriasis and psoriatic arthritis. There is a further theory that by reducing TRM cells in the skin may induce longer disease control. The BE UNIQUE study aims to examine the abs effect on TRM cells at a molecular and cellular level in psoriasis.
There was further discussion in his talk around predicting who will achieve a super response. Ultra short disease duration is a known strong predictor of super response but a correlation with low circulating IL 17 F levels was also noted.
Speaker: Pr. Johann Gudjonsson
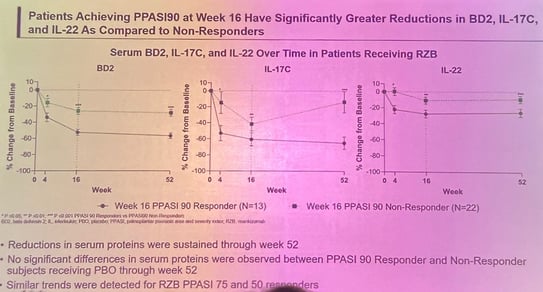
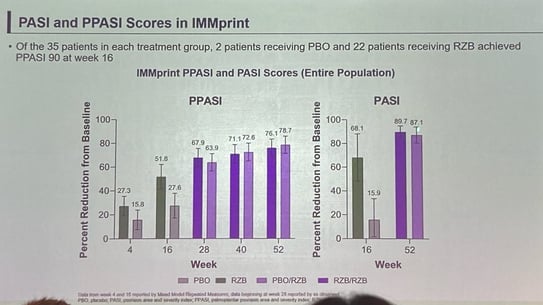
In a separate presentation, Pr. Gudjonsson shared results of IMMprint, a RCT treating palmoplantar psoriasis with the IL 23 inhibitor risankizumab. The basis for study was that clinically palmoplantar psoriasis appears to respond better to IL23 blockade than IL17 blockade but what mechanisms underpin this? Enrolled patients were randomised to placebo or risankizumab and at week 16 PPASI 90 was achieved in 22 out of 35 of the risankizumab treated patients compared with two placebo patients. In those patients who responded, reduced circulating levels of BD2, IL17 C and IL 22 were noted. However, there was no difference in observed IL17A levels between responders and non-responders at week 16 and the levels seen did not correlate with PPASI response, suggesting that the modulation of the IL 23 pathway in achieving response in Palmoplantar psoriasis goes beyond IL17a alone.

Speaker: Dr. Trudi Veldman
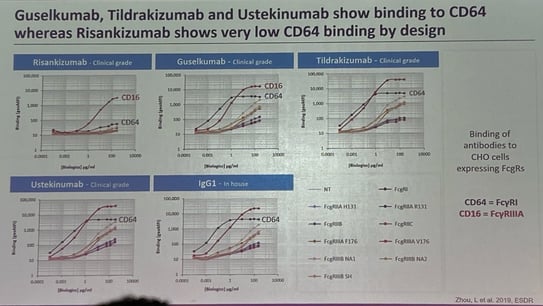
Dr. Trudi Veldman, Massachusetts USA, presented robust cellular and gene expression evidence of the mode of action of IL – 23 inhibitors from her group who have studied the IL23 target in depth. Firstly, she explained the available IL23 inhibitors: risankizumab, guselkumab and tildrakizumab; which target the P19 unit and ustekinumab which targets the P40 unit of IL 23 along with IL 12. These agents were compared at a cellular level in their lab.
Dr. Veldman explain the differences between risankizumab and guselkumab molecules:
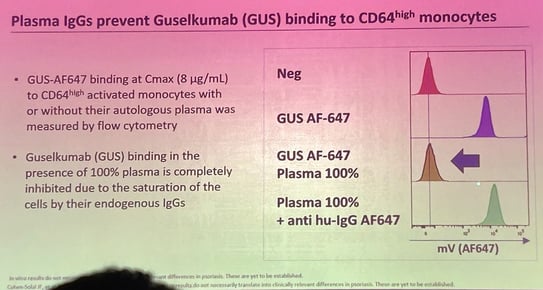
In vitro studies have looked at guselkumab CD64 binding on monocytes, with the hypothesis that inflammatory monocytes producing IL 23 are captured intracellularly before they are released into circulation. Veldman contested the clinical significance of this finding by showing that in physiological settings CD64 is a high affinity receptor for IgG1 and plasma IgG1 concentration will outnumber guselkumab IgG levels 600:1. From cellular lab studies monocytes primarily bonded with plasma IgG1 and although guselkumab binds monocytes strongly when alone, when in the presence of plasma and guselkumab binding dramatically reduces. Even when only 20% plasma is added to simulate tissue levels of plasma there continues to be more than 90% inhibition of CD64 binding by guselkumab (graph below). Overall suggesting that this pathway of Fc receptor portion binding by guselkumab is unlikely to be of clinical significance.
In the context of the vast volume of cellular data being presented throughout this conference this was an important reminder that in vitro results do not necessarily translate into clinically relevant differences in treatments.
Speaker: Pr. Jörg Prinz
Professor Jörg Prinz presented data from his team who have investigated the relationship between streptococcal throat infection and psoriasis, with the key initiating interaction occurring between B cells and melanocytes. Previously the team identified a specific psoriatic CD8+ TCR – Vα3s1/Vβ13s1 T cell clone in lesional skin. This interacts with the major psoriasis risk MHC allele: HLA C* 06:02, priming CD8+ T cells against melanocytes. B cells extracted from Streptococcus infected tonsils induced these auto-stimulatory CD8+ T cells, driving psoriatic inflammation. Previously, it was thought this process was initiated by molecular mimicry. Prinz and his team, however, have identified this novel pathogenic pathway. Moreover, they demonstrated that the CD8+ T cell priming B cell antigens show no similarity with streptococcal proteins, refuting the theory of molecular mimicry. In essence, inflammation by streptococcal tonsillitis induces an HLAC* 06:02 restricted autoimmune response with B cells that cross react against melanocytes in the skin triggering psoriasis. This raised several questions about the need for further investigation of the role of melanocytes in psoriasis pathogenesis.
Speaker: Dr. Luis Pig
Dr. Luis Puig provided a clinical overview of the importance of infections and vaccinations in the management of psoriasis. Key take aways from this clinically relevant talk included the following:
Speaker: Dr. Alex Birk Nielsen
Alex Birk Nielsen, Copenhagen Denmark, presented findings from his work in Professor Lone Skov’s group comparing the oral microbiota of patients with psoriasis, their cohabitant and healthy control controls. The background to this is that there is emerging evidence that the gut microbiota is linked with many inflammatory conditions and saliva microbiota has been associated with several conditions including diabetes, periodontitis, SLE, autoimmune thyroid disease and psoriasis. The group took a singular oral sample from 52 patients with psoriasis, 50 controls and 21 partners of patients with psoriasis. The latter were included to control for environmental confounders. When investigating the Microbiome diversity is key. In this study alpha diversity (diversity within sample) and beta diversity (diversity between species) were investigated. The findings showed lower alpha diversity in the psoriasis group compared with healthy control group and several taxal differences between the psoriasis and the control groups. Further studies are required to investigate the clinical implications of these findings.
Speaker: Dr. Yasmin Alfallouji
Dr. Yasmin Alfallouji, on behalf of Dr. Satveer Mahil’s group in London UK, presented work on development of an automated PASI assessment from real world images using standard and multi–Vision Transformers. Capturing 1109 images from 152 participants the group used both standard vision Transformers compared with multi–Vision Transformers to assess psoriasis patient PASI scores compared with two independent clinicians assessing in real life. The MultiViT model performed better than the standard ViT model. The intention is to integrate this into the Myskin app for patient directed monitoring of disease. Questions and discussion after this presentation provided food for thought, suggesting using this technology to improve the psoriasis severity scores beyond the rigid structure of PASI. Which led on well to the next invited speaker Professor Justin Ko.
Speaker: Pr. Justin Ko
Professor Ko presented concepts central to his work in spearheading Stamford’s medical dermatology department’s use of digital health. He talked about starting with the “end in mind” when planning any transformation of healthcare. He highlighted the value of clinicians in directing technology designers: where doctors define meaningful problems worth solving. By handing these problems to the technology designers clinically relevant solutions are more likely to arise rather than trying to fit existing technologies into current clinical models.
Professor Ko’s four points for the aim of artificial intelligence in healthcare included:
He advocated for an attitude shift towards letting go of reliance on face-to-face in clinic appointments when managing medical dermatology patients, sharing that 50% of Stamford’s medical dermatology is now conducted virtually. Questions at the end highlighted that virtual appointments are not new, with telephone reviews of patients occurring for decades. Professor Ko responded positively to this, pointing out that by using algorithms to highlight out of range monitoring findings from patient submitting clinical information alongside blood results, the number of patients flagged requiring doctors time to review and speak with them has dramatically reduced. Thereby reducing the burden on clinician time, freeing them up for other activities.
Professor Ko briefly touched on the use of artificial intelligence in psoriasis with the overall take away messages that good data is everything and advocating that the skill set of AI should be approached to better overall patient care, by utilising capacities the machines have that the clinicians do not, rather than trying to train AI to benchmark against expert clinicians.
He shared the cautionary tale of Google who designed an excellent lab based retinal screening technique with AI, but when implemented in the field in Thailand they had not considered the local infrastructure such as access to Wi-Fi and patient demand resulting in an epic failure. Google have since changed their model when designing AI for healthcare, engaging with local teams who deliver clinical care from the outset for better outcomes at the end. Once again, highlighting the importance of starting with the “end in mind.”
Speaker: Pr. Mahira El Sayed
Professor Mahira El Sayed, from Cairo, Egypt, delivered a compelling keynote lecture on the challenges of managing psoriasis and low middle income countries with a particular focus on the social and economic factors affecting psoriasis patients in the Middle East. Professor El Sayed noted the ongoing value of older but economical treatments within this population, such as methotrexate and the value of increasingly available biological biosimilars. She pointed out how there is under representation of Middle Eastern patients in clinical trials and the challenges and need to develop psoriasis guidelines for this geographical area, to serve these patients equitably and efficiently.
Speaker: Dr. Maria-Angeliki Gkini
Dr. Maria-Angeliki Gkini, London, presented a systematic review of the literature on psoriasis in skin of colour (SoC). The background to this work is that it is increasingly recognised that there is under representation of skin of colour in dermatology atlases and clinical trials, with RCT trials for psoriasis including only 14% SoC patients.
Systematic review of the literature unveiled the following:
The overarching finding was the paucity of literature on psoriasis in SoC, highlighting the need for further investigation. Social barriers to this include limitations in access to care for SoC patients which will contribute to under recognition of disease, likely more advanced disease at presentation and reduced enrolment in clinical trials. Gkini did highlight the current VISIBLE trial looking at guselkumab in SoC.
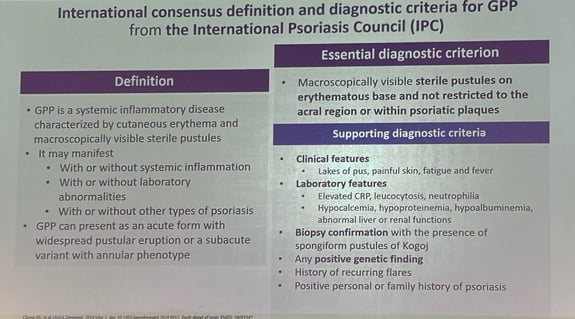
Speaker: Professor David Burden
The last session of day 1 saw Professor David Burden, Glasgow Scotland, present the IL 36 pathway in GPP, from gene to clinic. IL36Rn mutations have been identified in GPP patients and although not present in all cases, are associated with more severe disease. This systemic and life-threatening disease previously had a high mortality rate and the condition confers significant morbidity, associated with flares requiring hospitalisation. The il36 receptor inhibitor spesolimab, administered as a single infusion, works exceedingly quickly, with reduction in pustules reported from as early as 4 hours and overall clearance and resolution of fevers and systemic symptoms within a week.
Speaker: Pr. Siew Choon
Professor Siew Choon shared her career-long experience with managing GPP and the tragic impact this has had on many of her patients in her hospital in Johor, Malaysia. With the advent of IL36 receptor inhibitor spesolimab, however, she described the dramatic impact this treatment has had on these patients lives. Professor Choon expounded on the clinical diagnosis and management, biochemical pathophysiology and results from her work in delivering spesolimab clinical trials in this complex and distinct form of psoriasis. Some highlights included the following:
Speaker: Dr. Mrinal Sarkar
Dr. Mrinal Sarkar shared data from his work with Dr. Gudjonsson’s team from Michigan USA, exploring a possible underlying mechanism contributing to the prominent female sex bias seen in patients affected with pustular psoriasis. They identified sexual dimorphism in keratinocyte response to IL36 cytokines. Bulk RNA sequence data from primary keratinocytes showed female sex bias in IL36G response. Female keratinocytes displayed a more robust pro-inflammatory response to IL36G when compared with male keratinocytes. Female keratinocytes also showed increased expression of type one IFN and IFN signature genes pointing towards the association between IFN and IL 36 in female keratinocytes.
Speaker: Pr. James Galloway
Professor James Galloway, London, professor of rheumatology specialising in targeted therapies for rheumatoid arthritis and psoriatic arthritis, presented and invited lecture on the challenges of interpreting published safety data and identifying true causal adverse effects from drugs such as Biologics intended to be given long-term. Key takeaways included the following.:
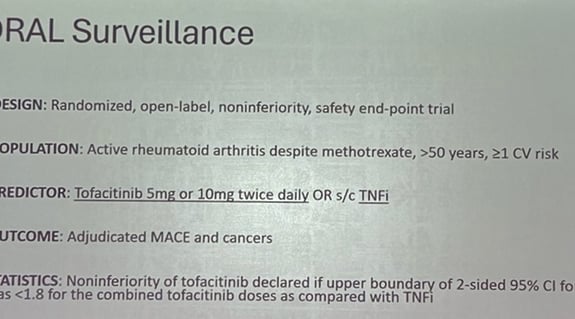
JAK inhibitors were shown to be associated with lymphoma in animal models however proportionally the dose used is much higher than in clinical practice for humans and this is seen with most drugs in mouse models in a dose dependent way. Nevertheless, off the back of this knowledge the ORAL surveillance open label trial is recruiting until 130 patients have had the event of cancer to further investigate the risk in practice.
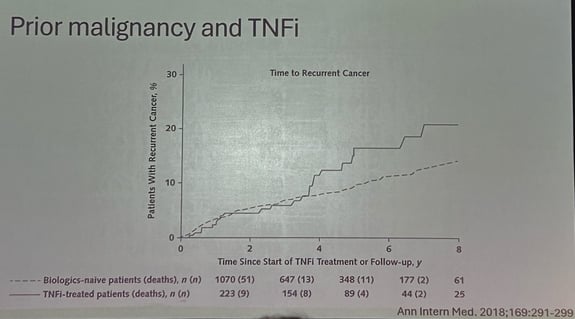
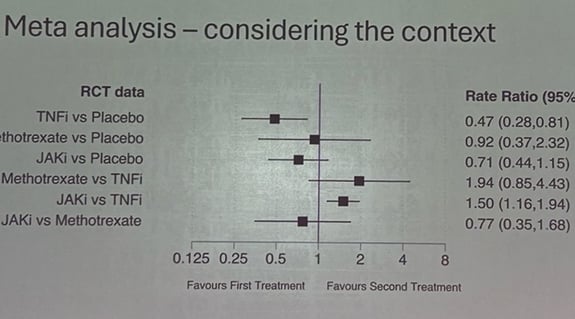
When comparing JAK inhibitors and TNF inhibitors and the rate of cancer the hazard ratio is 1.48. Limitations of this data when comparing with the dermatology population however is it in rheumatoid arthritis around 50% will be smokers and older. Also, the absolute risk is small. Nevertheless, even a small risk would likely influence patient’s choice regarding the treatment.
A network meta-analysis showed a significantly higher rate of cancer occurring with JAK inhibitor treatment compared with TNF inhibitors. This raises the question whether JAK inhibitors increase cancer risk or TNF inhibitors reduce cancer risk. Interestingly when comparing TNF inhibitors with placebo the hazard rate ratio for cancer was significantly lower with TNF inhibitors (HRR0.47 (0.28 to 0.81)). Suggesting TNF inhibitors may reduce the rate of cancer directly in this patient group.
Speaker: Dr. Ali Al-Janabi
Dr. Ali Al-Janabi presented data from a study looking at patients with “paradoxical eczema” secondary to Biologics for psoriasis (including TNF inhibitors, aisle 17 inhibitors and aisle 23 inhibitors). On mass cytometry blood samples from these patients revealed type 1 cytokine expression. Key findings included up-regulation of IFN and IL10 and also IL17a in paradoxical eczema.
New available therapies for novel targets
Speaker: Hannah Dawe
With the arrival of the new topical AHR (aryl hydrocarbon receptor) agonist, Tapinarof, Hannah Dawe, London Uk, presented work examining the role of AHR in psoriasis. AHR is anti-inflammatory in the skin and involved in skin barrier maintenance. CYP1A1 is a marker of AHR activation.
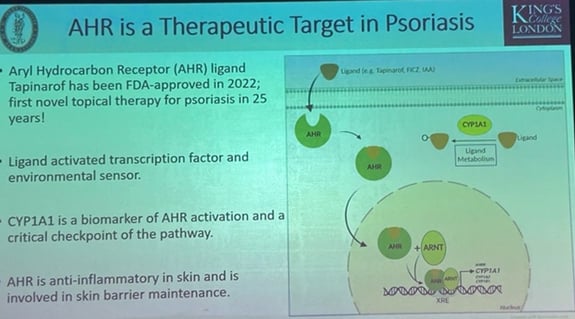
The group’s findings showed that CYP1A1 expression significantly decreased in psoriasis skin. This goes against other published findings. Most other studies performed in Korea so they propose that this may have been genetic variance. Healthy skin biopsy tissue exposed to psoriasis inflammatory cytokines increased AHR expression and CYP1A1. AHR levels appear to inhibit further AHR expression. A potentially exciting new target for topical treatment of mild to moderate psoriasis.

Speaker: Dr. Andrew Pink
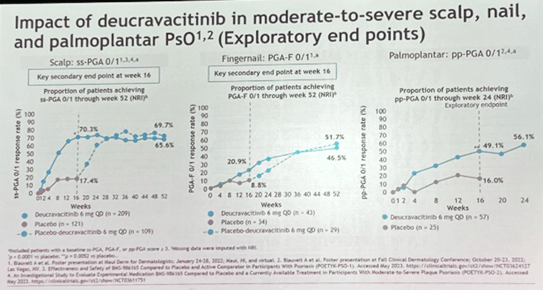
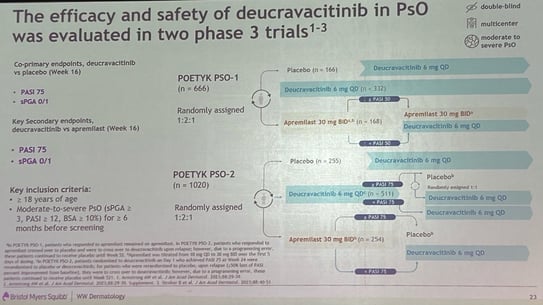
Dr. Andrew Pink, London UK, presented on a relatively newly available TYK2 inhibitor deucravacitinib. TYK2 is a part of the JAK family. Blockade of TYK2 inhibits JAK1 and JAK2 but not JAK3. The summary from POETYK clinical trials shows deucravacitinib achieved the primary endpoints of PASI 75 and sPGA by week 16 in 58% and 53% respectively. Side effects include nasopharyngitis and upper respiratory infections, but no significant adverse events were reported particularly MACE, DVT or PE.
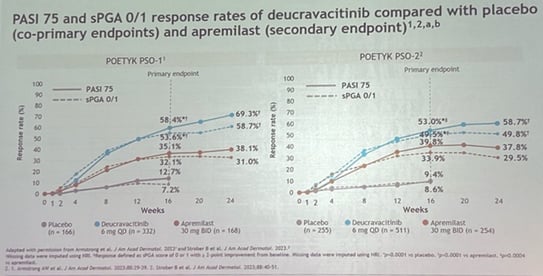
A current trial investigating deucravacitinib for high impact sites shows promising results 70% moderate severe scalp psoriasis achieving clear or almost cleared by week 16, 50% of nails psoriasis by week 52 and Palmarplantar psoriasis reduction by week 16.
The final morning of the Congress provided a holistic overview to psoriasis as a disease and its management and pointed towards areas for future research to address some of the needs and questions as yet unanswered in this complex disease.
Key themes from today included diet and the microbiome and how these might relate to psoriasis with findings from trial such as METRED – P and MANGO being shared along with expert experience from the holistic clinic model in Belgium.
Disease modification with the highly effective treatment options now available has been a theme running throughout the entire Congress. This theme was furthered today with an overview lecture and new findings from a pilot study aiming to induce remission with high dose IL23 inhibitor and the possible effects on reducing TRM cells postulated to be involved in long-term remission of psoriasis. From the opposite perspective, modification of treatment to optimise psoriasis management was also discussed. This included stratifying biological treatments by patient factors and the concept of precision biologics dosing, tailored to serum drug levels and patient factors.
The overall management of psoriasis patients with advocacy for holistic assessment of patients with psoriasis and a drive to rethink the patient reported outcome measures away from negatively posed questions shared from the POSITIVE trial. This theme culminated in the decades-spanning experience shared in the keynote lecture by Professor Mark Lebwohl, who presented a lifetime’s work delivering care and developing treatments for psoriasis patients.
Speaker: Dr. Sylvia Zanesco
Sylvia Zanesco, London Uk, presented pilot data from the current MEditerranean diet and time restricted eating dietary interventions for psoriasis (METRED – P) on behalf of the King’s College London group led by Professor Wendy Hall. This study tested the Mediterranean diet and time restricted eating diet on psoriasis patients with a PASI of at least five, a body mass index between 25 and 40, not currently receiving systemic treatment and with no underlying comorbidities. 24 Participants were randomised to one of Mediterranean diet (MD), time restricted eating (TRE) or a combination of MD with TRE. Patient reviewed in clinic at baseline and again at 12 weeks with assessments, including PASI, DLQI and body composition with the Tanita® scale. 10 participants have completed the study to date with interim data showing the following.:
The pilot data is planned to enable expansion to a fully powered RCT to further investigate.
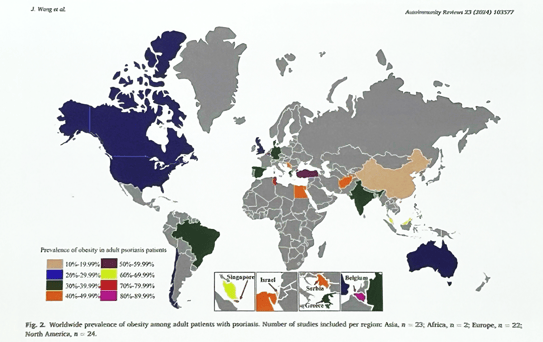
Speaker: Pr. Jo Lambert
Professor Jo Lambert, from Gent Belgium shared her invited lecture: understanding the impact of diet and the gut Microbiome on psoriasis. As Professor Lambert herself opened, this subject is a “Challenging and hypothesis generating topic”. She shared a compelling global map of obesity prevalence in adult patients with psoriasis showing rates varying from 20-29% in North America to 80-89% in Belgium. Indicating the prevalence of this association between obesity and psoriasis across the world.
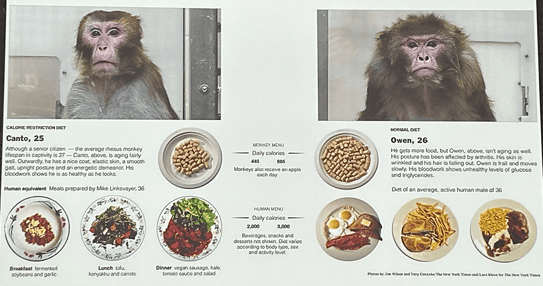
Professor Lambert went on to remind us of the 1980’s dietary study in two monkeys fed either a healthy or high caloric diet which showed the dramatic impact changing diet can have on developing a variety of morbidities.
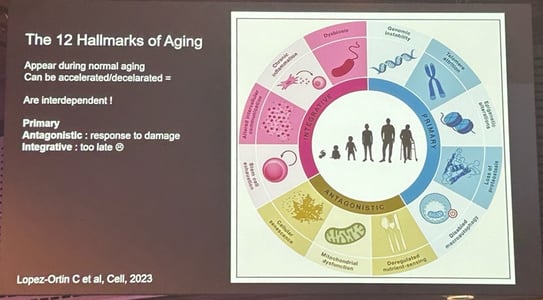
Professor Lambert shared the concept of “Psoriaging” whereby psoriasis accelerates aging. She outlined the 12 hallmarks of aging and dealt into some of the areas where psoriasis may directly accelerate the aging process.
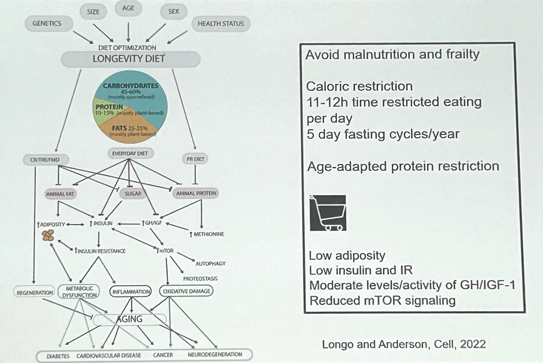
In psoriasis there is deregulated nutrient sensing mediated by the mTor pathway. When looking at how to modify this effect dietary changes might be an area of intervention as they can lead to change in mTor pathway. Caloric restriction diet with intermittent fasting have shown some benefit in reducing mTor signalling.
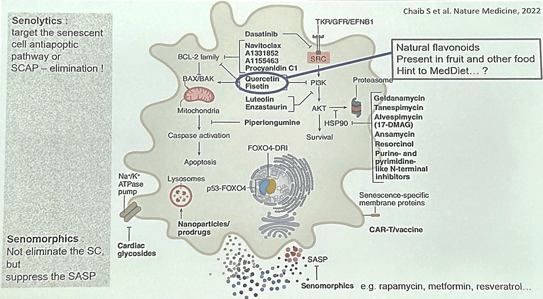
Professor Lambert also touched upon senolytics which target the senescent cell antioptic pathway or SCAP, and senomorphics which suppress senescence-associated secretory phenotype (SASP). Some of these are found in the Mediterranean diet (MD) including senolytic natural flavonoids present in fruit and other food: quercetin and fisetin and senomorphic resveratrol found in red wine.
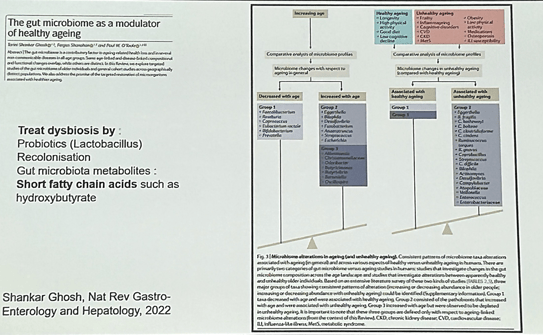
Furthermore, the microbiome appears to be involved in regulation of healthy ageing. A proposed mechanism for this is that So-called “Good bacteria” produce short fatty chain acids which have an overall systemic anti-inflammatory effect.
Although there was published dietary recommendations for adults with psoriasis or psoriatic arthritis published in JAMA 2018 this was based on very sparse available data. Therefore, Professor Lambert advocated for further research in this area to support evidence based dietary advice for patients.
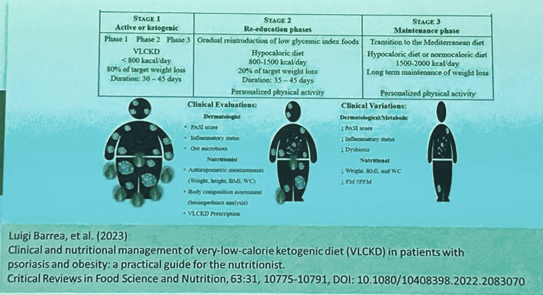
She shared Luigi Barrea’s dietary protocol for psoriasis published in 2023, which showed a good effect on PASI and reduction in inflammatory scores but cautioned that in practice this militant diet is probably not feasible for most patients.
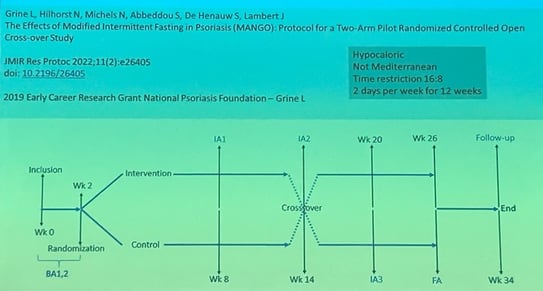
Professor Lambert presented her group’s data from the MANGO study. This took a small group of psoriasis patients who implemented Modified intermittent fasting, with low calorie diet. Although not statistically significant results did show a trend for improved clinical outcome and improvement in gut microbiome, but as yet it’s unclear if this was a cause or effect.
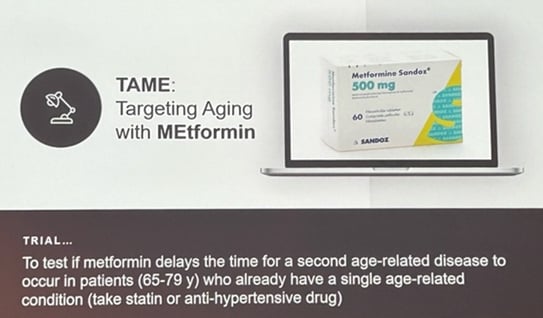
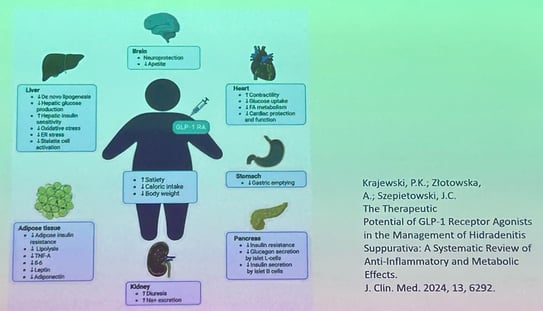
Professor Lambert acknowledged the challenges of behavioural modification for dietary changes and suggested that the treatments aimed at obesity in the context of psoriasis may be helpful and more acceptable to patients than diet. She mentioned the TAME trial investigating metformin’s effect on mTOR and targeting aging and the many possible emerging used for GLP-1 agonists. She did however advise not to underestimate the potential effect of dietary modifications on psoriasis control and offered experience from her practice that around 30% of her psoriasis patients show improvement with dietary measures. This was corroborated in discussion by experience from Professor Catherine Smith, London Uk.
Speaker: Dr. Andrew Blauvelt
Dr. Andrew Blauvelt, Oregon USA, presented the findings from the “knockout study”; a pilot study aiming to knock out inflammation and particular TRMs in psoriasis tissue with initial high dose risankizumab to induce disease remission.
Epidermal CD8 TRM with dependence on IL23 hypothesised to be key to psoriasis pathogenesis. Participants with severe psoriasis were randomised to either loading dose of 300mg or 600mg of risankizumab. The study design was double blinded, therefore all pts received 4 injections at baseline but dose different.
By Week 100, two of the 18 patients remained clear. Four out of 18 maintained PASI 90 and 75% of patients' psoriasis recurred gradually over a year.
No safety issues were seen and were not expected by the trial team, as similar doses are used in IBD patients in clinical practice.
Risankizumab down regulates IL7 signalling by reducing CD8+ TRM 17 cells. TRM th1 cells are not affected.
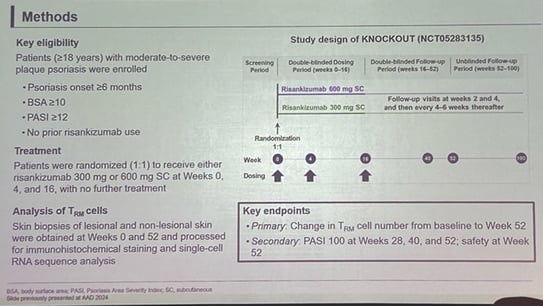
The summary findings included:
Pro inflammatory cytokine production by keratinocytes reduced
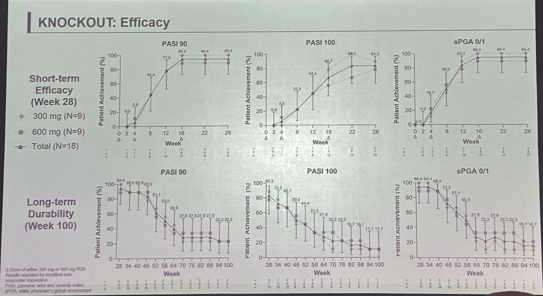
Dr. Blauvelt concluded these data provide mechanistic rationale for durability of response to risankizumab and support high dose induction of IL23 agent. He proposed the further hypothesis that if repeated in short duration disease groups they would likely see higher proportion controlled at week 100. Further investigation in a larger sample is needed.
Speaker: Professor Kave Shams
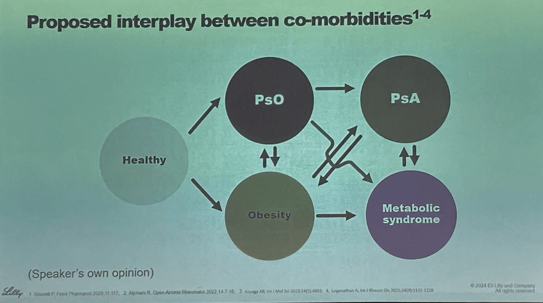
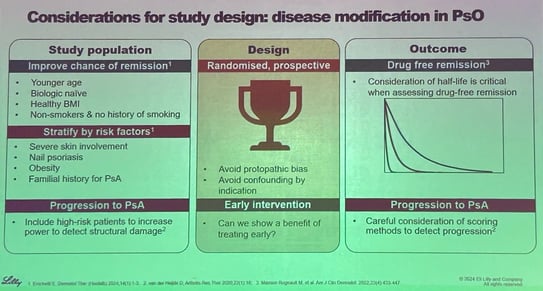
Professor Kave Shams, Leeds UK, discussed the concept of disease modification in his talk. The goal of achieving clear or nearly clear skin for psoriasis is now a reality, and patients are increasingly asking when they can stop treatment after reaching this stage. While biologics have allowed 50% of rheumatoid arthritis patients to achieve remission, psoriasis has not yet reached the same level of success.
A key issue is the definition of remission, which does not currently include the Dermatology Life Quality Index (DLQI) in published guidelines. When treatment is stopped, many psoriasis patients relapse, with most experiencing a relapse within one year. Immunological memory contributes to plaques reappearing in the same areas.
Another important factor is the drug half-life. Clinical trials assessing disease modification need to differentiate between true disease modification and the prolonged action of a drug due to its long half-life.
Psoriasis duration is linked to a higher risk of developing psoriatic arthritis (PsA), but the exact relationship between cutaneous psoriasis and PsA development is unclear. Identifying patients who will progress to PsA is challenging due to factors like protopathic bias—treating a disease before it’s visible, based on suspected risk.
The interplay between psoriasis comorbidities, such as obesity, is complex. Obesity not only causes inflammation but also places strain on joints, which can contribute to the development of PsA. Additionally, reduced physical activity due to weight gain may further exacerbate joint problems.
Study designs for disease modification in psoriasis need to take these complex interactions into account. The definition of remission is expected to evolve and should eventually incorporate patient-reported outcomes, which are currently absent from the Delphi definition of remission.
Speaker: Dr. Charlotte Thomas
Charlotte Thomas, King's College London, presented a framework for precision biologic dosing in psoriasis, emphasizing the variability in patient responses to treatment. Some patients are "super responders," while others require higher or lower doses to maintain control of the disease.
In conclusion, this research highlights the potential of precision dosing in psoriasis treatment, offering personalized therapeutic strategies that could improve patient outcomes and reduce the trial-and-error approach to biologic therapy.
Speaker: Pr. Lone Skov
Professor Lone Skov, Hellerup Denmark, discussed the importance of stratifying biologic treatments for psoriasis based on real-world evidence (RWE) to improve patient outcomes, reduce costs, and alter the disease trajectory. While biologics are effective for many patients, there are still cases of refractory psoriasis, highlighting an unmet need in treatment.
In conclusion, RWE is vital in stratifying biologic treatments to better match patients with the most effective therapies, particularly for refractory cases, while also addressing safety concerns and comorbidities in the broader population. Overall, data suggests that patient started on systemic treatment earlier had better overall outcomes.
Speaker: Pr. Ulrich Mrowietz
Professor Ulrich Mrowietz, Kiel Germany, referenced Professor Jonathan Barker’s idea that dermatology is now in a phase of evolution, not revolution, particularly in the management of psoriasis. Traditionally, the focus has been on visible skin symptoms, such as the Psoriasis Area and Severity Index (PASI), but the importance of understanding the patient’s experience is becoming clearer.
The WHO advocates for people-centered healthcare, shifting the focus from "What is the matter with you?" to "What matters to you?" This approach highlights the need to update patient-reported outcomes (PROs). Traditional PROs like the Dermatology Life Quality Index (DLQI) often frame questions in a negative light, which may not be the most effective way to understand patient wellbeing. The WHO-5, a more positive and patient-centric questionnaire, emphasizes overall wellbeing rather than just disease-related concerns.
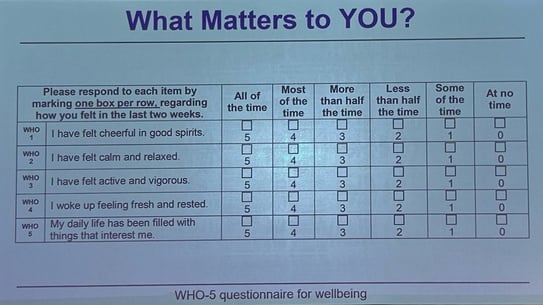
The POSITIVE study explored the impact of the IL-23 inhibitor tildrakizumab on psoriasis patients, assessing wellbeing through PROs like the WHO-5. The study also considered the wellbeing of patients’ partners and physicians. The goal was to explore how psoriasis impacts not only the patient but also those close to them. The WHO-5 score, which assesses overall wellbeing, was used as a benchmark, and baseline scores were similar to other serious conditions, such as breast cancer, with a 10% change considered a minimal clinically important difference (MCID).
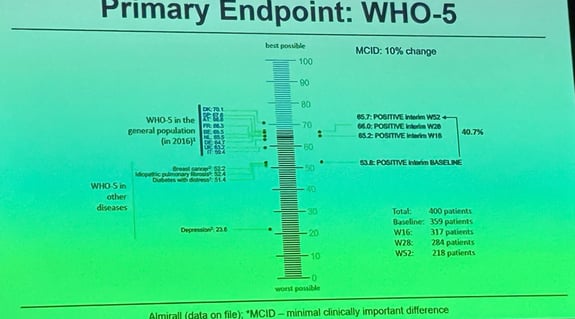
Key findings from the study include:
In conclusion, the POSITIVE study suggests the value of using PROs like the WHO-5 to better understand the broader impacts of psoriasis treatment, moving beyond visible skin symptoms to consider the patient's overall quality of life, as well as the wellbeing of their partners and the physicians involved in their care.

Speaker: Dr. Michael Sticherling
Dr. Michael Sticherling, Erlangen Germany, presented findings from a retrospective observational study on the impact of interdisciplinary clinical boards for managing chronic inflammatory diseases, including psoriasis. These weekly multidisciplinary team (MDT) meetings involve dermatologists, rheumatologists, and gastroenterologists.
Key points from the study:
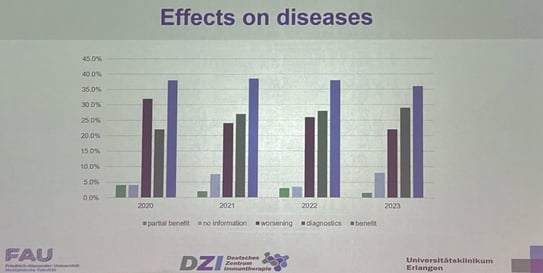
In conclusion, the study emphasizes that collaborative MDT meetings enhance patient care by integrating expertise across specialties, leading to better management of psoriasis and related conditions.
Speaker: Dr. Mark Lebwohl
Dr. Mark Lebwohl, New York USA, delivered a fantastic Keynote lecture, providing a comprehensive overview of psoriasis management, from its historical treatments to current advancements and future directions.
In conclusion, significant progress has been made in psoriasis treatment, with promising therapies in the pipeline and a better understanding of the disease's complexities and comorbidities.
Speaker: Dr. James Krueger
Dr. James Krueger, New York USA, presented results from the phase 2b study on Zasocitinib (TAK-279) an oral, highly selective TYK2 inhibitor that modulates key cytokine pathways involved in psoriasis. It targets cytokines that drive disease progression, specifically IL-17A and IL-17F, which are central to the inflammatory response in psoriasis.
In this Phase 2b study, approximately 70% of patients achieved a PASI 75. This data was derived from a subset of patients who provided skin biopsy and blood samples for analysis.
Key findings from the study:
This study suggests that Zasocitinib effectively targets the key inflammatory pathways in psoriasis, providing potential for significant clinical improvement in moderate to severe cases.
What is left to discover about psoriasis?
Some areas for future research suggested from this conference included
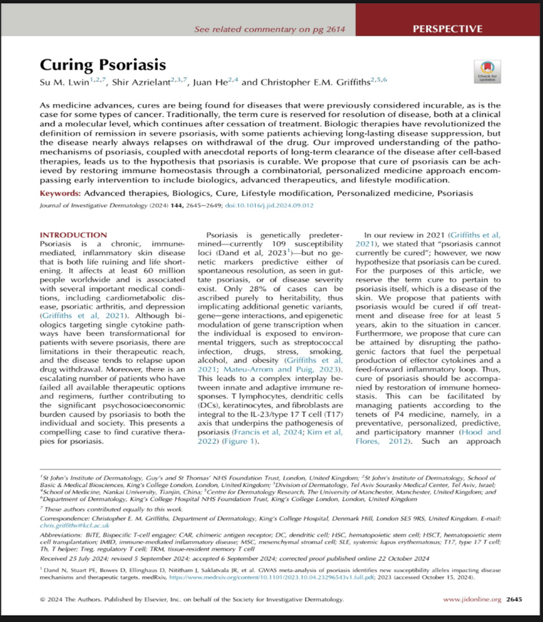
Su M. Lwin, Shir Azrielant, Juan He, Christopher E.M. Griffiths, Curing Psoriasis, Journal of Investigative Dermatology, Volume 144, Issue 12, 2024, Pages 2645-2649. https://doi.org/10.1016/j.jid.2024.09.012
The Psoriasis Gene to Clinic Conference 2024 highlighted many exciting advances in the understanding and treatment of psoriasis. While some new treatments overlap with historical therapies, the conference also debunked several previous misconceptions. Key developments include the identification of new treatment targets, with an increasing focus on disease modification and personalized treatment strategies. These advancements aim to tailor therapies to individual patient needs, potentially improving outcomes significantly. Additionally, there is growing optimism around the possibility of cure for psoriasis, marking a transformative shift in how the disease is approached and managed.



Interest of a novel dermocosmetic shampoo in the management of scalp psoriasis


What is psoriasis: causes, symptoms, treatments?


Skin of Color Update 2024 Bioderma Congress Reports