2 professionals
Bioderma Congress Reports AAD 2024
Bioderma Congress Reports AAD 2024
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
Benefit from valuable features: audio listening, materials to be shared with your patients
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations
Already have an account? login now
Reports written by Dr. Chris Callewaert (Dermatologist, Belgium), and Dr. Joël Claveau (Dermatologist, Quebec)
Related topics
Speaker: Teri Seeberger Greiling MD
Report written by Dr. Chris Callewaert
The microbiota exists on all barrier sites of the body, including the gut, skin, lungs, vagina, mouth, and more. The microbiome refers to the collective genome of these microbes. Within this ecosystem, various types of relationships exist, including pathogens, commensals, mutualists, and pathobionts, the latter of which may become pathogenic depending on environmental factors. Our microbiome is shaped by numerous factors such as birth method, diet, exercise, hormones, geographic location, medication, cosmetics, and drugs, with many medications acting as antibiotics.
Humans have coevolved with the microbiome, and its absence can lead to a weakened immune system or an immune system that attacks harmless host cells. The rise of inflammatory diseases can be attributed to the immune system's inability to distinguish between friend and foe.
Lupus, for instance, is often overlooked in textbooks concerning the impact of the microbiome on immune pathways.
Mechanism 1 involves cross-reactivity, where the immune system cannot differentiate between host and bacterial antigens. Some bacteria, such as Ruminococcus, Roseburia, and Porphyromonas, produce antigens like Ro60, leading to cross-reactivity.
Mechanism 2 involves bacterial translocation, where bacteria from the gut leak into the bloodstream and migrate to other parts of the body, including the skin and organs affected by lupus. Even beneficial bacteria like Lactobacillus reuterii and Ruminococcus can translocate, exacerbating the autoimmune response.
Fecal microbiome transplant has shown promise in conditions like ulcerative colitis and lupus, with multiple studies demonstrating consistent results. The gut microbiota also influences melanoma survival after immune checkpoint inhibitor therapy, with poorer survival rates observed in patients who received antibiotics prior to treatment.
Innovative approaches include engineering Staphylococcus epidermidis to produce melanoma antigens, prompting T cells to attack distant melanomas. Additionally, imbalances in dopamine levels can contribute to neurological conditions like Parkinson's disease and formication, highlighting the intricate interplay between microbiota and human health.
Speakers: Alan Irvine, Tissa R Hata, Jonathan Silverberg and Lawrence Eichenfield
Report written by Dr. Chris Callewaert
Alan Irvine
The skin serves as the body's primary barrier, with the immune barrier represented by Langerhans cells acting as a secondary defense.
Atopic dermatitis (AD) manifests through a complex interplay of three pathways:
AD commonly induces itching.
Loss of function of filaggrin, critical for skin health, increases the risk of developing AD (Odds ratio 3.1), asthma (Odds ratio 1.5), and peanut allergy (Odd ratio 5.3). Filaggrin monomers are cleaved by bleomycin hydrolase (Caspase 14, Caspase 1) in to NMF (moisturizing factor which keeps the skin hydrated)
Microbiome interacts with the stratum corneum. Forms biofilm. S. aureus
Stress exacerbates skin barrier dissolution, a trait with evolutionary roots for combating parasites and ticks.
Infant skin in pre-clinical AD: low NMF, ceramide, type2 skewing, microbiome alterations.
Many signs are there before AD kicks in.
Can barrier protection prevent AD?
Studies show no effect. Review by Kelleher & al. 2021
Yet, babies that received moisturizers had reduced AD incidence in the first year of life. But it’s a short-term effect.
Of the 3 major pathways that lead to AD, the immune targeting is the most tractable.
On Dupilumab, the skin barrier restores perfectly. 16 week study. Its like a house on fire: First solve the fire before fixing the roof.
Tissa R Hata MD
James Leyden's study in 1974 already showed S. aureus colonization in lesions of AD (Leyden & al., 1974), highlighting the skin's compromised defense mechanism against pathogenic invasion in this condition.
Normally, the skin serves as a robust barrier against pathogens. However, in AD, there's a notable decrease in the expression of antimicrobial peptides (AMPs). Additionally, AD-afflicted skin shifts from an acidic to a neutral pH environment, further hampering its protective capabilities. The deficiency in AMPs also impedes the induction of Th2 cytokines.
Caregivers serve as reservoirs for S. aureus, with a significant presence detected on both child-caregiver pairs and patients themselves, suggesting the potential need for caregiver treatment. Moreover, households harboring AD patients tend to exhibit higher S. aureus colonization rates.
Skin colonization by S. aureus often precedes clinical AD diagnosis in infants (Meylan et al., 2017). Interestingly, the presence of S. epidermidis on pediatric skin has been associated with protection against AD development (Kennedy et al., 2017).
Coagulase-negative staphylococci (CONS) produce their own bacteriocins, which inhibit the agr quorum sensing system in S. aureus, critical for its virulence and colonization (Nakamure et al., 2020). Infants who did not develop AD showed higher levels of S. aureus mutated in Agr quorum sensing virulence factors.
Research conducted by the Gallo lab identified commensal Staph strains capable of killing S. aureus. However, the prevalence of such strains was significantly lower on AD non-lesional skin compared to healthy skin, indicating a loss of beneficial commensals in AD-afflicted individuals. This loss may be attributed to the heightened sensitivity of CONS-AM+ strains to AMPs, leading to their rapid demise on AD skin (Nakatsuji & al., 2023).
The potential for microbiome manipulation to improve AD remains a subject of inquiry, with ongoing studies aimed at elucidating whether microbiome alterations alone can confer protection against AD development. Further research is needed to address this question conclusively.
Jonathan Silverberg
Jonathan Silverberg gave a great presentation and high-level overview on atopic dermatitis, and its onset at different ages. He included lots of pictures, and reviews to give an up-to-date presentation.
He noted that the pediatric population is much more prone to Staph toxins than adults. Their microbiome is also different. Kids have more commonly asthma, allergen-specific IgE and known genetic polymorphisms.
Set up approach of management of AD:
Patient is often convinced that the onset of AD is a food. He thinks that is a very bad idea, as there are random positives. It is not clinically relevant. If you follow them in that story, you condemn patient to a lifelong allergy, which is not a good idea. You actually want to expose them more, so they become more tolerable. AAAAI guidelines advise against elimination diet.
Lawrence Eichenfield MD (prof at UCSD, Rady children’s hospital)
According to Atopic Dermatitis guidelines, topical therapies include:
The three main points are:
1/ Care Plans and Regimens of Care: Tailored care plans are essential for effective management.
2/ Good Bathing Practices: Limited data exists on bathing practices, but moisturizing post-bath can significantly enhance skin hydration. Avoiding bathing to prevent skin dryness lacks evidence basis, and bathing may offer additional benefits in active eczema. Bathing and moisturizing together significantly increase skin moisture levels, whereas using only moisturizer results in less significant moisturization.
Bleach baths may have some positive impact but are not necessarily better than bathing alone. They do not affect the microbiome. Regular bathing, or potentially bleach bathing, is important in crusted eczema.
Moisturizers can help reduce itch, minimize signs, symptoms, and inflammation, and increase the time between flares.
3/ Anti-inflammatory Medications: Corticosteroids have a high level of evidence. They offer rapid anti-inflammatory response, are cost-effective, and come in a wide range of potencies. However, potential side effects include stinging/burning, atrophy, concerns about withdrawal phenomena, telangiectases, and adrenal axis suppression. While social media has raised concerns about steroid addiction and withdrawal, there is no conclusive proof in the literature. Topical calcineurin inhibitors (TCIs) provide a safe alternative, especially when steroid use is a concern. Short-term data is available for topical JAK inhibitors.
Emerging non-steroid topicals include nuxolitinib 1% cream, roflumilast 0.15% cream undergoing phase 3 studies, tapinarof 1% cream with promising phase 3 trial results and a pediatric study, and crisaborole 2% ointment with a one-year daily maintenance study.
Regimens may consist of monotherapy or a sequence of multiple therapies for improved outcomes.
He is co-author on the Myles & al. Roseomonas study to combat AD. However, it didn’t go through as it was a negative study. Double blinded clinical trial failed.
Speakers: Richard Gallo, Hilary Baldwin, Linda Stein Gold and James Del Rosso
Report written by Dr. Chris Callewaert
Richard Gallo MD – chair dermatology at UCSD
The classic model of acne is now considered outdated due to emerging understandings of systemic connections for disease triggers, including endocrine and environmental influences, diet, and comorbidities. Contrary to previous beliefs, there is minimal evidence supporting the proliferation of Cutibacterium acnes (C. acnes). Inflammatory triggers are recognized as unique to the disease, with the role of hypoxia and biofilms particularly notable in the absence of a follicular plug.
The concept of the holobiome is introduced, emphasizing not only the host but also the microbiome both on and within the host, in conjunction with the environmental metagenome. While few microorganisms are pathogens, most are mutualistic, commensal, or environmental contaminants, with the latter being largely irrelevant.
Similar to conditions like atopic dermatitis (AD) and psoriasis, acne is characterized by numerous complexities and interconnected factors.
Regarding the role of Cutibacterium acnes in acne, toxins produced by C. acnes, such as beta hemolysins and CAMP factors, are implicated in skin tissue damage. While C. acnes is equally abundant on healthy and acne-prone skin, certain ribotypes or subclasses may be more prevalent in acne. Some strains exhibit higher inflammatory responses, possibly due to plasmid-encoded factors, though the exact mechanisms remain unclear. Additionally, the inflammatory potential of C. acnes varies based on its location within the skin, with deeper layers associated with increased inflammation. The surrounding follicular cells also play a significant role, as they may become less effective in combating C. acnes, leading to heightened inflammation.
Diet and gut health also influence acne development. A questionnaire study on 300 acne patients and 120 controls have identified dairy as a potential trigger, while fruits and vegetables are considered beneficial. Commercial probiotics did not really help. The gut microbiome of acne patients suggests that certain bacteria, such as Bifidobacteria and Lactobacilli, may have a protective effect.
In light of these insights, the approach to combating C. acnes is evolving. Rather than relying solely on antibiotics, alternative strategies include neutralizing toxins through vaccination or antibody production, selective killing of C. acnes using beneficial skin bacteria like Staphylococcus capitis or Lactobacilli, minimizing fermentation, and exploring the potential roles of diet and probiotics. Future research will continue to refine these approaches.
Hilary Baldwin MD
Androgens are localized within the same cells where synthesis occurs rather than being released into circulation, indicating that testosterone may not serve as an accurate biomarker for androgens.
Clascoterone has shown promising success in acne treatment.
Combining clindamycin 1.2%, adapalene 0.15%, and benzoyl peroxide (BP) 3.1% has yielded favorable results, with good tolerability among patients.
New devices such as lasers offer selective photothermolysis of sebaceous glands, offering a safer option for individuals with darker skin tones, albeit requiring a considerable amount of time.
The social stigma surrounding acne was highlighted in a study involving 1300 participants who rated photographs depicting individuals with varying degrees of acne severity. The findings revealed that individuals with severe acne were perceived as less comfortable to befriend, date, hire, or feature in social media posts. They were also judged to be less intelligent, trustworthy, and likeable. These perceptions contribute to the sense of judgment experienced by acne patients.
An acne vaccine is being developed, with early-age public vaccine programs aimed at preventing future acne. Results from phase 1 studies are awaited, with the vaccine targeting virulence factors of Cutibacterium acnes (C. acnes).
It's important to note that C. acnes plays a crucial role in skin homeostasis, and any intervention should not indiscriminately eradicate all strains. There are three subtypes of C. acnes: Type I (IA1) is associated with acne, while Type II is typically found in healthy skin.
Linda Stein Gold MD
Patients with rosacea have an elevated risk of cardiovascular diseases, as evidenced by significantly increased odds of diagnoses related to circulatory system diseases, hypertensive diseases, cerebrovascular diseases, and arterial disease compared to controls.
Metronidazole is commonly used by rosacea patients; however, there are more effective alternatives available. Topical anti-inflammatory creams such as ivermectin have demonstrated superior efficacy compared to metronidazole. They not only work better than antibiotics but also offer longer-lasting remission. Achieving nearly clear skin typically takes about three months for remission, while complete clearance may require a longer duration, often five months or more, emphasizing the importance of striving for complete clearance.
The effectiveness of antibiotics in rosacea treatment can be attributed to their potent anti-inflammatory properties rather than their antimicrobial effects, as Cutibacterium acnes (C. acnes) is not strongly associated with rosacea.
Oral minocycline has shown significant efficacy, particularly at higher doses, with no observed impact on the microbiome, making it a viable option for rosacea management.
Benzoyl peroxide, when microencapsulated to stabilize it and reduce direct skin exposure, has yielded excellent results in treating rosacea. This formulation is well-tolerated and associated with prolonged remission, providing approximately 58 days of disease-free period.
Oxymetazoline, known for its vasoconstrictive properties, can effectively alleviate symptoms of rosacea by reducing redness and inflammation.
Additionally, paroxetine has emerged as an effective treatment for refractory erythema associated with rosacea, offering new hope for patients with persistent symptoms.
James Del Rosso (future AAD president)
The short answer is yes. The use of antibiotics (Abx) in dermatology is prevalent, but the timing and indication for their use are crucial considerations. Often, antibiotics are prescribed as a precautionary measure, even when the etiology of the condition may be viral. Dermatologists tend to prescribe antibiotics more frequently and for longer durations compared to other healthcare specialties.
An overview of antibiotics in dermatology reveals several key points. Topical anti-inflammatory agents like Dapsone are utilized, while monotherapy with topical antibiotics such as erythromycin, clindamycin, and minocycline is discouraged due to concerns about antibiotic resistance. The efficacy of erythromycin diminishes over time with prolonged use, and the relevance of its anti-inflammatory effects in acne management is debated. Combination therapy with benzoyl peroxide alongside clindamycin or erythromycin helps mitigate the risk of antibiotic resistance.
Optimizing topical therapy for acne involves incorporating gentle and straightforward skincare routines. Benzoyl peroxide, with its direct antimicrobial and comedolytic properties, is favored, especially in combination formulations to improve compliance and reduce the number of products used. Topical retinoids play a significant role in acne management, while the introduction of topical clascoterone adds another important mode of action to treatment regimens. Antibiotic monotherapy is best avoided to minimize the development of resistance, emphasizing the need for simplified combination therapies.
Oral antibiotics have widespread systemic effects and can impact various areas, including the skin, nasal passages, and gastrointestinal tract. They may inadvertently select for more Streptococcus bacteria, although they don't necessarily lead to strep throat. Tetracycline-based antibiotics, including doxycycline, minocycline, and the more recently developed sarecycline, are commonly used due to their favorable safety profiles for chronic use.
Speakers: Gregory Orlowski and Lisa Shen
Report written by Dr. Chris Callewaert
Gregory Orlowski MD (Boston Medical Center)
Hidradenitis Suppurativa (HS) initially presents similarly to acne but undergoes distinct changes over time, evolving into a complex structural disease with significant inflammatory components. It shares numerous similarities with psoriasis, and many drugs effective for psoriasis also offer relief for HS symptoms.
The HiSCR-50 score is commonly used to measure HS severity, although other assessment tools are also available. The condition progresses through stages: Stage I, characterized by inflammation and amenable to medical treatment; and Stages II/III, involving structural changes requiring surgical intervention.
HS is notably more complex and inflammatory than psoriasis, with patients facing elevated risks of suicide and experiencing considerable impairment in various aspects of life, including employment and relationships.
Management strategies for HS include surgical interventions, such as laser therapy, cryoinfulliation, tumescent Kenalog, and intralesional detergent administration. Patients face a lot of doubt, fear and have a lack of information on the disease. Antibiotics have shown efficacy, and patients often seek relief from pain.
While biologics are standard for treating psoriasis, HS requires a multidisciplinary approach beyond biologics alone due to its unique challenges.
The impact of smoking cannabis on HS outcomes remains unclear, with conflicting evidence suggesting both improvement and exacerbation of symptoms. The speaker recommends exploring THC-based treatments without the need for smoking in HS patients.
Lisa Shen (Boston Medical Center)
Hidradenitis Suppurativa (HS) tends to manifest at an earlier age in female patients, often showing symptoms before the age of 18. Diagnosis is often delayed, taking over seven years on average, as initial symptoms are mistaken for boils or abscesses. Comorbidities associated with HS include acne, obesity, and anxiety, with the mean age of onset around 13 years. Additionally, HS is prevalent among many Black patients, with risk factors including obesity, acne, acanthosis nigricans, depression, PCOS, anxiety, smoking, and insulin resistance.
Lifestyle modifications are challenging and often require the involvement of the entire family. These modifications include weight management, smoking cessation, reducing friction in clothing, minimizing shaving, and implementing proper wound care practices.
Medical treatment options for HS include antibiotics such as doxycycline, clindamycin + rifampicin, augmentin, azithromycin, and ertapenem. Spironolactone may be prescribed to manage hormonal flares in HS, especially in cases of concomitant PCOS and hirsutism, but it is recommended only if the menstrual cycle is well-established due to potential side effects.
Metformin may be prescribed in adolescents to address insulin resistance and aid in androgen inhibition for those with PCOS, with caution advised regarding gastrointestinal distress. Isotretinoin is considered for early HS cases, particularly when acne is also present, while vigilance for signs of inflammatory bowel disease (IBD) is essential due to the comorbidity between HS and IBD.
Biologics such as adalimumab, infliximab, ustekinumab, secukinumab, and ixekizumab are utilized in HS treatment. JAK inhibitors are also emerging as potential options, although their long-term effects on growth remain uncertain.
Surgical interventions for HS include intralesional triamcinolone injections, laser hair removal, deroofing procedures, and excision, aiming to alleviate symptoms and improve quality of life.
Speakers: Eva Parker, Sarah Jane Coates, Alexandra P Charrow, Aisha Sethi and Zachary A Zinn
Report written by Dr. Chris Callewaert
Eva Parker MD
The majority of dermatologists acknowledge the significant impact of climate change, particularly as temperatures rise by 1.5 degrees Celsius. Heat plays a foundational role in climate change's effects on dermatology, with regions like the Arctic experiencing much warmer temperatures. Climate-related events such as droughts, wildfires, hurricanes, and flooding are becoming more frequent, especially in low- and middle-income nations.
Various factors contribute to climate change, including human behavior such as the release of long-lasting CFCs into the atmosphere. Heat also leads to the production of ozone, contributing to air pollution levels that exceed WHO limits for much of the population.
The impacts of climate change are far-reaching, affecting every organ system, including the skin. Certain groups are particularly vulnerable, including outdoor workers, women, individuals with skin of color, indigenous populations, and those living in poverty.
In addition to health impacts, climate change can damage infrastructure, lower real estate values, and threaten health systems during extreme events like hurricanes, floods, tornadoes, and wildfires. Ultimately, climate change represents one of the most significant crises of the century, serving as a force multiplier for health impacts, equity issues, and challenges faced by the health sector.
Sarah Jane Coates MD
Pediatricians play a crucial role in mitigating the effects of climate change on children and supporting families in adapting to these changes. Children are particularly vulnerable to climate-related impacts due to their higher surface-to-volume ratio, which increases susceptibility to changes in temperature, air quality, water quality, and food quality. Heat-sensitive skin conditions, such as atopic dermatitis, disorders of cornification, ectodermal dysplasia syndromes, and conditions requiring medication that impairs sweating, are of particular concern.
Climate change contributes to the spread of vector-borne diseases like dengue fever, with Aedes mosquitoes proliferating due to factors such as urbanization and globalization. Rising temperatures increase the risk of disease transmission, with dengue fever becoming more prevalent, especially among children and pregnant women. Additionally, Kawasaki disease incidence tends to rise after floods or heavy rainfall events, although the exact causes are not fully understood.
Mass population displacement, as seen in refugee camps, exacerbates various skin-related diseases. Furthermore, psychodermatology highlights the impact of stress on conditions like atopic dermatitis, underscoring the importance of addressing mental health in dermatological care.
Pediatric dermatologists should take proactive steps to address climate-related health risks. This includes ensuring access to air conditioning during heatwaves, employing motivational interviewing techniques to encourage behavior change, and utilizing storytelling to foster empathy and understanding among patients and families. Additionally, virtual assessments can help reduce the need for families to travel long distances for medical appointments, minimizing carbon emissions associated with transportation.
Alexandra P Charrow MD
Pollution and heat have significant implications for dermatological conditions like hidradenitis suppurativa (HS) and atopic dermatitis (AD). There is growing evidence that air pollution, particularly particulate matter (PM), nitrogen dioxide (NO2), and sulfur dioxide (SO2), can exacerbate skin diseases.
Studies have shown that exposure to PM can increase Staphylococcus aureus colonization in mouse models, and there is a documented association between PM exposure and AD in a Korean study. The effects of air pollution on skin conditions may vary depending on geographical location, with real impacts observed in patients, especially vulnerable individuals. For example, there has been an increase in AD-related healthcare visits following wildfire events!
Similarly, NO2 and SO2 have been linked to AD flares (Korean study), with increased healthcare visits noted after exposure to these pollutants. As heatwaves become longer and more frequent, urban heat islands exacerbate the problem, creating significantly warmer conditions in cities compared to rural areas. This increased heat can impair the body's ability to dissipate heat through sweating, leading to exacerbations of skin conditions like AD, psoriasis, ichthyoses, and systemic sclerosis. AD tends to be more prevalent in hotter weather conditions.
The relationship between heat and HS flare-ups has also been documented, with studies suggesting an association. Managing hyperhidrosis, wearing loose-fitting clothing, and monitoring mental health during warmer periods are recommended strategies for mitigating the impact of heat on HS symptoms.
Aisha Sethi MD
The speaker spent a significant part of her childhood in Pakistan and also worked there in 2010 and 2022. Pakistan, despite contributing less than 1% of greenhouse gas emissions globally, experiences profound impacts from climate change, driven largely by human activities. Deforestation in regions like Brazil exacerbates these effects, leading to environmental degradation and climate-related challenges.
Pakistan has become a notable example of the consequences of climate change, with incidents like climate migration becoming increasingly common. Signs of climate-related diseases like dengue fever are prevalent in almost every neighborhood, highlighting the public health impact. The melting glaciers of the Himalayas contribute to larger and more frequent floods in Pakistan, damaging infrastructure and displacing communities. After floods, outbreaks of diseases like diarrhea, dengue, and malaria become more prevalent.
One notable aspect of the dengue fever outbreak is the behavior of the Aedes mosquito, which is primarily active during the day, increasing the risk of transmission. With her experience, she understood the urgent need for essential drugs like gentian violet to combat various bacterial and fungal infections, which have become more common in Pakistan between 2010 and 2022. Additionally, there has been a notable increase in snake bites, attributed in part to the warmer climate, with a 2-degree increase leading to a 6% rise in incidents.
The spread of diseases like dengue fever, once associated mainly with travel to affected regions, has become a global concern, with cases now appearing in unexpected places like Florida among individuals who have not traveled abroad. This trend underscores the global impact of climate change on disease distribution and prevalence.
Zachary A Zinn
The lengthening of vector seasons due to climate change has resulted in a notable increase in Lyme disease cases. This shift reflects the broader trend of climate change exacerbating health issues worldwide. Interestingly, the healthcare system itself contributes significantly to environmental degradation, thereby perpetuating the cycle of climate change.
Both electricity consumption and waste generation within the healthcare sector contribute significantly to its environmental footprint. These two factors represent substantial sources of greenhouse gas emissions and pollution. Thus, as the healthcare system works to address the health impacts of climate change, it must also confront its own environmental footprint and strive to implement more sustainable practices.
Speakers: Jean McGee, Cecilia Larocca, Alan Zhou, Stephanie Gallitano, Martina Cartwright, Apostolos Pappas and Li-Chi Chen
Report written by Dr. Chris Callewaert
Jean McGee PhD MD (Harvard Medical School)
Despite the early hour, the session attracted significant interest, with attendees posing numerous questions afterward.
We are more bacteria than human.While humans possess a core human genome, the variability of the human microbiome is equally crucial. Studies involving gut microbiome transplants in mice have shown that such transplants can induce obesity or leanness in the recipient mice, underscoring the potential connection between gut health and metabolic outcomes.
Three primary targets were discussed: oral antibiotics, dietary interventions, and probiotics. It was noted that isotretinoin has a lesser impact on the gut microbiome compared to antibiotics like doxycycline, which can have a significant and possibly long-lasting effect on gut microbiota composition.
Regarding the long-term consequences of antibiotic use, it was acknowledged that there is indeed a lasting impact, with implications for liver metabolism.
The session also delved into the effects of dietary interventions, such as the Mediterranean diet, on the gut microbiome. Studies have shown that adherence to such diets can lead to changes in the gut microbiota, potentially slowing the aging process and improving cardiovascular health markers.
In terms of the gut-skin axis, the impact of diet on conditions like acne was explored. High-glucose and high-fat diets were noted to activate pathways associated with acne, although research in this area remains limited.
Regarding probiotics, while the US FDA does not require approval for their use, no health claims for probiotics have been approved by the FDA. However, studies have shown promising results, particularly in mitigating antibiotic-associated diarrhea when taken after a course of antibiotics. Lactobacillus rhamnosus GG was specifically recommended for this purpose.
For atopic dermatitis (AD) patients, lower levels of Bifidobacterium in the gut and higher levels of E. coli and C. difficile have been observed. While many studies have explored the use of probiotics in AD, findings have not been consistent, highlighting the individualized nature of treatment experiences.
Overall, while no specific probiotics were recommended for AD or acne, it was noted that probiotics might offer benefits, with the timing of administration, such as during pregnancy, being particularly important.
Cecilia Larocca MD
The session delved into the intricate relationship between the gut microbiome and cancer, highlighting the growing body of knowledge in this area. It was noted that there are more bacterial cells in the human body than human cells themselves, with bacteria even present in the breast, contrary to previous beliefs of sterility. This microbial presence may occur through translocation from the gut or adjacent locations such as the skin.
The focus has shifted to the tumor microbiome as a new frontier, particularly in chemotherapy resistance and the amplification of immunotherapy effects. Notably, recent research has identified specific bacteria associated with responses to immunotherapy, allowing for the prediction of responders versus non-responders.
Various mechanisms were discussed regarding how the gut microbiome affects the immune system, including the release of metabolites impacting T-helper cell responses, the activation of antigen-presenting cells (APCs), and the cross-reactivity of bacterial antigens with tumor neoantigens. The timing of antibiotic administration was highlighted as crucial, with studies showing worse outcomes when antibiotics were given within 60 days before or after immune changes.
While the impact of diet on cancer treatment outcomes was explored, the data remains relatively weak, particularly in the context of melanoma. The session emphasized the need for solid prospective randomized trials to ascertain the effects of diet and supplements. However, caution was advised regarding the use of supplements, as some, like vitamins C and E, have shown potential harm, including an increased risk of melanoma.
Despite the uncertainties surrounding diet and supplements, there is evidence suggesting that dietary modifications, such as high-fiber diets, may modify responses to cancer treatment. However, the use of probiotics in melanoma patients undergoing immunotherapy did not yield beneficial results in a prospective study, contrary to expectations.
Overall, while further research is needed to fully elucidate the role of the gut microbiome and dietary interventions in cancer treatment, emerging evidence suggests promising avenues for improving treatment outcomes and overcoming resistance to immunotherapy, including the potential use of fecal microbiota transplantation (FMT) and high-fiber diets.
Alan Zhou (Northwestern university)
The role of the microbiome is increasingly being investigated across a wide range of skin disorders, including conditions such as Hidradenitis Suppurativa (HS), pyoderma gangrenosum (PG), lupus, vitiligo, eczema, psoriasis, acne, seborrheic dermatitis (SD), and wound healing.
In the case of Cutaneous T-cell Lymphoma (CTCL), it has been observed that patients are commonly colonized by Staphylococcus aureus (S. aureus). Mouse models of CTCL progress rapidly when there is Staph coverage, suggesting an impact of antibiotics in resolving CTCL skin conditions.
CTCL patients, typically older individuals, tend to have more Gram-positive bacteria and there is a higher incidence of sepsis, particularly in more advanced stages of CTCL. Factors such as skin type and ethnicity are also considered important in CTCL.
Shifts in bacterial composition have been observed in CTCL, with S. aureus being particularly significant due to its adhesion factors, pro-inflammatory factors, toxins, and ability to disrupt the skin barrier and produce superantigens. Additionally, other skin bacteria like Staphylococcus argenteus, Bacillus safensis, and Corynebacterium tuberculostearicum may also play a role alongside S. aureus.
The relationship between the nasal microbiome and CTCL has been explored, revealing associations with altered nasal microbiota characterized by the presence of S. aureus and Staphylococcus epidermidis (S. epi). However, further research is needed in this area.
Studies have also investigated the impact of the gut microbiome on CTCL, revealing similarities to the gut microbiome found in conditions like atopic dermatitis (AD) but not in psoriasis. Loss of protective gut commensals, including butyrate producers and anti-inflammatory species, has been observed in CTCL.
In terms of the skin microbiome in CTCL, higher levels of S. aureus and lower levels of S. hominis have been noted, along with increased abundance of Streptococcus. Phototherapy in responders has been associated with increased alpha diversity on the skin microbiome.
Key takeaways include the potential role of S. aureus and other bacteria in driving disease activity in CTCL, the presence of microbial biomarkers predictive of treatment responsiveness, and the observation that CTCL skin in African-Americans tends to have higher relative abundance of staphylococcal bacteria.
The concept of using "designer bugs" as cancer drugs is an area of ongoing research, with promising prospects for the future. Overall, while probiotics may be effective in some cases, their efficacy is likely to be individualized, emphasizing the importance of precision medicine in treating skin disorders like CTCL.
Stephanie Gallitano MD
In the review of Inflammatory Bowel Disease (IBD), a comparison is drawn between Ulcerative Colitis (UC) and Crohn’s disease, highlighting the complex interplay among environmental factors, the microbiome, and lifestyle in these conditions. These two disease are more of a spectrum, rather than 2 clearly different disorders.
IBD is often associated with other autoimmune diseases such as rheumatoid arthritis and psoriasis, suggesting a shared underlying mechanism among these conditions.
Neutrophilic disorders can manifest in IBD patients, as evidenced by a case where a patient presented with pustules on the chest resembling acne, accompanied by smaller pustules on the back. Biopsy revealed a significant presence of neutrophils, indicating neutrophilic dermatosis. Similar lesions were observed on the chin, further supporting the association.
Bowel-associated dermatosis-arthritis syndrome, characterized by pustules in the mouth, hands, and feet, accompanied by neutrophils, is observed in patients who have undergone bowel bypass or gastrointestinal surgery, leading to a blind loop. Treatment typically involves restoring a healthy gut microbiome, although antibiotics alone may not suffice, necessitating the addition of immunosuppressants.
IL17 inhibitor-related pyoderma and IBD can present with symptoms such as diarrhea, abdominal pain, fever, and bloody diarrhea, along with elevated fecal calprotectin levels, white blood cell count, erythrocyte sedimentation rate, and C-reactive protein.
The use of antibiotics has been linked to the development of IBD, particularly in children who are exposed to multiple courses of antibiotics, with the highest risk observed following 5+ courses and for courses of nitroimidazoles and fluoroquinolones.
Martina Cartwright PhD (University of Arizona)
The pursuit of natural alternatives to Western medicine arises from frustration with existing therapies, leading to a focus on water-soluble and fat-soluble nutrients, as well as minerals, in dermatological care.
Water-soluble nutrients such as vitamin B and biotin are essential for skin health, while vitamin C aids in collagen formation, and antioxidants like carotenoids, vitamin A, and lycopene offer protection against environmental damage.
Fat-soluble nutrients play roles in skin structure and wound healing, with vitamin A, vitamin D, and vitamin E serving as key players in these processes.
Minerals like zinc, copper, selenium, and iron are crucial for skin health, with iron deficiency being particularly prevalent in the Western world. Topical applications of minerals like zinc and copper can also benefit the skin.
Overnutrition and undernutrition both contribute to skin issues, with overnutrition leading to vitamin toxicity and undernutrition being common in elderly populations or those with poor diets, illness, eating disorders, or malabsorption issues.
Medical Nutrition Therapy (MNT) offers a comprehensive approach to nutrition intervention, with protocols existing for various health conditions such as diabetes, cardiovascular disease, oncology, weight management, and food allergies, often covered by insurance.
Functional foods rich in polyphenols found in fruits and vegetables are desirable for promoting skin health, while neutraceuticals and phytochemicals offer additional benefits.
Avoiding excess consumption of sugar, salt, stimulants like caffeine, and spirits is advised, as they can have adverse effects on skin health and overall well-being.
Obesity is linked to dermatological conditions due to its role in promoting inflammation through adipose tissue, which produces inflammatory cytokines. Medications like GSP1 agonists can help mitigate weight-related issues by slowing gastric emptying.
Rapid weight loss can negatively impact skin health by disrupting collagen structure and elastin degradation, leading to premature aging.
Choosing high-quality carbohydrates, considering factors like glycemic index, whole grain content, fiber content, added sugar percentage, degree of processing, environmental sustainability, and protein composition, is crucial for overall health and reducing the risk of diabetes.
Apostolos Pappas PhD (Rutgers)
Research indicates that essential fatty acids, such as linoleic acid (omega-6) and alpha-linolenic acid (omega-3), are crucial for skin health, as our bodies cannot produce them. Approximately 40% of these essential fatty acids end up on the skin, according to studies using radio-labeled essential fatty acids. For example, in a human study using flaxseed oil, linoleic acid was shown to improve skin hydration, transepidermal water loss (TEWL), and roughness.
Regarding the treatment of atopic dermatitis (AD) with probiotics, studies have yielded mixed results. Some studies in Asia have shown improvements, while others in Europe did not. The effectiveness of probiotics appears to be strain-specific, with Lactobacillus salivarius and Lactobacillus fermentum reducing the SCORAD index in children with AD, while Lactobacillus plantarum and Lactobacillus rhamnosus GG (LGG) did not show significant effects. However, it's important to note that no probiotic has shown efficacy comparable to dupilumab, and elimination diets are not considered a cure for AD.
Research suggests that a low glycemic diet may improve acne symptoms, with studies conducted in various countries, including the USA, Australia, Korea, and Turkey. While the link between acne and diet remains controversial, some associations have been observed, particularly with skimmed milk and acne compared to whole milk. Additionally, there is ongoing research on the impact of the Mediterranean diet on acne.
Psoriasis is recognized as a systemic disease, often associated with other conditions such as diabetes, metabolic syndrome, and cardiovascular disease. The gut microbiome appears to play a role in psoriasis, with weight loss showing the strongest evidence for improving symptoms.
For rosacea, certain foods have been found to exacerbate flares, and further studies on the microbiome and associations with Helicobacter pylori are ongoing. The American Academy of Dermatology (AAD) recommends avoiding specific food triggers to manage rosacea symptoms.
Li-Chi Chen MD
Higher serum glucose levels are associated with a higher perceived age, with diabetic patients perceived as the oldest, but also non-diabetic individuals with high glycemic blood levels appearing older. For every 18mg/dl increase, there is an extra 0.4 years perceived age.
A healthy diet is linked to fewer facial wrinkles, as adherence to a predefined healthy diet is associated with less facial wrinkling. Conversely, consuming more snacks is correlated with more wrinkles, while consuming more fruits is associated with fewer wrinkles.
Aging and the skin involve intrinsic and extrinsic factors. Intrinsic aging entails the loss of collagen and elastin, resulting in fine wrinkle formation, as well as epidermal, dermal, and extracellular matrix atrophy, making the skin less elastic and more fragile. Extrinsic aging, influenced by environmental factors such as sun exposure, stress, chemical exposure, and diet, can exacerbate facial sinking or sagging.
Sugar contributes to collagen degradation by binding to proteins like collagen and elastin, leading to deformation in glycated skin. Chronic elevated blood sugar levels can accelerate the breakdown of collagen fibers.
To combat dietary advanced glycation end products (AGEs), it's recommended to limit simple sugars, favor fruits, vegetables, whole grains, and whole foods, and restrict meat consumption and processed foods. Diabetics should aim for good glycemic control and vary cooking methods, favoring boiling, poaching, and steaming over high-temperature cooking.
Collagen supplements, although challenging to deliver to the skin due to their large molecular size, have shown promise in improving skin hydration and elasticity in both short-term and long-term studies.
Diet can influence perceived age, with diets rich in vitamin C and linolenic omega-3 fatty acids associated with a lower perceived age. Nutrition also plays a role in photo damage, with individuals consuming eggs, yogurt, legumes, vegetables, nuts, olives, cherries, melons, jam, tea, and water showing fewer wrinkles due to reduced sun exposure.
Both the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet are recommended for their health benefits, including reducing the risk of cancer, heart disease, and osteoporosis. These diets emphasize nutrient-rich foods while limiting unhealthy fats, red meat, and sodium intake.
In general, recommendations for nutrition and aging include consuming an antioxidant-rich diet, healthy fats, and limiting the intake of fried, roasted, or charcoal-grilled foods, as well as foods with a high glycemic index. It's also important to moderate alcohol intake and stay hydrated by drinking plenty of water.
Speakers: Dr Steven T. Chen (Boston, USA), Dr Benjamin Kaffenberger (Columbus, USA), Dr Jesse J. Keller (Portland, USA), Dr Kalyani Marathe (Cincinnati, USA), and Dr Robert Micheletti (Philadelphia, USA).
Report written by Dr. Joël Claveau
This highly instructive session was split into 30-minute segments dealing more specifically with the different cases that we may come across in dermatological consultations with hospitalised patients.
Robert Micheletti, MD, FAAD
The first section dealt with vasculitis and was presented by Dr Robert Micheletti, one of the world’s leading experts in the field.
He defines this pathology as the inflammation and subsequent destruction of vessels, resulting in tissue damage.
He explained that when small vessels are affected, either palpable purpura, urticarial papules, vesicles or petechiae appear. Medium-sized vessels cause livedo reticularis, retiform purpura, subcutaneous nodules, ulcers or digital necrosis. This means that a simple skin examination can provide a much more accurate diagnosis.
The conference then focused more on small vessel vasculitis. Lesions are found primarily on the lower limbs and pressure points.
Investigations should include a biopsy of a fresh lesion (1 to 2 days old) and an immunofluorescence exam to try to clarify the aetiology and the possibility of internal organ involvement.
Clinical-pathological correlation is therefore essential in order to make a diagnosis. The causal factor is found in only half of cases, and includes infections, medication, autoimmune diseases and cancers. A full system review is very important to identify damage to internal organs and target further investigations where necessary. For example, we need to look for constitutional symptoms, sinusitis, cough, abdominal pain, joint pain, haematuria and paraesthesia.
If this review is negative, as a minimum, we should request a complete blood count and urinalysis with microscopy. It is important that we are able to identify the presence of glomerulopathy, which is often asymptomatic and which can develop up to 6 months after the cutaneous involvement. Treatment is required if the episode is not limited and lasts more than a few weeks. There is little evidence when it comes to choosing treatment, and options include dapsone and azathioprine.
Kalyani Marathe, MD, MPH, FAAD
The second part tackled a number of different clinical cases that may be encountered in paediatric dermatology in hospital.
The first case presented was “urticaria multiforme”, which is often misdiagnosed as erythema multiforme. It has transient, well-defined plaques secondary to infection or antibiotics. When this reaction is associated with joint pain, it is called a serum sickness reaction. Treatment includes antihistamines and prednisone if the joints are affected.
The next case discussed was toxic shock secondary to the exfoliative toxins of Staphylococcus aureus. It is most often seen before the age of 5, as the kidneys are immature and therefore unable to evacuate the toxin. Treatment consists of antibiotics such as cephalosporins and clindamycin in addition to nutritional support.
Next came RIME or “Reactive infectious mucocutaneous eruption”. This disorder has now been clearly demonstrated to be distinct from Steven-Johnson syndrome. Initially associated with Mycoplasma pneumoniae, we now know that several other infections can precipitate it. It has a greater effect on the mucosa than the skin. Treatment includes antibiotics, steroids, immunoglobulins and nutritional support. These patients may be hospitalised if there is ocular involvement or systemic symptoms, or if it affects an extensive surface area.
The last two disorders presented are both caused by the coxsackie virus: eczema coxsackieum and hand-foot-and-mouth syndrome. They usually take the form of round papules or very well-defined papulovesicles. This characteristic distribution is the key to diagnosis. While patients may well develop significant bullae and erosions, their general condition remains excellent.
Jesse J. Keller, MD, FAAD
The final section dealt with the diagnosis and treatment of ulcers in hospital.
The speaker began by describing the differential diagnosis of ulcers, which includes diabetic, arterial, infectious, venous, neutrophilic and occlusive microvascular ulcers.
Diabetic ulcers are more common on the soles of the feet of diabetic patients.
Acute arterial ulcers are often found on the toes, together with pain and a decrease in the peripheral pulse.
Infectious or inoculation ulcers are focal, often in the context of trauma, and associated with a purulent-looking scab.
Venous ulcers are usually poorly defined and located around the malleoli, more often internally. The surrounding skin shows signs of venous insufficiency, such as lipodermatosclerosis.
The prototype of neutrophilic ulcers is pyoderma gangrenosum. It is a painful, rapid and progressive ulceration. The edges are undermined and purplish. Pathergy is observed where skin trauma causes lesions to develop.
Once healed, the lesion gives way to a cribriform atrophic scar. Treatment is multidisciplinary and includes wound care, analgesia and controlling the inflammation with immunosuppressive agents such as steroids, cyclosporine or TNF inhibitors.
Finally, the prototype of occlusive ulcers is calciphylaxis. They are most often found in fatty areas such as the abdomen, sides, thighs and acral areas. They are reticulated plaques which progress to retiform purpura and necrotic ulcerated bedsores. The pain is severe and persistent. Management includes discontinuation of causative drugs such as warfarin, vitamin D, calcium, steroids and iron. PTH levels also need to be reduced with Cinacalcet®, for example. Intravenous or intralesional sodium thiosulphate is the most widely recognised treatment.
Speakers: Dr Kathleen Cook-Suozzi (New Haven, US), Dr Ashley Wysong (Los Angeles, US), Dr Mariam Totonchy (Seattle, US)
Report written by Dr. Joël Claveau
This highly informative session was divided into three 20-minute segments and impressively covered all aspects of the management of high-risk squamous cell carcinoma (SCC), from definition, diagnosis and staging to further investigations and treatment. At the same time, the objectives were to adequately stage high-risk SCC and establish a more accurate prognosis, determine indications and methods of imaging, and consider different surgical and non-surgical treatment options as part of a multidisciplinary approach.
By way of introduction, the diagnosis of more than 1 million cases of SCC per year in the United States was mentioned. Although the majority of cases are low-risk cases that can be treated with surgery alone, there remains a good proportion of cases at high risk of local recurrence and metastases. The National Comprehensive Cancer Network (NCCN) and Brigham and Women’s Hospital (BWH) high-risk criteria have been revised. The NCCN criteria now include tumours measuring more than 2 cm (trunk and limbs), those with a special location regardless of size (head, neck, hands, feet, anogenital region), and recurrent, ill-defined tumours with a depth of invasion of more than 2 mm and with a poorly differentiated histology and lymphovascular or perineural invasion.
In terms of the BWH criteria, the risk factors we have identified are tumour size equal to or greater than 2 cm, the presence of perineural invasion (PNI > 0.1 mm), invasion under fat, invasion of bone, and poor histological differentiation. The criteria from 0 to 4 are added together (T1: 0 criteria, T2a: 1 criterion, T2b: 2 or 3 criteria, T3: 4 or more criteria). A study in the NEJM by Wysong et al. (2023) cited during the presentation mentioned that of all the high-risk factors listed above, a depth of more than 2 mm and perineural/lymphovascular invasion are the factors that confer the greatest risk of local or distant recurrence.
The second part focused on an emerging concept in dermatological oncology, i.e. gene expression analysis. The literature on the subject currently refers to a series of 40 genes that can be used to assess the risk of metastasis in high-risk head and neck SCC. Specific mention was made of the study by Arron et al. (2022) on this subject, which succeeded in identifying three different groups of tumours with regard to the risk of metastasis-free survival. Group 1 conferred a low biological risk of less than half the risk of the study population. In comparison, Group 2A conferred a moderate biological risk (similar to standard clinico-pathological factors) and Group 2B a high biological risk. In terms of prognosis, metastasis-free survival at three years was assessed at 91% for Group 1, 80% for Group 2A and 44% for Group 2B. To summarise, the speaker mentioned the use of gene expression analysis for Stage T2B/T3 tumours (BWH), T3/T4 tumours (AJCC), recurrent tumours, and immunocompromised patients. These tests remain expensive and their exact role in everyday practice remains to be defined.
The next section looked at the role of imaging. It was stated at the outset that the main purposes of imaging in cases of cutaneous carcinoma are to assess bone or orbital invasion, evaluate soft tissue extension, stage lymph node or metastatic disease, assess the potential for perineural growth (tumour with invasion of medium-sized or large nerves) and carry out post-operative monitoring. The specific features of each approach were then detailed. Firstly, ultrasound is non-invasive and can be used to image the primary tumour and lymph nodes. In addition, contrast-enhanced computed tomography (CT) is the imaging method of choice for assessing advanced tumours. In most cases, it achieves visualisation superior to that with magnetic resonance imaging (MRI) and is excellent for assessing bone and lymph node involvement. It is a good choice for the initial assessment of lesion size and depth. MRI with gadolinium injection offers superior soft tissue contrast. It is therefore a better method for assessing perineural invasion and bone metastases limited to marrow. The indications for imaging to look for perineural invasion are clinical suggestion of this phenomenon (pain, anaesthesia, paresthesia, etc.), a large tumour with distribution opposite a nerve root, and histopathological evidence of this involvement. Several studies have shown that nearly 80% of cases of perineural invasion were initially missed on imaging. Radiologists must therefore be highly suspicious. Two studies on the importance of imaging were presented. They showed that 65% of imaging tests for advanced SCC (BWH T2B or T3) were abnormal and that this modified management in more than 30% of cases. Lastly, on the subject of monitoring, 75% of recurrences occur within the first two years. A CT scan should therefore be performed every six months, alternating with an ultrasound scan every three months, or else an ultrasound scan should simply be performed every three months for a total of two years in all cases.
The last part dealt with the treatment of these tumours. As far as surgery is concerned, negative margin excision is the key. The Mohs procedure therefore remains the gold-standard treatment, since 100% of the margins are examined. Studies clearly demonstrate the lower risk of metastasis and recurrence with this technique. In comparison, studies using radiotherapy for positive resection margins are unconvincing, with a recurrence rate of over 80% within two years. However, radiotherapy remains an important method in cases of extensive perineural extension, unresectable disease, regional recurrence, or metastatic disease such as in the parotid gland. Indications for post-operative radiotherapy include lymph node disease and large tumours with significant nerve invasion. Therefore, except in rare cases, radiotherapy as primary treatment is not recommended, but it can be a very important form of adjuvant therapy in certain clinical contexts. The last method discussed was immunotherapy.
The two compounds accepted for advanced or metastatic SCC are cemiplimab and pembrolizumab, both PD-1 inhibitors. Their response rates are 47% and 34% respectively. Side effects include fatigue, skin rashes, gastrointestinal effects, pruritus, and immune effects. A study recently published in the NEJM showed encouraging preliminary results for use as neoadjuvant therapy for Stages II to IV. Lastly, options for preventing SCC include nicotinamide (30% reduction in occurrence at 12 months), acitretin (50% reduction in occurrence at 24 months), and topical field treatments for extensive actinic keratosis such as 5-FU, omiquimod and photodynamic therapy.
Speakers: Dr Aimilios Lallas, Prof Joseph Malvehy (Barcelona, Spain), Dr Sebastian Podlipnik (Barcelona, Spain), Dr John Paoli (Gothenburg, Sweden), Dr Bengü Nisa Akay (Ankara, Turkey), Dr Susana Puig (Barcelona, Spain)
Report written by Dr Joël Claveau
In the first session, Dr Lallas reminded us of the importance of the 7 rules to avoid missing melanoma:
In the second session, Prof Joseph Malvehy spoke about a very difficult subject: the early diagnosis of melanoma on the scalp. Here are some tips:
In the following session, Dr Sebastian Podlipnik presented his tips for diagnosing facial melanoma:
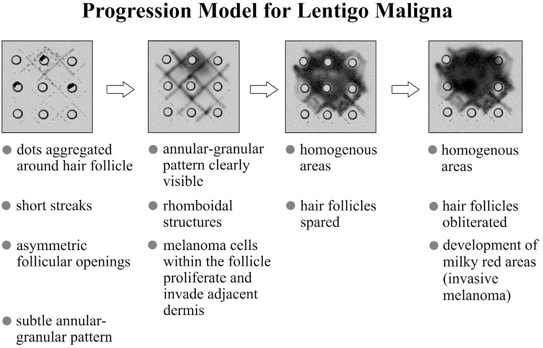
Progression model for lentigo maligna, adopted with permission from Stolz et al.1
Clinics in Dermatology - 2002;20:276-278
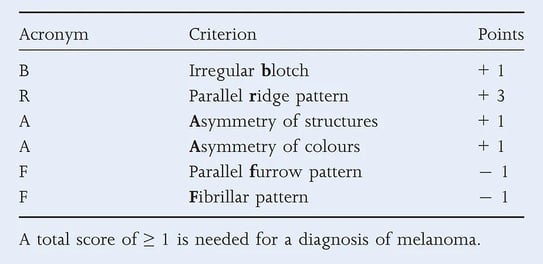
In the fourth conference, Dr. John Paoli summarised some important criteria for accurately recognising acral melanoma:
British Journal of Dermatology (2015) 173, pp1041-1049
Next, Dr Bengü Nisa Akay gave us some rules to avoid missing nail melanoma:
Lastly, in the final lecture on mucosal melanoma, Dr Susan Puig gave us the following rules:
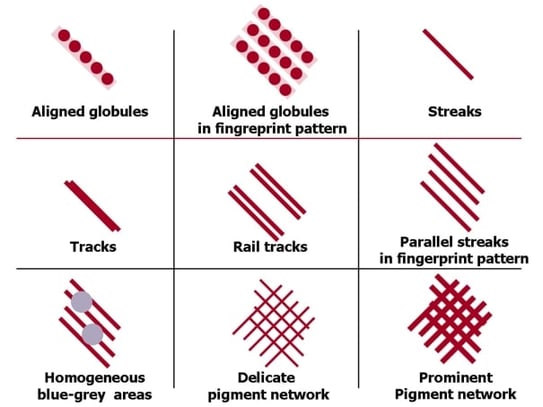
Patterns observed in dermoscopy of mucous membranes
Dermoscopy of pigmented oral lesions, Olga Warszawik et al.
J Dermatol Case Rep. 2008 Oct 11; 2(3): 43–48.


BIODERMA Congress Reports AAD 2023


BIODERMA Congress Reports AAD 2022


Bioderma Congress Reports JDP 2023